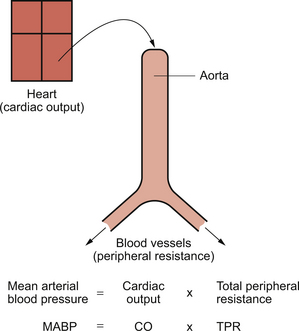
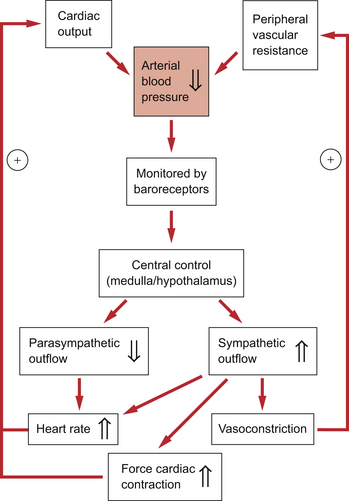
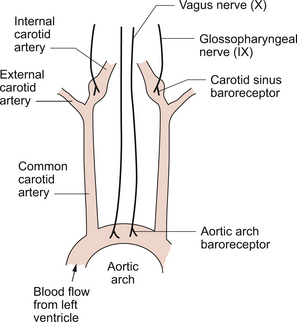
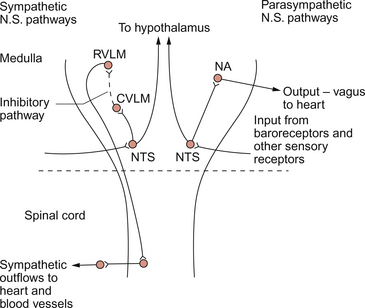
10 A simple model of the arterial circulation is shown in Figure 10.1. Blood pressure can be regulated by changes in either cardiac output or the peripheral resistance. Arterial blood pressure provides the driving force to perfuse the tissues of the body with blood. This driving force is dissipated as blood moves round the circulation and there is a continuous fall in pressure between the arteries and the right atrium (see Fig. 9.1). Mean aortic pressure is typically about 95 mm Hg whereas right atrial pressure is about 0–5 mm Hg. Although the output of the heart is phasic, i.e. blood enters the circulatory system during cardiac systole and this ceases when the heart refills during diastole, circulation of blood around all the tissues of the body is continuous. This is driven by the head of pressure maintained in the arterial tree (see page 86). Blood pressure in the arteries is pulsatile but by the time blood reaches the capillaries, where the important functions of the circulatory system take place, the pressure fluctuations have been damped out (see Fig. 9.1). It is important that arterial pressure is maintained quite constant, as a fall in pressure below a critical level leads to underperfusion of the brain and the subject faints (see Chapter 9). A sustained rise in arterial blood pressure—hypertension—leads to the pathological changes in blood vessels described later in this chapter. Moment to moment fluctuations in arterial blood pressure are minimized by the baroreceptor reflex. This reflex is summarized in Figure 10.2. An outline of a case history of a patient with hypertension is shown in Case 10.1:1. The factors determining cardiac output have been discussed in Chapter 4. The essential features are that the heart has an intrinsic contractile rate which can be modified by the parasympathetic (vagus) nerve to slow the heart or by the sympathetic nerves to increase heart rate. The force of contraction of the heart and, therefore, the stroke volume is determined by a combination of preload effects (blood volume, venous return, venous tone), contractility effects (changes in myocyte [Ca++] produced physiologically by sympathetic nerve stimulation) and afterload effects (mainly opposition to opening the aortic valve produced by the arterial blood pressure). The factors determining peripheral blood vessel resistance to flow have been discussed in Chapter 9. Some of the mechanisms (metabolite, endothelial and local hormone effects) ensure an appropriate distribution of flow within tissues to match the local metabolic activity. Adjustment of the overall resistance to maintain arterial blood pressure at a relatively constant level is achieved by the autonomic nerve supply to peripheral blood vessels. This has the fundamental characteristics that it is sympathetic in origin, using noradrenaline (norepinephrine) as the main neurotransmitter which, acting primarily through α1-receptors, leads to vasoconstriction (see Chapter 9). Although there are parts of the circulation where one or other of these characteristics does not apply, these are very limited and specialized aspects of vascular control and are not major factors determining the total peripheral resistance. The location of the main arterial baroreceptors is shown in Figure 10.3. Information from these two groups of baroreceptors enters the brain at the level of the medulla. The initial processing of information from the baroreceptors occurs in the nucleus tractus solitarius (NTS) in the medulla. The NTS has connections to the regions of the medulla which organize the outflow to the two divisions of the autonomic nervous system. The cell bodies of the preganglionic parasympathetic nerves, which slow heart rate, are located in the nucleus ambiguus and the dorsal motor nucleus. There are also neural connections from the NTS to the rostral ventrolateral medulla, a region of the brainstem controlling the sympathetic outflow to the heart (increases rate) and to the peripheral blood vessels (mainly leading to vasoconstriction). Figure 10.4 summarizes the main pathways in the medulla involved in the control of arterial blood pressure. The cerebellum is involved in the coordination of muscle movement in exercise and is also involved in the circulatory responses to exercise. Aspects of this are discussed in Chapter 13. A flow chart summarizing the baroreceptor reflex for the regulation of arterial blood pressure is shown in Figure 10.2. The responses to a fall in blood pressure are illustrated. The reflex response is an increase in heart rate, an increase in the force of cardiac contraction and an increase in peripheral vasoconstriction, all of which will help to restore blood pressure to normal levels. It has been said that regulation of heart rate is the primary role of the baroreceptor reflex and that responses leading to vasoconstriction and venoconstriction are of secondary importance. Baroreceptor reflex resetting occurs during the long-term rises in blood pressure known as hypertension and also during the changes in blood pressure which occur with increasing age. The site of these adaptive changes is in the central control mechanisms. The changes in baroreceptor function are a consequence of raised blood pressure rather than a primary cause of hypertension. Sensitivity of the baroreceptor mechanism may decrease when there are changes in the arterial wall compliance which sometimes occur as a consequence of atherosclerotic changes (see Chapter 8). Groups of receptors located at the junction of the atria and the great veins effectively monitor blood volume. Approximately two thirds of blood volume is contained in the veins and changes in this volume will alter the stretch in the wall of the veins. This stretch is detected by myelinated vagal afferent nerves. In the control of blood volume this information is supplemented by an input from the arterial baroreceptors and by hormonally mediated changes in kidney function. An increase in blood volume leads to decreased secretion of antidiuretic hormone (ADH) and therefore a diuresis. Concurrently a decrease in renin secretion from the kidney leads to a decrease in aldosterone mediated sodium retention (see Chapter 9
ARTERIAL BLOOD PRESSURE
Introduction
Arterial baroreceptors
Anatomical location of baroreceptors
Central control of the cardiovascular system
The baroreceptor reflex
Cardiopulmonary reflexes
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine