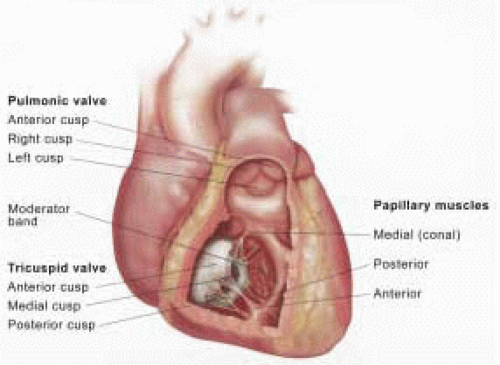
TRANSESOPHAGEAL ECHOCARDIOGRAPHIC EVALUATION OF THE TRICUSPID AND PULMONIC VALVES
Two-Dimensional and Color Flow Doppler
A complete evaluation of the right-sided valves includes standard two-dimensional (2-D) views, CFD, and spectral Doppler examination of the right-sided chambers, the TV, the PV, and their supporting structures, the vena cavae, the hepatic veins, and the proximal main pulmonary artery (PA). TEE may prove less effective in visualizing the TV and PV compared to the MV and AV due to the anterior location of the right-sided valves. Examination of the TV may be especially difficult in the presence of a calcified or prosthetic mitral annulus, or thickened atrial septum. Furthermore, visualization of all three leaflets of the PV is difficult with either TTE or TEE.
The Society of Cardiovascular Anesthesiologists, in collaborative effort with the American Society of Echocardiography (SCA/ASE), has recently published TEE practice guidelines detailing standard imaging planes useful for evaluating the TV and the PV (
7). The relevant views for examination of the right heart, the TV and the PV are listed in
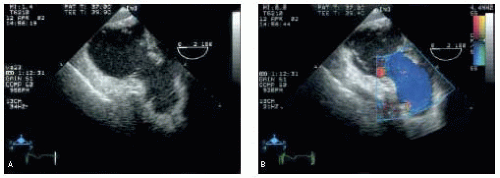
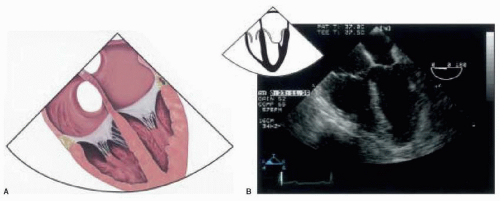
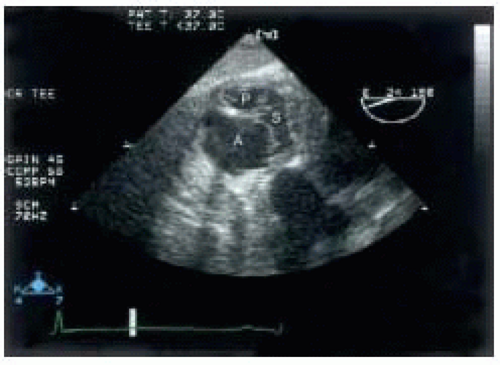
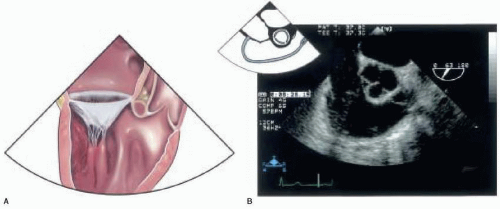
Table 16.1. The midesophageal four-chamber (ME 4-C) view is the starting point for assessing the right-sided valves and provides a good view of the TV. In this view, the atria and ventricles, the atrioventricular valves, and the atrial and ventricular septa are well seen. The TV septal leaflet is displayed to the right of the screen, with either the anterior or posterior leaflets to the left, depending on the degree of TEE probe retroflexion (
Figs. 16.3A and
16.3B). It may be necessary to advance the probe slightly to optimize this view if the valve is obscured by a calcified or prosthetic AV. Anatomic abnormalities of the TV are easily seen, as well as the relative sizes of the right atrium and ventricle that may result from TV pathology. Color flow Doppler examination of the TV allows assessment of tricuspid regurgitation (TR). The valve should be interrogated throughout its superior-to-inferior
aspect and across its transverse dimension (0, 30, and 60 degrees) to completely map the TR jet and determine the severity of regurgitation. Spectral Doppler examination of the valve may be attempted in this imaging plane, but the angle of interception between the direction of flow and the ultrasound beam may preclude an accurate result. The PV is not visualized in the ME 4-C view.
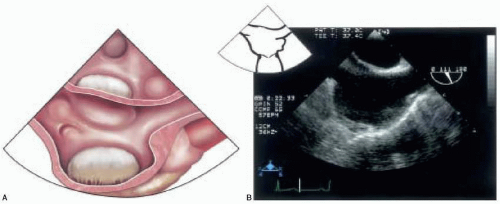
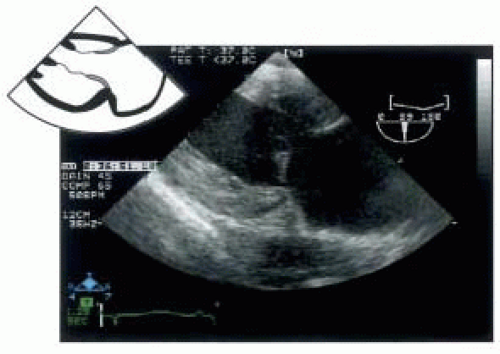
At the same midesophageal level, advancement of the transducer multiplane angle to between 60 and 90 degrees will display the midesophageal RV inflow-outflow view. In this view, the posterior leaflet of the TV will appear to the left side of the screen display and the anterior leaflet to the right. In the far right field, the PV is visible, separating the proximal PA and right ventricular outflow
tract (RVOT) (
Figs. 16.4A and
16.4B). Rotation of the probe to the left (counterclockwise) may improve the image of the proximal main PA allowing evaluation of its first few centimeters for abnormalities. Of note, although the PV leaflets may not be clearly imaged in this view, CFD may still be used to detect pulmonic regurgitation (PR).
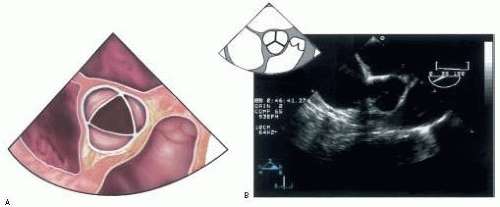
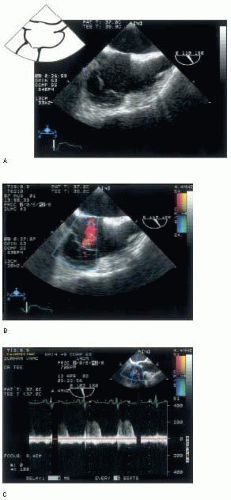
A third imaging plane for examining RV inflow can be acquired beginning with the midesophageal bicaval view (110-140 degrees of transducer rotation) (
Figs. 16.5A and
16.5B) and applying slight counterclockwise probe rotation. The Eustachian valve is often well seen on the left side of the display. In this modified bicaval view, the basal RV and portions of the TV appear in the left far field and allow evaluation of TV inflow and regurgitation (
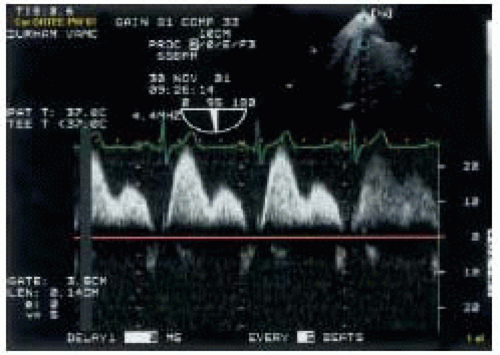
Figs. 16.6A and
16.6B). In addition, the direction of blood flow and the ultrasound beam vector are closely aligned in this view, thereby allowing accurate spectral Doppler assessment of transvalvular flow. Pulsed wave Doppler (PW) analysis of TR peak jet velocity allows estimation of RV and PA systolic pressures (
Fig. 16.6C). Also, the severity of
TV stenosis may be assessed using continuous wave (CW) Doppler techniques.
Imaging of the PV may be augmented with the midesophageal short-axis view of the AV (ME AV SAX). This view is developed at 30-60 degrees of transducer rotation, with the display showing the PV and the main PA to the right of the AV (
Fig. 16.7A). In this scan plane, the right posterior pulmonic leaflet appears posteromedial and the anterior pulmonic leaflet appears more lateral on the display (
Fig. 16.7B) (
8). This is another excellent view in which to inspect the proximal pulmonary artery for pathology.
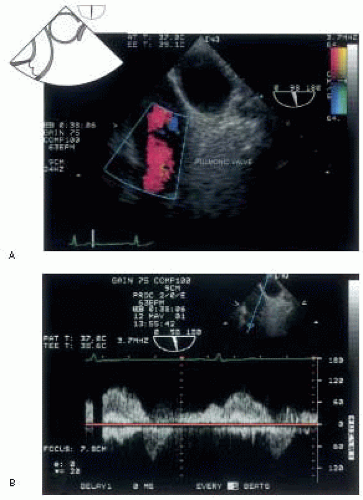
Also useful for PV imaging is the upper esophageal (UE) aortic arch short-axis view (
Fig. 16.8A). In this window, the PA and the PV appear on the left side of the screen, well aligned in long axis with the ultrasound beam vector (
Fig. 16.8Bb). Hence, it is one of the best views for assessing the severity of pulmonic stenosis (PS) and PR. Turning the probe slightly to the left (counterclockwise) and retroflexing may improve the view of the PV. This view provides the best longitudinal assessment of the main PA.
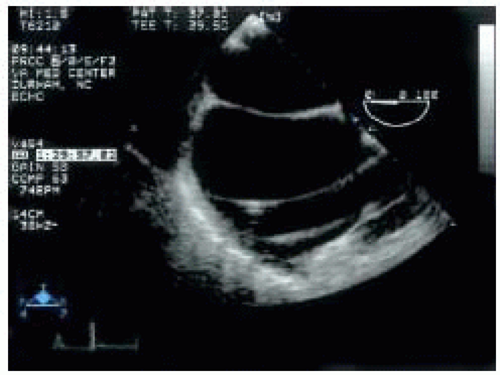
Transgastric (TG) views of the TV are useful, although slightly more difficult to obtain. A short axis of the RV is obtained by visualizing the short axis of the left ventricle and rotating the probe to the right (clockwise). By anteflexing the probe and withdrawing slightly, the three leaflets of the TV come into view, in a manner somewhat analogous to that of the short axis of the leaflets of the mitral valve (
Fig. 16.9). The anterior leaflet appears in the left far field, the posterior in the near left, and the septal to the right of the display. The TG RV inflow view is also developed from the TG midpapillary, short-axis view of the left ventricle by turning the probe slightly rightward (clockwise), centering the RV on the display, and advancing the multiplane angle to between 100 and 120 degrees
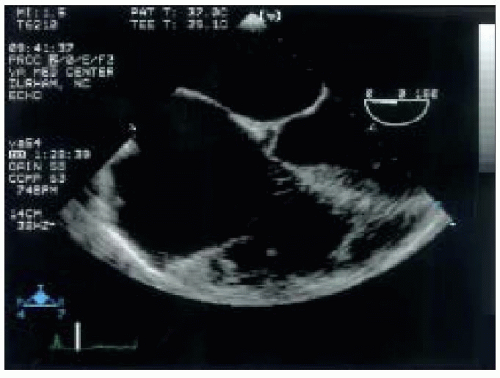
(
Fig. 16.10). This scan plane provides the best view of the TV supporting structures, including the chordae tendinae and papillary muscles. The RV appears on the left, and the RA on the right of the display screen. From this scan plane, the TEE probe can be rotated further rightward (clockwise) to image the hepatic veins, most easily identified with CFD. Pulsed wave Doppler can then be used to evaluate hepatic flow patterns (
Fig. 16.11). The PV and the RVOT can also be imaged from this probe location. From the TG RV inflow view at between 100 and 120 degrees, reducing the multiplane angle slowly toward zero and anteflexing brings the RVOT and the PV into view somewhere between 60 and 90 degrees (TG RV outflow view) (
Fig. 16.12A) (
7). At times, the aortic valve may appear just to the right of the PV, demonstrating the intimate relationship between the two semilunar valves (
Fig. 16.12B).
Finally, further advancing the TEE probe to the deep transgastric position at zero degrees, rightward (clockwise) probe rotation and anteflexion will reveal another view of the RVOT and the PV (
Figs. 16.13A and B). It is important to evaluate the proximal main PA whenever visible, as abnormalities may reflect PV pathology, or be the cause of it.
An additional view, not technically part of TV and PV imaging, is a view of the short axis of the aorta and superior vena cava with the distal portion of the main PA seen to the right of the screen, and the proximal right PA appearing at the top of the screen in long axis. This view is developed from the aortic valve short-axis view by slow withdrawal of the TEE probe until these structures come into view. Often, a pulmonary artery catheter can be seen in both the SVC and the right main PA in this view. The left PA is usually obscured by the bronchial structures.
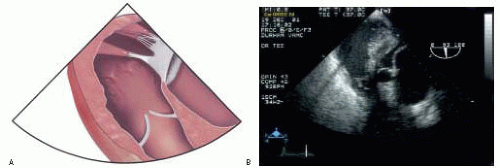
Any of the echocardiographic imaging artifacts may confound evaluation of the TV and the PV. Especially pertinent to imaging of the right-sided structures, however, are pacing wires and intracardiac catheters that may cause acoustic shadowing or be misinterpreted as intracardiac masses, clots, or vegetations (
Fig. 16.14) (
9).
 A) and restriction (E
A) and restriction (E  A) of RV filling. It is important to note that tricuspid inflow patterns have lower absolute
A) of RV filling. It is important to note that tricuspid inflow patterns have lower absolute