Assessment in Off Pump Myocardial Revascularization
Jack S. Shanewise
Over the past several years, there has been a great increase in interest in performing coronary artery bypass graft (CABG) surgery without cardiopulmonary bypass (CPB). Initially in the United States efforts were primarily directed at “minimally invasive” direct coronary artery bypass (MIDCAB), a procedure in which an in situ left internal mammary artery (LIMA) graft is anastomosed to the left anterior descending (LAD) artery through a small left anterior thoracotomy. This procedure was developed to compete with angioplasty for LAD lesions, its proponents emphasizing the decreased cost and time of recovery compared to conventional CABG, usually performing it on younger, healthier patients. However, as time passed, the more widely adopted approach has been to perform CABG surgery on one or more vessels through a full median sternotomy but without CPB, a procedure called off-pump CABG (OPCAB). Its purpose is to provide adequate coronary revascularization while avoiding the morbidity associated with CPB, such as coagulopathy, pulmonary dysfunction, renal insufficiency, and CNS injury. This chapter will discuss how echocardiography can facilitate the management of patients undergoing these procedures.
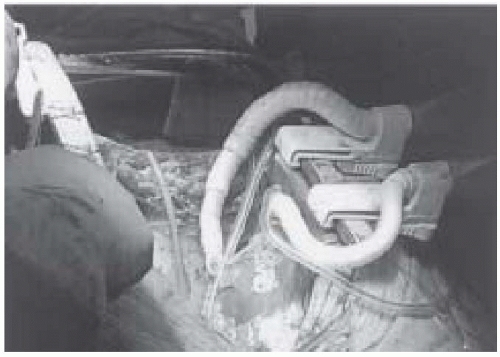
A few surgeons have performed CABG without CPB for many years (1,2,3). But its widespread application of OPCAB occurred with the development of techniques that enable the performance of distal coronary anastomoses on a beating heart. Early on, drugs such as beta antagonists were used to decrease the heart rate and contractility to help provide a quiet surgical field. But more recently, retracting and stabilizing devices have been developed that usually provide an immobile surgical field without the need for pharmacological intervention (Fig. 26.1).
There are several theoretical advantages of performing CABG surgery without CPB compared to conventional CABG. Proponents of OPCAB claim that it costs less than CABG with CPB. While one might think the cost for disposable equipment might be less, in fact, most of the disposable epicardial stabilization devices actually cost more than the disposables needed to put a patient on cardiopulmonary bypass. Costs for personnel are the same because OPCAB is done with a bypass pump and perfusionist standing by. OPCAB would cost less if patients recover more quickly, are extubated sooner, spend less time in the ICU, and are discharged sooner from the hospital than conventional CABG patients. Reports in the literature suggest that this is the case (4,5). The main theoretical advantage of OPCAB, however, is its lack of the untoward effects of CPB, especially in patients with existing impairment of pulmonary, renal, or central nervous system function. OPCAB may be especially beneficial for patients with atherosclerosis of the ascending aorta. Atheroembolism from cannulation and clamping of the ascending aorta for CPB is an important cause of perioperative stroke in these patients (6). With the use of in situ internal mammary artery grafts, OPCAB allows revascularization of the coronaries without touching the aorta. Using a partially occluding aortic clamp (“j” clamp) to construct proximal anastomoses for grafts would largely negate this advantage of OPCAB. There are at least two theoretical disadvantages of OPCAB compared to CABG with CPB. First, the positioning and stabilization of the heart and the occlusion of the coronary arteries required to construct grafts with this technique may cause hemodynamic instability, especially in patients with poor ventricular function. Second, the quality of distal coronary artery anastomoses performed on a beating heart may not be as good as those made with the quiet, clear field provided by CPB, possibly causing a lower rate of graft patency. Reports suggest comparable patency rates for the two techniques in the short term, but it will be some time before long-term patency rates can be compared.
HEMODYNAMIC CONSEQUENCES OF OPCAB
Two features of OPCAB can lead to hemodynamic instability: transient occlusion of coronary arteries during distal anastomosis construction and displacement of the heart to provide access to the distal coronary arteries (7). During OPCAB, the ability of the patient to tolerate occlusion of the artery being grafted is critically dependent on both the severity of the lesion in the artery and the presence of collateral flow into it or from it. For example, grafting of an LAD with a high-grade distal lesion is likely to be well tolerated for two reasons: only a small area of myocardium is supplied by the vessel distal to the obstruction, and collaterals into this region are likely to have developed. On the other hand, occlusion of an LAD with a less severe obstruction may cause hemodynamic instability, especially if this artery supplies collateral flow to another vessel with a high-grade obstruction. Thus, in order to prepare for the likely consequences of coronary occlusion, it is critical to know precisely the severity and location of the coronary lesions, as well as the surgical plan: which vessels will be occluded in what order, including plans for the use of shunts or other means to support the circulation during graft construction. When multiple grafts are to be performed with OPCAB, the order in which they are performed is important. Highly obstructed vessels supplied by collateral flow are usually grafted first to provide flow into more critical vessels before they are grafted. Performing the proximal anastomosis before the distal allows flow to be directed through the graft to the vessel as soon as the distal anastomosis is completed, and can minimize the time a critical portion of myocardium is ischemic during graft construction. To avoid any unnecessary confusion during the operation, the plan should be discussed directly with the surgeon.
Both in clinical practice and in the laboratory, augmenting the preload by volume loading and the headdown position can help maintain cardiac output and perfusion pressure when the heart is displaced (8). TEE is a good means of assessing adequacy of the volume status before displacement for graft construction is attempted (9). Making an incision in the pleura to the right of the heart allows the heart to be elevated without as much compression of the right heart and the vena cava, improving hemodynamic stability. As the heart is positioned, TEE can often provide an indication as to how much compression of the right or left ventricle has occurred. If either chamber is not filling, repositioning of the heart will be necessary. Close observation of the heart with TEE during periods of coronary occlusion may facilitate detection of worsening cardiac function as evidenced by weakening contraction, ventricular dilatation, or increasing mitral or tricuspid regurgitation. Seeing such changes should prompt aggressive interventions to support the circulation or insertion of an intracoronary shunt possibly. On occasion, stopping in the midst of the anastomosis to let the heart down to rest may restore stability to the circulation. Hemodynamic changes are more pronounced with displacement of the heart to access posterior coronary arteries than anterior vessels (10,11).
INTRAOPERATIVE ECHOCARDIOGRAPHY FOR OPCAB
Intraoperative monitoring with transesophageal echocardiography (TEE) during OPCAB is interesting and useful. Information obtained before, during, and after graft construction can be important, and a systematic approach should be used (Table 26.1). A careful and thorough examination is completed and recorded at the beginning of the procedure to establish a baseline for later comparison. Particular attention is placed on documenting LV function and regional wall motion, but it is important to assess right heart function and the valves, as well. Mitral regurgitation (MR) and tricuspid regurgitation (TR) can be dynamic, so their presence and severity are documented at the start of the procedure. Detection of severely impaired cardiac function at this point of the procedure may prompt intervention with drugs or mechanical devices to support the cardiovascular system or even lead to the decision to go on CPB. The aorta is assessed for the presence of atherosclerosis before it is clamped. Epiaortic echocardiography is the best way to detect atherosclerosis in the ascending aorta (12,13) and only takes a few minutes to perform.
Next, TEE can be used to assess the effects of displacement of the heart to gain access to the coronary arteries. With multiplane imaging, the three midesophageal views (four-chamber, two-chamber, and long-axis) allow assessment of all 16 segments of the LV and provide the ability to detect MR with color-flow Doppler, as well as assess right heart function (Fig. 26.2) (14). If the TEE imaging
plane is properly oriented to pass simultaneously through the middle of the MV annulus and the LV apex and held in that position by a clamp, the entire LV may be examined very quickly by just rotating the multiplane angle from zero to 180 degrees. Color-flow Doppler may be activated and the angle decreased back to zero to quickly assess changes in MR, and the RV and TR then examined in the four-chamber view, accomplishing a thorough assessment of the heart in just a few seconds. It is usually not possible to obtain transgastric views of the LV when the heart is displaced for graft construction to the right and circumflex coronary arteries because of loss of contact of the heart with the diaphragm, obscuring the transgastric echocardiographic window. Also, elevation of the heart by placing a lap pad underneath it will obscure the transgastric window. Changes, such as compression of the RV with underfilling of the LV or aggravation of valvular regurgitation, are sought. Placement of the vessel stabilizer may also cause changes in the TEE appearance of the heart, such as compression and underfilling of the LV. Tethering of the myocardium in the region of the stabilizer makes interpretation of wall motion changes more difficult in this area (Fig. 26.3) (15). Once positioning of the heart is completed for grafting, the LV is examined again to establish a baseline for comparison to detect changes during vessel occlusion.
plane is properly oriented to pass simultaneously through the middle of the MV annulus and the LV apex and held in that position by a clamp, the entire LV may be examined very quickly by just rotating the multiplane angle from zero to 180 degrees. Color-flow Doppler may be activated and the angle decreased back to zero to quickly assess changes in MR, and the RV and TR then examined in the four-chamber view, accomplishing a thorough assessment of the heart in just a few seconds. It is usually not possible to obtain transgastric views of the LV when the heart is displaced for graft construction to the right and circumflex coronary arteries because of loss of contact of the heart with the diaphragm, obscuring the transgastric echocardiographic window. Also, elevation of the heart by placing a lap pad underneath it will obscure the transgastric window. Changes, such as compression of the RV with underfilling of the LV or aggravation of valvular regurgitation, are sought. Placement of the vessel stabilizer may also cause changes in the TEE appearance of the heart, such as compression and underfilling of the LV. Tethering of the myocardium in the region of the stabilizer makes interpretation of wall motion changes more difficult in this area (Fig. 26.3) (15). Once positioning of the heart is completed for grafting, the LV is examined again to establish a baseline for comparison to detect changes during vessel occlusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree