Assessment of Right Ventricular Function
Gautam Sreeram
Rebecca A. Schroeder
Jonathan B. Mark
In the past, greater emphasis was placed on descriptive indices of left ventricular function than right ventricular function. In fact, the right ventricle (RV) was often viewed as a simple passive conduit contributing little to overall cardiac performance. More recently, realization of the importance of RV function in maintaining hemodynamic stability has led to a closer examination of the RV.
The asymmetric shape of the RV precludes characterization using simple geometric formulae and complicates assessment of global RV function. Consequently, assessment of RV size and function requires multiple approaches and techniques. Over the past number of years, measurement of RV volume has progressed from simple cross-sectional area planimetry to real-time, three-dimensional echocardiographic renderings of chamber volume (1).
The isovolumic phases of the cardiac cycle are shorter for the RV than for the left ventricle (LV). As a result, while onset of left ventricular contraction normally occurs prior to the onset of right ventricular contraction, RV ejection begins earlier, lasts longer, and has a reduced ejection velocity and a later peak compared with LV ejection. Right ventricular ejection results primarily from inward motion of the RV free wall with smaller contributions from contraction of the RV outflow tract and descent of the base of the heart (2). Right ventricular contraction can be described in terms of movements along major and minor axes, which play an important role in the calculation of some indices of RV function (3).
STRUCTURE AND FUNCTION OF THE RIGHT VENTRICLE
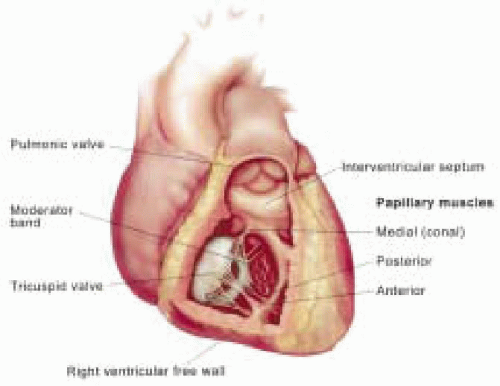
The RV is an asymmetric, complex chamber, which normally appears crescent shaped in short-axis cross section. The RV medial wall is formed by the ventricular septum that it shares with the LV. The RV free wall may be divided into basal, mid, and apical segments corresponding to the adjacent left ventricular segments in the long-axis, four-chamber view. Trabeculae carnae or muscle bundles line most of the inner RV chamber (Fig. 11.1).
Right ventricular anatomy may also be described in terms of its inflow and outflow tracts, which reflect the separate embryologic origins of these portions of the RV. The RV inflow tract begins at the tricuspid valve and is located posteroinferiorly, while the anterosuperiorly positioned RV outflow tract leads to the pulmonic valve and pulmonary artery. An encircling muscular ring separates the inflow and outflow portions of the RV and is composed of four distinct muscular bands: the parietal band, crista supraventricularis, septal band, and moderator band (4). Of these, the moderator band is of considerable importance to the echocardiographer. This structure appears as a prominent muscular trabeculation extending from the lower ventricular septum to the RV free wall, and it must not be mistaken for an abnormal intracardiac mass or thrombus.
The RV has other distinctive anatomic features that distinguish it from the LV. The inflow RV is heavily trabeculated with the trabeculae carneae, while the outflow RV, or infundibulum, is smoother walled. The papillary muscles that support the tricuspid valve via chordae tendineae are more variable in location and size in the RV compared to the mitral valve support structures. The anterior papillary muscle to the tricuspid valve, which arises from the moderator band, is the only papillary muscle commonly identified during routine transesophageal echocardiography (TEE).
TRANSESOPHAGEAL ECHOCARDIOGRAPHIC IMAGING OF THE RIGHT VENTRICLE
Because of its unique geometry, multiple images of the RV are required for accurate structural and functional assessment. The most useful TEE scan planes for RV examination include the midesophageal four-chamber view, midesophageal RV inflow-outflow view, transgastric mid short-axis view, and transgastric RV inflow view.
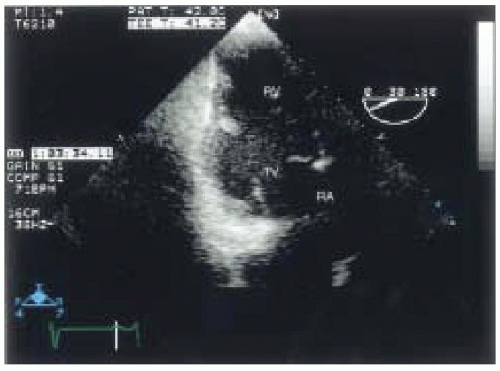
The midesophageal four-chamber view is the single most useful view for assessing overall RV anatomy and global function, and allows evaluation of the apex, mid, and basal segments of this ventricle. In the four-chamber view, the RV appears triangular compared to the elliptical LV and its length extends to only two-thirds of the length of the LV. As a result, the LV, not the RV, normally forms the cardiac apex (Fig. 11.2).
The midesophageal RV inflow-outflow view is sometimes termed the “wrap-around view,” because the right atrium (RA), RV, and pulmonary artery (PA) appear to encircle the aortic valve and left atrium, circumscribing a 180° to 270° arc (Fig. 11.3). This view is particularly helpful for assessing motion of the RV free wall.
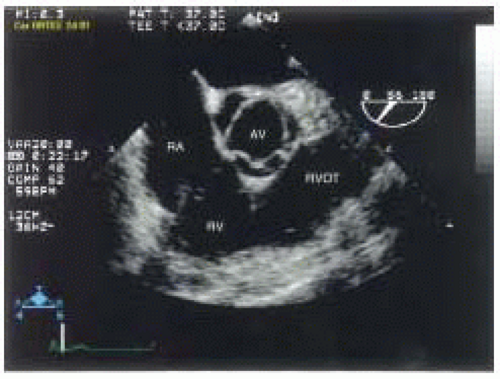 FIGURE 11.2. Midesophageal four-chamber view of the right ventricle (RV), left ventricle (LV), right atrium, and left atrium. |
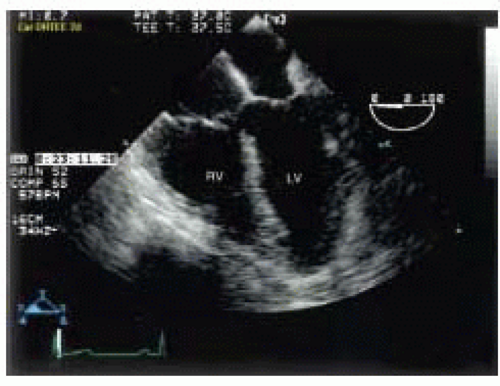 FIGURE 11.3. Midesophageal right ventricular inflow-outflow view with right atrium (RA), right ventricle (RV), right-ventricular outflow tract (RVOT), and aortic valve (AV) labeled. |
The transgastric mid short-axis view may be obtained in the horizontal scan plane with the TEE probe inserted approximately 35-40 cm from the incisors, with the tip flexed to achieve a true short-axis view. Slight clockwise (rightward) probe rotation will center the RV in the image screen. While this view is used most often to monitor LV function, it also allows assessment of the RV free wall and ventricular septum (Fig. 11.4).
Finally, the transgastric RV inflow view provides a long-axis view of the RV similar to the transgastric two-chamber view of the LV. To acquire this view, begin with the transgastric mid short-axis view of the RV (described above) and advance the multiplane angle to approximately 90° or
until the RA and RV are seen in long axis, with the RV inflow and tricuspid valve centered in the image. Alternatively, one develops the transgastric two-chamber view of the left atrium and ventricle and then rotates the probe clockwise (rightward) until the two right-sided chambers are displayed. Both techniques allow one to obtain the same image of the RV inflow tract and the long axis of the right atrium and ventricle (Fig. 11.5).
until the RA and RV are seen in long axis, with the RV inflow and tricuspid valve centered in the image. Alternatively, one develops the transgastric two-chamber view of the left atrium and ventricle and then rotates the probe clockwise (rightward) until the two right-sided chambers are displayed. Both techniques allow one to obtain the same image of the RV inflow tract and the long axis of the right atrium and ventricle (Fig. 11.5).
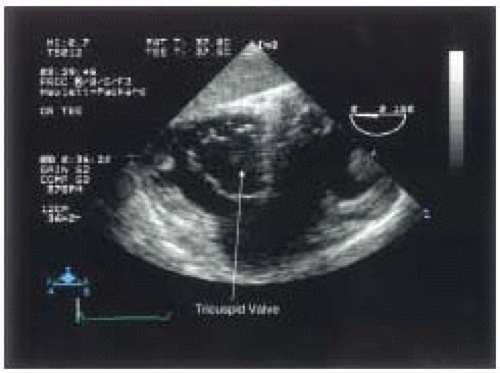 FIGURE 11.4. Transgastric mid short-axis view of right ventricle with tricuspid valve seen in cross-section. |
Other TEE views may be used to supplement these four standard views in patients who have abnormal RV anatomy and function. The midesophageal long-axis view includes a portion of the RV outflow tract, and often the pulmonic valve can be seen anterior to the aortic valve (Fig. 11.6). The transgastric RV outflow view provides an image with many of the same structures seen in the midesophageal RV inflow-outflow view, including the RA, RV, PA, and both tricuspid and pulmonic valves (Figs. 11.7a and 11.7b). Not only used for anatomic imaging, this view allows calculation of cardiac output from measurements of the RV outflow tract dimensions and the corresponding blood flow velocity. This view is acquired beginning with the transgastric mid short-axis view, advancing the multiplane angle to approximately 110-140°, and with slight clockwise (rightward) rotation of the TEE probe. Finally, the deep transgastric RV apical view provides an image similar to the deep transgastric long-axis view, but focused instead on the RV, tricuspid valve, and RA (Fig. 11.8). This view is acquired by slight clockwise (rightward) rotation of the probe from the deep transgastric long-axis view.
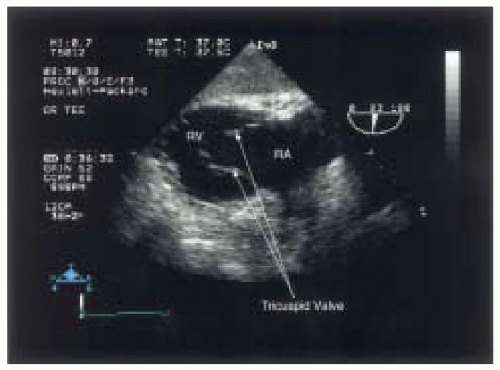 FIGURE 11.5. Transgastric RV inflow view with tricuspid valve leaflets clearly seen in open position. |
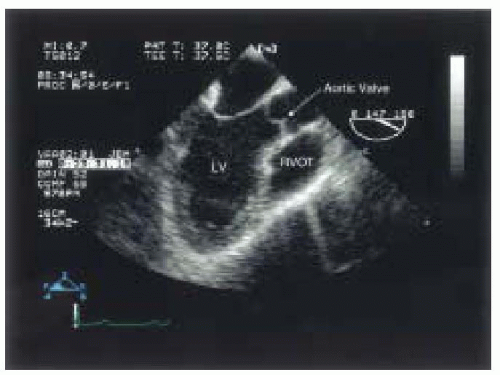 FIGURE 11.6. Midesophageal long-axis view of the left ventricle (LV), with the right ventricular outflow tract (RVOT) visible to the right side. |
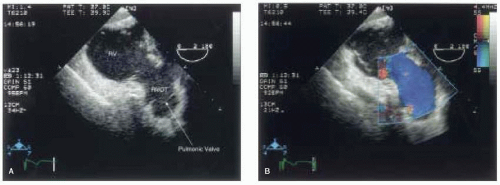 FIGURE 11.7. Transgastric right ventricular outflow view with the pulmonic valve visible in the far field, without (A) and with (B) color-flow Doppler. |
RIGHT VENTRICULAR GLOBAL SYSTOLIC FUNCTION—QUANTITATIVE ECHOCARDIOGRAPHIC ASSESSMENT
Assessment of global right ventricular function includes measurements of RV volume and ejection fraction. Because of the irregular shape of the RV, acquisition of multiple images may be necessary to fully define chamber size and shape. A number of quantitative techniques have been described to measure RV volume and function. First, maximal short-axis and mid short-axis measurements of RV chamber size can be made in a single-plane with normal measurements being 3.5+/−0.2 cm and 2.8+/−0.2 cm, respectively (Fig. 11.9) (3). Second, application of the multiplane method or modified Simpson’s rule can be used to determine RV volume (5). Third, investigators have estimated RV volume from summation of smaller geometric volumes using models of an ellipsoid, a prism, and a pyramid (6,7,8). Fourth, right ventricular end-diastolic and end-systolic measurements can be measured by planimetry, and a fractional area change (FAC) ejection fraction calculated where FAC = [(end-diastolic area − end-systolic area)/end-diastolic area] × 100 (9). Fifth, echocardiographic automated border detection allows measurements of the right ventricular cavity area, and the derived end-systolic pressure area and volume relations may be used to assess RV function (10). Finally, three-dimensional echocardiography is being used to determine if more accurate, repeatable estimates of cardiac size can be obtained when compared to conventional two-dimensional imaging (1,11). Given the complexity and potential inaccuracies in all of these methods, quantitative assessment of RV volume is rarely performed in clinical TEE practice.
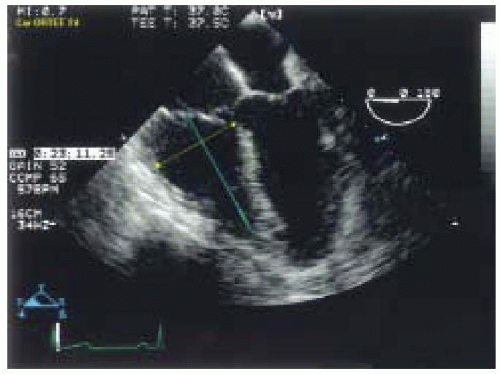 FIGURE 11.9. Measurement of RV chamber size: maximal short-axis (yellow) and mid short-axis (blue) distances measured perpendicular to the long axis of the right ventricle (green).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|