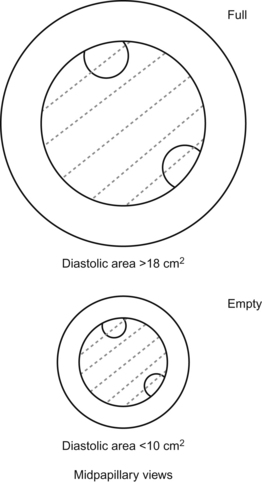
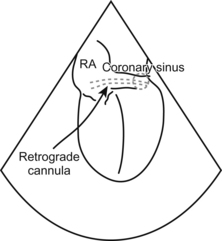
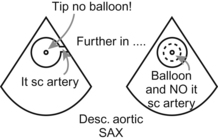
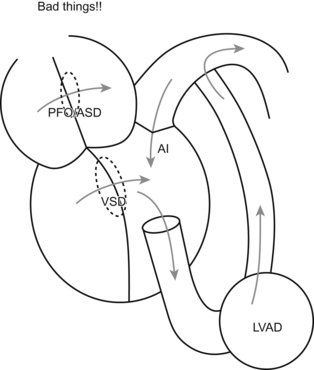
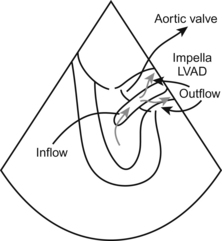
Chapter 16 Assessment of Perioperative Events and Problems Ricardo Martinez-Ruiz and Christopher J. Gallagher The TEE is the anticrash weapon of choice. The TEE gives you the real picture, right now, no need for a leap of faith. 1. End-diastolic area decreased, ventricle contracting OK—You’re low on volume. The heart is empty, so fill it. 2. End-diastolic area increased, ventricle contracting poorly—You have a bad and already overfilled ventricle. Fix whatever’s causing the global hypokinesis (Get a blood gas! Don’t forget the basic stuff!), and once you’ve fixed what you can fix, it’s time for inotropes or ventricular support of some kind. 3. End-diastolic volume normal or low, ventricle contracting well or hyperdynamic—You have a problem with the volume not “going where it’s supposed to go”. Either the volume is all going out into a vastly dilated circulatory tree (anaphylaxis with low systemic vascular resistance), or else some other channel is misrouting your good cardiac output (severe mitral regurg or aortic regurg, or a ventricular septal defect). Assessment of Bypass and Cardioplegia Let’s stretch a little and try to figure this one out. To see the coronary sinus on TEE, you need to get your ME 4-chamber view and slowly advance the probe into the stomach and VOILA!!! The coronary sinus shows up as a drak conduit that drains into the right atrium (you can check with Doppler to see the coronary sinus blood flow). Ocassionally you may have a valve (Thebesian valve) impeding the easy positioning of the retrograde cannula, the cannula gets stuck on it. It is pretty cool to tell your surgeon that the reason he is struggling getting it in position is because of the valve. The tip of your dual stage cannula should be just into the IVC. It’s not a stretch to look for correct placement of an intra-aortic balloon pump. You want to see the tip of the IABP at the takeoff to the left subclavian artery. No higher (occlusion to the left arm) and no lower (inadequate function of the balloon pump and potential occlusion of renal arteries, oops). You should see the tip of the IABP, but no balloon!, at the level of the takeoff of the Lt subclavian artery on the most upper view of the descending thoracic aorta. As soon as you push the probe deeper, the balloon should be visible with its characteristic up and down, up and down… (you can also assess the quality of expansion of the balloon). Things can get more exotic, of course. Once the LVAD is going, you can also use the TEE to confirm that the aortic valve isn’t opening. At first that concept seems a little jarring.
Hypotension and Causes of Cardiovascular Instability
Cardiac Surgery: Techniques and Problems
 Use your TEE to show that the heart is not beating at all—that would mean the cardioplegia is working.
Use your TEE to show that the heart is not beating at all—that would mean the cardioplegia is working.
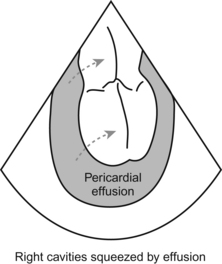
 Use your TEE to see that the heart is not blowing up like a basketball—that would tell you that the cannulae are flowing in the right direction and there is not some catastrophic flow reversal.
Use your TEE to see that the heart is not blowing up like a basketball—that would tell you that the cannulae are flowing in the right direction and there is not some catastrophic flow reversal.
Cannulas and Devices Commonly Used During Cardiac Surgery
What else might Show up During Cardiac Surgery?
Circulatory Assist Devices

Assessment of Perioperative Events and Problems






