Asymptomatic or Mild Angina |
Class I |
1. |
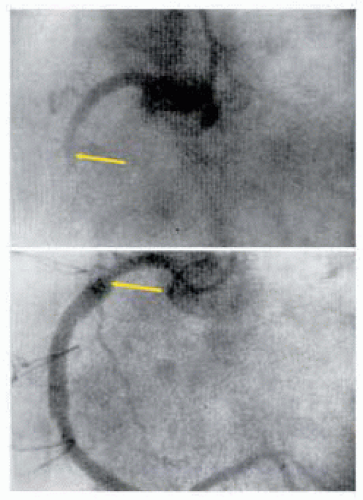
Left main disease (A) |
2. |
Left main equivalent (A) |
3. |
3-vessel disease, EF < 0.50 and/or large ischemic areas (C) |
4. |
Prox LAD Dz + 1-2 vessel Dz + EF < 0.50 +/or large at-risk ischemic area (A) |
Class IIa |
Prox LAD Dz + 1-2-vessel disease (A) |
Class IIb |
1- or 2-vessel Dz + large at-risk viable area (B) |
Stable Angina |
Class I |
1. |
Left main Dz (A) |
2. |
Left main equivalent (A) |
3. |
3-vessel Dz (benefit greater with LVEF < 0.50.) (A) |
4. |
2-vessel Dz with prox LAD stenosis + either EF < 0.50 or ischemia (A) |
5. |
1- or 2-vessel Dz (no prox LAD stenosis) + large at-risk area (B) |
6. |
Disabling angina on max med Rx and acceptable risk (B) |
Class IIa |
1. |
Prox LAD Dz + 1-vessel disease (A) |
2. |
1- or 2-vessel Dz (no prox LAD Dz) mod viable ischemic area at-risk (B) |
Class III (not recommended) |
1. |
1-2 vessel Dz (no prox LAD Dz) symptoms not ischemia, < max med Rx, small ischemia viable area (B) |
2. |
Borderline coronary Dz (50%-60% or left main < 40%) + no ischemia (B) |
3. |
Insignificant coronary Dz (< 50%) (B) |
Unstable Angina (Non-STEMI) |
Class I |
1. |
Left main stenosis (A) |
2. |
Left main equivalent: (> 70% prox LAD + prox LCx)(A) |
3. |
Active ischemia not responsive to med Rx + PCI not possible (B) |
Class IIa |
1. |
Prox LAD Dz with 1- or 2-vessel Dz (A) |
Class IIb |
1- or 2-vessel disease not involving the proximal LAD when PCI not possible/optimal |
Emergent / Urgent CABG STEMI |
Class I |
1. |
Failed PCI + persistent pain or unstable hemodynamics + suitable Sx anatomy (B) |
2. |
Persistent recurrent ischemia on max med Rx and suitable Sx anatomy + significant area at risk + not PCI candidates (B) |
3. |
During surgery for VSD or ischemic MR (B) |
4. |
Cardiogenic shock < 36 hrs of MI (age < 75) + ST elevation, LBBB, posterior MI + suitable Sx anatomy (A) |
5. |
Life-threatening ventricular arrhythmias and left main Dz (> 40%) or equivalent (B) |
Class IIa |
1. |
< 6-12 MI + suitable anatomy not candidates or failed fibrinolysis/PCI (B) |
2. |
CABG mortality elevated (< 3 to 7 days MI); benefit CABG by risk-benefit (B) |
Class III (not recommended) |
1. |
Persistent angina + small area myocardium at-risk and stable hemodynamics (C) |
2. |
Successful epicardial reperfusion + poor microvascular reperfusion (C) |
Poor LV Function |
Class I |
1. |
Left main Dz (B) |
2. |
Left main equivalent (B) |
3. |
Prox LAD Dz + 2- or 3-vessel Dz (B) |
Class IIa |
Significant viable noncontracting revascularizable myocardium (B) |
Class III (not recommended) |
No evidence of ischemia or significant revascularizable viable myocardium (B) |
Life Threatening Ventricular Arrhythmias |
Class I |
1. |
Left main stenosis (B) |
2. |
Left main equivalent (B) |
Class IIa |
1. |
1-2 vessel Dz causing the arrhythmias (B) |
2. |
Prox LAD Dz + 1-2 vessel Dz (B) |
Class III (not recommended) |
1. |
VT with scar + no ischemia (B) |
2. |
CABG after failed PCI |
Class I |
1. |
Ischemia or threatened occlusion with significant at-risk area (B) |
2. |
Hemodynamic compromise (B) |
Class IIa |
1. |
Foreign body crucial anatomic position (C) |
2. |
Unstable hemodynamics + impaired coagulation + no previous sternotomy (C) |
Class IIb |
Unstable hemodynamics + impaired coagulation + previous sternotomy (C) |
Class III |
1. |
Absence of ischemia (C) |
2. |
Inability to revascularize target anatomy or no-reflow state (C) |
Previous CABG |
Class I |
1. |
Disabling angina with max med Rx or atypical angina with ischemia (B) |
2. |
No patent grafts + left main Dz or equivalent (B) |
Class IIa |
1. |
Bypassable distal vessel(s) with large area threatened myocardium (B) |
2. |
Atherosclerotic LAD vein graft (Dz > 50%) or large at risk areas (B) |
Valve Surgery at Time of CABG |
Class I |
Severe AS 1 criteria for AVR (B) |
Class IIa |
1. |
Mod MR correction probably indicated (B) |
2. |
Mod AS acceptable combined risks (B) |
Class IIb |
1. |
Mild AS if acceptable combined risk (C) |
2. |
Arterial conduits |
Class I |
In all CABG, the LAD Dz should considered for left IMA graft (B) |
Transmyocardial revascularization (laser) |
Class IIa |
Angina refractory to Rx 1 not candidates for PCI-CABG (A) |
Classification of Recommendations |
Class I: |
Conditions for which there is evidence and/or general agreement that a procedure is beneficial and effective. |
Class II: |
Conditions for which there is conflicting evidence and/or a divergence of opinion about the usefulness of a procedure or treatment. |
IIa: |
Conflicting evidence but weight of evidence/opinion is in favor of benefit/ efficacy. |
IIb: |
Conflicting evidence and benefit/efficacy is less well established by evidence/opinion. |
Class III: |
Conditions for which there is evidence and/or general agreement that the procedure/ treatment is not useful or effective. |
Level of Evidence |
A: |
Data from multiple randomized trials or metaanalysis |
B: |
Data from single randomized trial or nonrandomized studies |
C: |
Concensus opinion of experts only or standard of care |
Adapted from Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA guidelines for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the 1991 guidelines for coronary artery bypass graft surgery). J Am Coll Cardiol 1993;34:1262-1346. |