Assessment
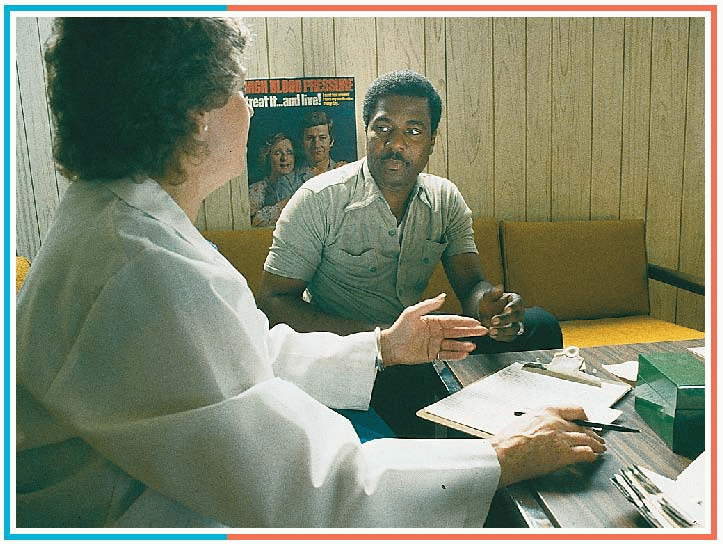
Taking a health history
The first step in assessing the cardiovascular system is to obtain a health history. Begin by introducing yourself and explaining what will occur during the health history and physical examination. Then ask about the patient’s chief complaint. Also, be sure to ask about both the patient’s personal and family health history.
|
|
Common chief complaints
Chest pain
Many patients with cardiovascular problems complain at some point of chest pain. Chest pain can arise suddenly or gradually and can radiate to the arms, neck, jaw, or back. It can be steady or intermittent and mild or acute, and it can range in character from a sharp, shooting sensation to a feeling of heaviness, fullness, or even indigestion. The cause of chest pain may be difficult to determine at first. Chest pain can be provoked or aggravated by stress, anxiety, exertion, deep breathing, or consumption of certain foods.
|
memory board
PQRST: What’s the story?
Use the PQRST mnemonic to fully explore your patient’s chest pain. When you ask the questions below, you’ll encourage him to describe his symptom in greater detail. Remember to streamline your questions according to the patient’s pain severity so that emergency care can be initiated promptly when indicated.
PQRST
Provocative or palliative
What provokes or relieves the chest pain?
What makes the pain worsen or subside?
Quality or quantity
What does the pain feel like?
Are you having the pain right now? If so, is it more or less severe than usual?
To what degree does chest pain affect your normal activities?
Region or radiation
Where in the chest does the pain occur?
Does the pain appear in other regions as well? If so, where?
Severity
How severe is the chest pain? How would you rate it on a scale of 0 to 10, with 10 being the most severe?
Does the pain seem to be diminishing, intensifying, or staying about the same?
Timing
When did the pain begin?
Was the onset sudden or gradual?
How often does the pain occur?
How long does it last?
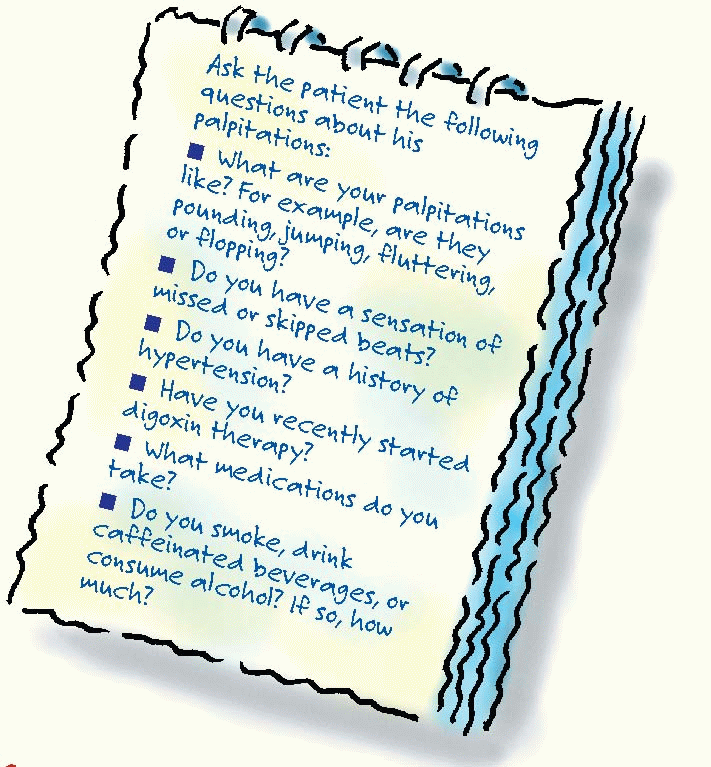
Palpitations
Defined as a conscious awareness of one’s heartbeat, palpitations are usually felt over the precordium or in the throat or neck. Palpitations may be regular or irregular, fast or slow, paroxysmal or sustained. Ask the patient to simulate his rhythm by tapping his finger on a hard surface.
Many palpitations are insignificant. However, they can be caused by such disorders as arrhythmias, hypertension, mitral prolapse, and mitral stenosis.
|
|
|
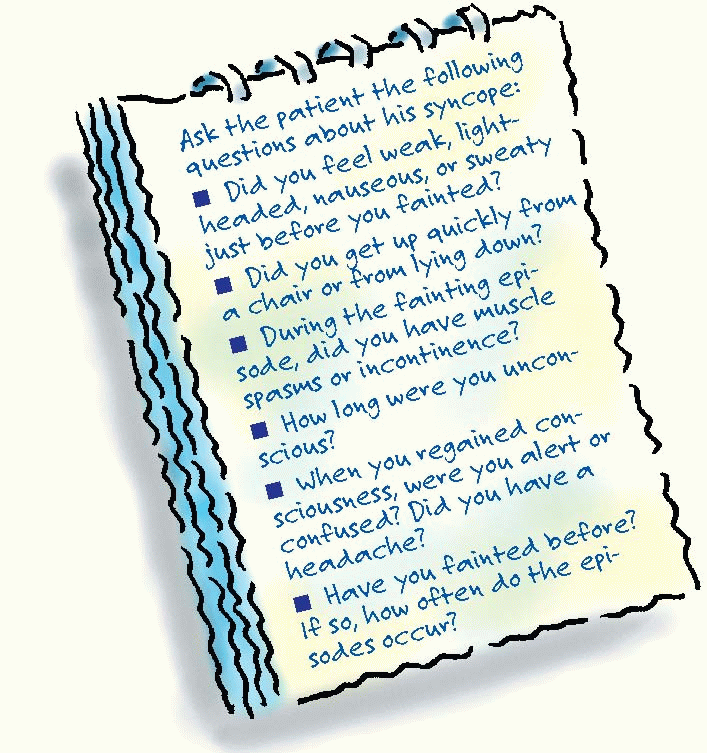
Syncope
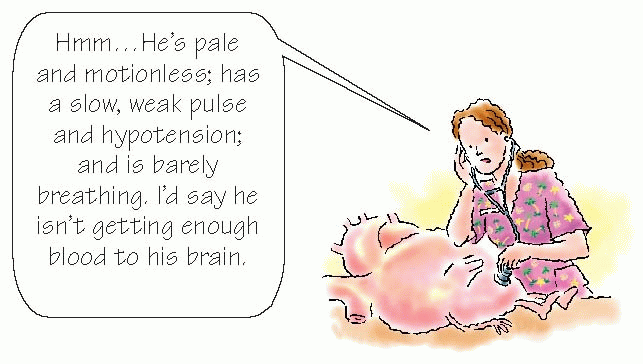
Syncope is a brief loss of consciousness caused by a lack of blood to the brain. It usually occurs abruptly and can last for seconds to minutes. It may result from such disorders as aortic arch syndrome, aortic stenosis, and arrhythmias.
When syncope occurs, the patient typically lies motionless, with his skeletal muscles relaxed. The depth of unconsciousness varies. The patient is strikingly pale with a slow, weak pulse; hypotension; and almost imperceptible breathing.
|
|
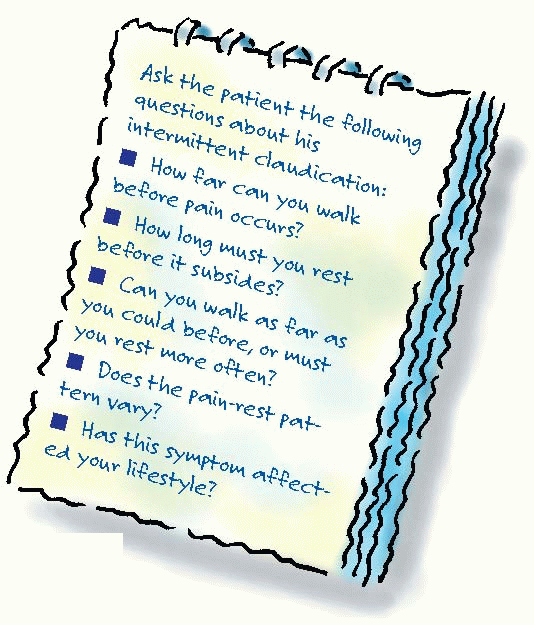
Intermittent claudication
Intermittent claudication is severe cramping limb pain that’s brought on by exercise and relieved by 1 or 2 minutes of rest. It usually occurs in the legs. This pain may be acute or chronic; when acute, it may signal acute arterial occlusion. Intermittent claudication typically results from such disorders as aortic arteriosclerotic occlusive disease, acute arterial occlusion, or arteriosclerosis obliterans.
|
|
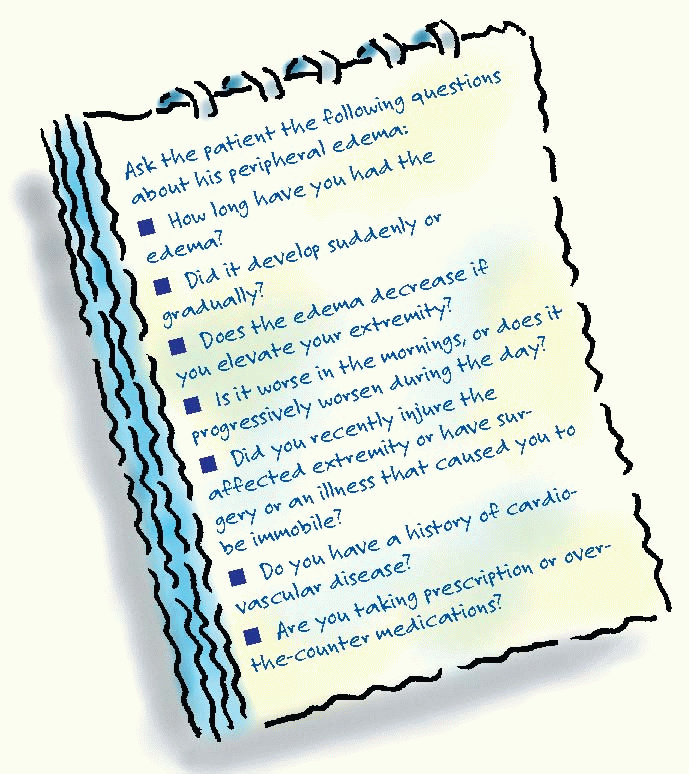
Peripheral edema
Peripheral edema results from excess interstitial fluid in the arms or legs. It may be unilateral or bilateral, slight or dramatic, and pitting or nonpitting. Arm edema may be caused by superior vena cava syndrome or thrombophlebitis. Leg edema may be an early sign of right-sided heart failure, thrombophlebitis, or chronic venous insufficiency.
|
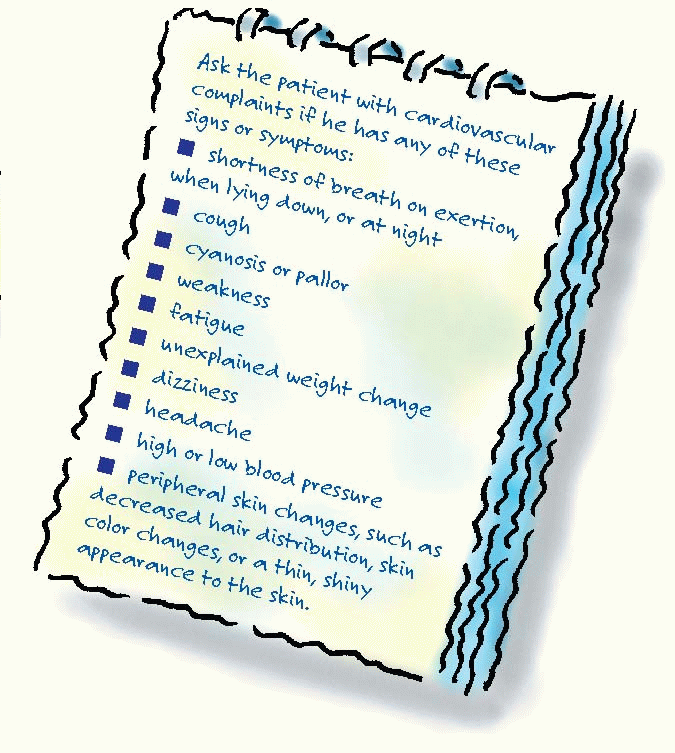
Other signs and symptoms
Ask the patient if he has any other signs or symptoms. Also, inquire about the patient’s family history and past medical history, including history of heart disease, diabetes, or chronic lung, kidney, or liver disease.
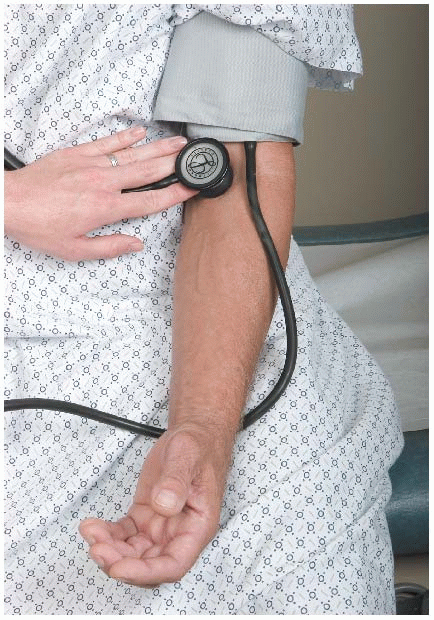
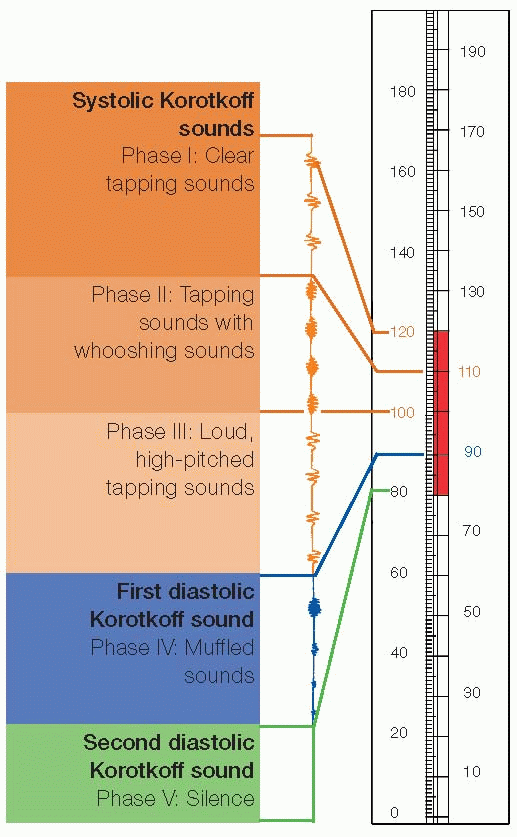
Measuring blood pressure
|
When you take a patient’s blood pressure, you’re measuring the lateral force that blood exerts on the arterial walls as the heart contracts (systolic pressure) and relaxes (diastolic pressure). Use these tips to obtain the most accurate reading:
Use a cuff that’s 20% to 25% wider than the patient’s arm circumference.
Support the patient’s arm at heart level.
Use the bell of the stethoscope.
Deflate the cuff at 2 to 3 mm Hg per second.
Listen for the five phases of Korotkoff sounds.
|
|
|
Performlna cardiac inspection
1 Take a moment to assess the patient’s general appearance. Is he overly thin? Obese? Alert? Anxious? Note his skin color, temperature, turgor, and texture. Are his fingers clubbed? If the patient is dark-skinned, inspect his mucous membranes for pallor.
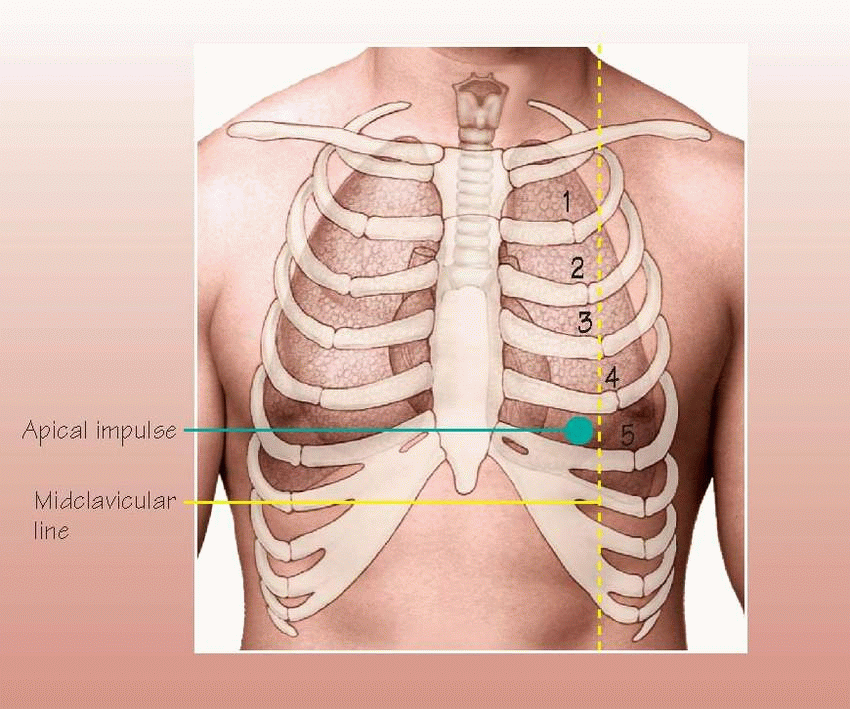
2 Next, inspect the chest. Note landmarks you can use to describe your findings and to identify structures underlying the chest wall. Also look for pulsations, symmetry of movement, retractions, or heaves (a strong outward thrust of the chest wall that occurs during systole).
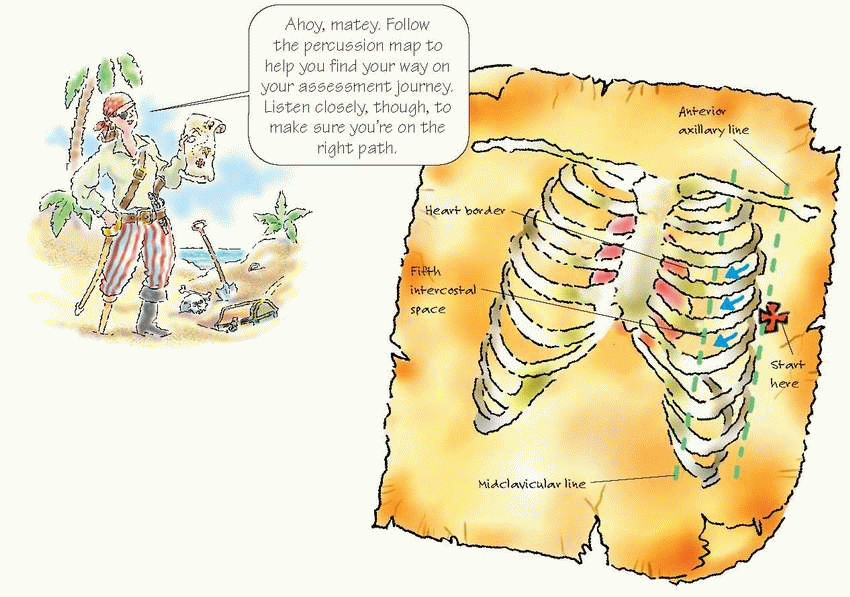
3 Note the location of the apical impulse, including any displacement. You should find it in the fifth intercostal space, medial to the left midclavicular line. It’s usually the point of maximal impulse and can be seen in about 50% of adults. You’ll notice it more easily in children and in patients with thin chest walls. Because the apical impulse corresponds to the apex of the heart, it helps indicate how well the left ventricle is working.
|
|
Performing cardiac palpation and percussion
|
Maintain a gentle touch when you palpate so that you don’t obscure pulsations or similar findings. Using the ball of your hand, then your fingertips, palpate over the precordium to find the apical impulse. Note heaves or thrills (fine vibrations that feel like the purring of a cat).
The apical impulse may be difficult to palpate in an obese or a pregnant patient and in a patient with a thick chest wall. If it’s difficult to palpate with the patient lying on his back, have him lie on his left side or sit upright. It may also be helpful to have the patient exhale completely and hold his breath for a few seconds.
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree