Arterial Blood Gases
Arterial blood gas analysis is performed to answer various clinical questions: Is gas exchange normal? Is there carbon dioxide retention in the patient with chronic obstructive pulmonary disease (COPD), severe asthma, or severe restrictive disease? Is there hypoxemia (low oxygen saturation)? Does the saturation decrease with exercise? What is the acid-base status?
Several important aspects need to be considered for obtaining and handling arterial blood specimens. The laboratory must always indicate on the report form whether the patient was breathing room air or an increased oxygen concentration. As stated in Section 3B (page 29), the arterial oxygen tension may be lower in the supine position than the upright posture. Therefore, the posture of the patient should be noted. The patient should be neither hyperventilating nor holding his or her breath. The specimen should not contain any air bubbles, and it should be quickly iced and promptly analyzed. Similar precautions apply to the analysis of the pH of pleural fluid when empyema is a possibility.
6A. Arterial Oxygen Tension
There are four major steps in the transfer of oxygen from inhaled air to the tissues:
1. Ventilation of the alveoli must be adequate.
2. Within the lung, the inhaled air must come in contact with venous blood; that is, there must be adequate matching of ventilation ( ) to perfusion (
) to perfusion ( ).
).
 ) to perfusion (
) to perfusion ( ).
).3. There must be diffusion of the oxygen through the alveolar wall into the hemoglobin in the red cells (see Chapter 4).
4. Oxygenated hemoglobin must then be transported by the cardiovascular system to the tissues.
The first two steps are discussed in this chapter. Transport, or so-called internal respiration, deals with the oxygen content of blood, the cardiac output, and the distribution of blood flow to the organs, and this topic is outside the province of this book.
The tension of oxygen in the arterial blood (Pao2) reflects the adequacy of the transfer of oxygen from ambient air to blood. In normal young adults, the Pao2 values at sea level range from 85 to 100 mm Hg. The values decrease slightly with age, to about 80 mm Hg at age 70. Hypoxemia exists when the Pao2 is less than these values. The oxygen dissociation curve is useful in
the consideration of hypoxemia. Figure 6-1 shows the average values for the oxygen tension of mixed venous blood (V ˜ = 40 mm Hg, saturation 75%) and arterial blood (a ˜ Pao2 = 100 mm Hg, saturation 96%). The curve is very steep at and below the venous point, where small changes in oxygen tension produce dramatic change in the oxygen content of blood, and hence the saturation. Conversely, at oxygen tensions of more than 60 to 70 mm Hg, large changes in tension have a relatively small effect on saturation. Hence, very little additional oxygen can normally be added to the blood by using very high inspired oxygen tensions. Cyanosis is not easily appreciated until the saturation has decreased to less than 75%.
= 40 mm Hg, saturation 75%) and arterial blood (a ˜ Pao2 = 100 mm Hg, saturation 96%). The curve is very steep at and below the venous point, where small changes in oxygen tension produce dramatic change in the oxygen content of blood, and hence the saturation. Conversely, at oxygen tensions of more than 60 to 70 mm Hg, large changes in tension have a relatively small effect on saturation. Hence, very little additional oxygen can normally be added to the blood by using very high inspired oxygen tensions. Cyanosis is not easily appreciated until the saturation has decreased to less than 75%.
the consideration of hypoxemia. Figure 6-1 shows the average values for the oxygen tension of mixed venous blood (V ˜
 = 40 mm Hg, saturation 75%) and arterial blood (a ˜ Pao2 = 100 mm Hg, saturation 96%). The curve is very steep at and below the venous point, where small changes in oxygen tension produce dramatic change in the oxygen content of blood, and hence the saturation. Conversely, at oxygen tensions of more than 60 to 70 mm Hg, large changes in tension have a relatively small effect on saturation. Hence, very little additional oxygen can normally be added to the blood by using very high inspired oxygen tensions. Cyanosis is not easily appreciated until the saturation has decreased to less than 75%.
= 40 mm Hg, saturation 75%) and arterial blood (a ˜ Pao2 = 100 mm Hg, saturation 96%). The curve is very steep at and below the venous point, where small changes in oxygen tension produce dramatic change in the oxygen content of blood, and hence the saturation. Conversely, at oxygen tensions of more than 60 to 70 mm Hg, large changes in tension have a relatively small effect on saturation. Hence, very little additional oxygen can normally be added to the blood by using very high inspired oxygen tensions. Cyanosis is not easily appreciated until the saturation has decreased to less than 75%.The four common causes of hypoxemia occurring with a normal inspired oxygen tension and barometric pressure are hypoventilation, ventilation-perfusion ( ) mismatch, shunt, and impaired diffusion.
) mismatch, shunt, and impaired diffusion.
 ) mismatch, shunt, and impaired diffusion.
) mismatch, shunt, and impaired diffusion.Hypoventilation
This term refers specifically to alveolar hypoventilation. There are two important, distinguishing features of alveolar hypoventilation. One feature is that arterial carbon dioxide tension (Paco2) is always increased. The following simple equation defines the relationship between Paco2 and alveolar ventilation ( ) and carbon dioxide production by the body (
) and carbon dioxide production by the body ( ) (“k” is a constant):
) (“k” is a constant):
 ) and carbon dioxide production by the body (
) and carbon dioxide production by the body ( ) (“k” is a constant):
) (“k” is a constant):Assume  stays constant. When (
stays constant. When ( ) decreases, Paco2 must increase. Similarly, an increase in
) decreases, Paco2 must increase. Similarly, an increase in  can increase Paco2, unless alveolar ventilation increases proportionately.
can increase Paco2, unless alveolar ventilation increases proportionately.
 stays constant. When (
stays constant. When ( ) decreases, Paco2 must increase. Similarly, an increase in
) decreases, Paco2 must increase. Similarly, an increase in  can increase Paco2, unless alveolar ventilation increases proportionately.
can increase Paco2, unless alveolar ventilation increases proportionately. FIG. 6-1. Oxyhemoglobin dissociation curve for hemoglobin that plots oxygen saturation against the partial pressure of oxygen (Po2) and also the oxygen content (Co2). P50 is the partial pressure of oxygen that results in a 50% saturation of hemoglobin. a, arterial blood; v, mixed venous blood. (From Taylor AE, Rehder K, Hyatt RE, et al., eds. Clinical Respiratory Physiology. Philadelphia, PA: W. B. Saunders, 1989. Used with permission.) |
A way to think of alveolar ventilation is as follows. When a subject inhales a tidal volume breath (designated VT), a certain amount of that breath does not reach the gas-exchanging alveoli. A portion stays in the upper airway, trachea, and bronchi, and a portion may go to alveoli with no perfusion (especially in disease), so that gas exchange does not occur in either case. This fraction of the inhaled VT is referred to as the dead space volume (VD). The Vd is small in normal conditions but increased in diseases such as emphysema and chronic bronchitis. If total ventilation ( E) is defined as the ventilation measured at the mouth, then
E) is defined as the ventilation measured at the mouth, then
 E) is defined as the ventilation measured at the mouth, then
E) is defined as the ventilation measured at the mouth, then
That is, alveolar ventilation is the total ventilation minus the amount ventilating the dead space. Thus,  in Eq. 1 may be reduced by a decrease in
in Eq. 1 may be reduced by a decrease in  or by an increase in VD/VT.
or by an increase in VD/VT.
 in Eq. 1 may be reduced by a decrease in
in Eq. 1 may be reduced by a decrease in  or by an increase in VD/VT.
or by an increase in VD/VT.The second feature is that the hypoxemia due to alveolar hypoventilation can always be corrected by increasing the inspired oxygen concentration. An increase of approximately 1 mm Hg in inspired oxygen tension produces a 1-mm Hg increase in arterial oxygen tension. Inspired oxygen can be increased several hundred millimeters of mercury, and the hypoxemia is easily corrected. Some of the more common causes of hypoventilation are listed in Table 6-1; all reflect abnormalities in the function of the respiratory pump.
Hypoventilation can be identified as a cause of hypoxia with the use of the alveolar air equation:
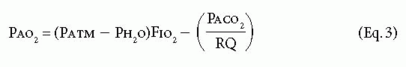
TABLE 6-1. Some Causes of Alveolar Hypoventilation | |||||
|---|---|---|---|---|---|
|
where Pao2 is the partial pressure of oxygen in the alveoli, Patm is the atmospheric pressure, Ph2o is the partial pressure of water (47 mm Hg at body temperature), FIO2 is the fraction of inspired oxygen, PACO2 is the partial pressure of carbon dioxide in the alveoli, and RQ is the respiratory quotient (usually 0.7-0.8 with a normal diet). PAO2–Pao2 is usually called the A-a gradient or (A-a) DO2. It is typically less than 10 in a young person and less than 20 in an older person. If it is normal, hypoxia is due to hypoventilation or a low FIO2. If it is high, hypoxia may be due to  mismatch, shunt, or diffusion impairment.
mismatch, shunt, or diffusion impairment.
 mismatch, shunt, or diffusion impairment.
mismatch, shunt, or diffusion impairment.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


