5 Arrhythmias and Atrioventricular Conduction Disturbances
Normal heart rate varies with age: the younger the child, the faster the heart rate. Therefore, the definitions used for adults of bradycardia (fewer than 60 beats/min) and tachycardia (more than 100 beats/min) have little significance for children. A child has tachycardia when the heart rate is beyond the upper limit of normal for age, and bradycardia when the heart rate is slower than the lower limit of normal (see Table 1-9).
I. BASIC ARRHYTHMIAS
A. RHYTHMS ORIGINATING IN THE SINUS NODE
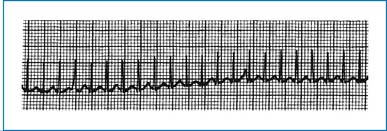
All rhythms that originate in the sinoatrial (SA) node (sinus rhythm) have two important characteristics (Fig. 5-1).
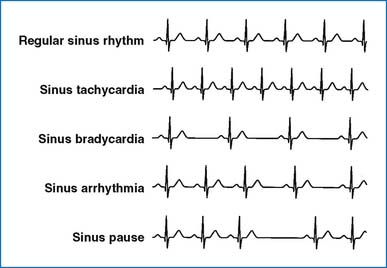
FIG. 5-1 Normal and abnormal rhythms originating in the sinoatrial node.
(From Park MK, Guntheroth WG: How to read pediatric ECGs, ed 4, Philadelphia, 2006, Mosby.)
1. A P wave is present in front of each QRS complex with a regular PR interval. (The PR interval may be prolonged, as in first-degree atrioventricular [AV] block.)
2. The P axis is between 0 and +90 degrees, often a neglected criterion. This produces upright P waves in lead II and inverted P waves in aVR (see Figs. 1-14 and 1-15).
SINUS TACHYCARDIA
1. Description: The characteristics of sinus rhythm are present. A rate above 140 beats/min in children and above 170 beats/min in infants may be significant. In sinus tachycardia the heart rate is usually lower than 200 beats/min (Fig. 5-1).
2. Causes: Anxiety, fever, hypovolemia, circulatory shock, anemia, congestive heart failure (CHF), catecholamines, thyrotoxicosis, and myocardial disease are possible causes.
3. Significance: Increased cardiac work is well tolerated by the healthy myocardium.
SINUS BRADYCARDIA
1. Description: The characteristics of sinus rhythm are present. A rate below 80 beats/min in newborn infants and below 60 beats/min in older children may be significant (Fig. 5-1).
2. Causes: Sinus bradycardia may occur in trained athletes. Vagal stimulation, increased intracranial pressure, hypothyroidism, hypothermia, hypoxia, and drugs such as digitalis and β-adrenergic blockers are possible causes.
3. Significance: Some patients with marked bradycardia do not maintain normal cardiac output.
SINUS ARRHYTHMIA
1. Description: There is a phasic variation in the heart rate, increasing during inspiration and decreasing during expiration, and the two characteristics of sinus rhythm are maintained (Fig. 5-1).
2. Causes: This normal phenomenon is due to a phasic variation in the firing rate of cardiac autonomic nerves with the phase of respiration.
3. Significance: There is no hemodynamic significance.
SINUS PAUSE
1. Description: In sinus pause, there is a momentary cessation of sinus node pacemaker activity, resulting in the absence of P wave and QRS complex for a relatively short duration. Sinus arrest lasts longer and usually results in an escape beat (such as nodal escape).
2. Causes: Increased vagal tone, hypoxia, digitalis toxicity, and sick sinus syndrome (see next section).
3. Significance: No hemodynamic significance is present.
4. Treatment: Treatment is rarely indicated except in sick sinus syndrome and digitalis toxicity.
SINOATRIAL EXIT BLOCK
1. Description: A P wave is absent from the normally expected P wave, resulting in a long RR interval. The duration of the pause is a multiple of the basic PP interval. An impulse formed within the sinus node fails to depolarize the atria.
2. Causes: Excessive vagal stimulation; myocarditis or fibrosis involving the atrium; and drugs such as quinidine, procainamide, or digitalis.
3. Significance: It is usually transient and has no hemodynamic significance.
SINUS NODE DYSFUNCTION (SICK SINUS SYNDROME)
1. Description: The sinus node fails to function as the dominant pacemaker of the heart or performs abnormally slowly, producing a variety of arrhythmias. The arrhythmias may include profound sinus bradycardia, sinus arrest with junctional escape, and ectopic atrial or nodal rhythm. When these arrhythmias are accompanied by symptoms such as dizziness or syncope, sinus node dysfunction is referred to as sick sinus syndrome.
2. Causes: Extensive cardiac surgery involving the atria (e.g., the Fontan operation); arteritis; myocarditis; antiarrhythmic drugs; hypothyroidism; congenital heart disease (CHD), such as sinus venosus atrial septal defect (ASD) or Ebstein anomaly; and occasionally idiopathic occurring in an otherwise normal heart.
3. Significance: Bradytachyarrhythmia is the most worrisome rhythm. Profound bradycardia following a period of tachycardia (overdrive suppression) can cause syncope and even death.
4. Treatment: Severe bradycardia is treated with atropine (0.02 to 0.04 mg/kg, IV, every 2 to 4 hours) or isoproterenol (0.05 to 0.5 mcg/kg, IV) or both. Chronic medical treatment with various drugs has not been successful uniformly. Permanent pacemaker implantation is the treatment of choice in symptomatic patients. Either atrial demand, dual-chambered demand or triggered, or ventricular demand pacemakers may be used.
B. RHYTHMS ORIGINATING IN THE ATRIUM
Atrial arrhythmias (Fig. 5-2) are characterized by the following:
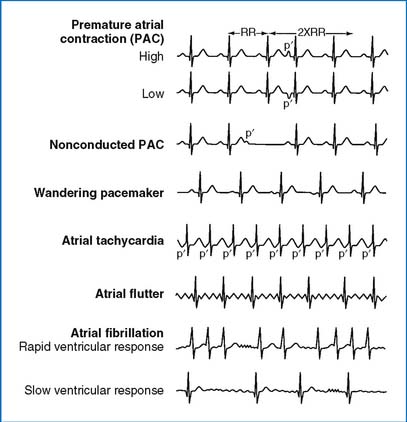
FIG. 5-2 Arrhythmias originating in the atrium.
(From Park MK, Guntheroth WG: How to read pediatric ECGs, ed 4, Philadelphia, 2006, Mosby.)
1. P waves of unusual contour (abnormal P axis) and/or an abnormal number of P waves per QRS complex
2. QRS complexes of normal duration (but with occasional wide QRS duration caused by aberrancy)
PREMATURE ATRIAL CONTRACTION
1. Description: In premature atrial contraction (PAC) the QRS complex occurs prematurely with abnormal P wave morphology. There is an incomplete compensatory pause; that is, the length of two cycles including one premature beat is less than the length of two normal cycles. An occasional PAC is not followed by a QRS complex (i.e., a nonconducted PAC) (Fig. 5-2). A nonconducted PAC is differentiated from a second-degree AV block by the prematurity of the nonconducted P wave (p′ in Fig. 5-2). The P′ wave occurs earlier than the anticipated normal P rate, and the resulting PP′ interval is shorter than the normal PP interval for that individual. In second-degree AV block the P wave that is not followed by the QRS complex occurs at the anticipated time, maintaining a regular PP interval.
2. Causes: Follows cardiac surgery and digitalis toxicity; also appears in healthy children, including newborn infants.
3. Significance: There is no hemodynamic significance.
4. Treatment: Usually no treatment is indicated except in cases of digitalis toxicity.
WANDERING ATRIAL PACEMAKER
1. Description: Gradual changes in the shape of P waves and PR intervals occur. The QRS complex is normal.
2. Causes: This is seen in otherwise healthy children. It is the result of a gradual shift of impulse formation in the atria through several cardiac cycles.
3. Significance: There is no clinical significance.
ECTOPIC ATRIAL TACHYCARDIA
1. Description: There is a narrow QRS complex tachycardia (in the absence of aberrancy or preexisting bundle branch block) with visible P waves at an inappropriately rapid rate. The P axis is different from that of sinus rhythm. When the ectopic focus is near the sinus node, the P axis may be the same as in sinus rhythm. The usual heart rate in older children is between 110 and 160 beats/min, but the tachycardia rate varies substantially during the course of a day, reaching 300 beats/min with sympathetic stimuli. It represents about 20% of supraventricular tachycardia (SVT). This arrhythmia is sometimes difficult to distinguish from the reentrant AV tachycardia and thus it is included under “supraventricular tachycardia.”
2. Causes: This arrhythmia is believed to be secondary to increased automaticity of nonsinus atrial focus or foci. Myocarditis, cardiomyopathies, atrial dilation, atrial tumors, and previous cardiac surgery involving atria (such as Fontan procedure) may be the cause. Most patients have a structurally normal heart (idiopathic).
3. Significance: CHF is common in chronic cases. There is a high association with tachycardia-induced cardiomyopathy.
4. Treatment: It is refractory to medical therapy and cardioversion. Drugs that are effective in reentrant atrial tachycardia (such as adenosine) do not terminate the tachycardia. Cardioversion is ineffective because the ectopic rhythm resumes immediately. The goal may be to slow the ventricular rate (using digoxin or β-blockers) rather than to try to convert the arrhythmia to sinus rhythm. Intravenous amiodarone may achieve rate control relatively quickly. Long-term oral antiarrhythmic drugs (such as flecainide or amiodarone) are the mainstay of therapy in patients not undergoing radiofrequency ablation. Radiofrequency ablation may prove to be effective in nearly 90% of cases.
MULTIFOCAL (OR CHAOTIC) ATRIAL TACHYCARDIA
1. Description: There are three or more distinct P wave morphologies. The PP and RR intervals are irregular with variable PR intervals. The arrhythmia resembles atrial fibrillation. Mechanism of this arrhythmia has been poorly defined. The onset of the arrhythmia may coincide with respiratory illness.
2. Causes: Young infants with (30% to 50%) or without various CHDs.
3. Significance: CHF may develop. Sudden death has been reported in up to 17% while on therapy. Long duration of the arrhythmia may cause left ventricle (LV) systolic dysfunction. Spontaneous resolution frequently occurs.
4. Management: Ineffectiveness of adenosine is a useful diagnostic sign of the condition. Drugs that slow AV conduction (propranolol or digoxin) and those that decrease automaticity (such as class IA or IC or class III) may be useful. Amiodarone (IV followed by PO) may be effective. This arrhythmia is refractory to cardiac pacing, cardioversion, and adenosine.
ATRIAL FLUTTER
1. Description: Atrial flutter is characterized by a fast atrial rate (F waves with saw-tooth configuration) of about 300 beats/min, the ventricle responding with varying degrees of block (e.g., 2:1, 3:1, 4:1), and normal QRS complexes (Fig. 5-2).
2. Causes: Structural heart disease with dilated atria, myocarditis, thyrotoxicosis, previous surgery involving atria, and digitalis toxicity are possible causes. However, most fetuses and neonates with atrial flutter have a normal heart.
3. Significance: The ventricular rate determines the eventual cardiac output; a too-rapid ventricular rate may decrease the cardiac output.
4. Treatment: In acute situations, synchronized cardioversion is the treatment of choice. Adenosine is not effective. It is important to rule out intracardiac thrombus by echo (preferably transesophageal echo) before cardioversion because it may lead to cerebral embolization. If a thrombus is found or suspected, anticoagulation with warfarin (with INR 2 to 3) is started and cardioversion delayed for 2 to 3 weeks. Warfarin is continued for an additional 3 to 4 weeks after conversion to sinus rhythm. To control the ventricular rate, calcium channel blockers, propranolol, or digoxin may be used. Amiodarone may be more effective than digoxin in treating atrial flutter. Quinidine may prevent the recurrences. For refractory cases, antitachycardia pacing or radiofrequency ablation may be indicated.
ATRIAL FIBRILLATION
1. Description: Atrial fibrillation is characterized by an extremely fast atrial rate (f wave at 350 to 600 beats/min) and an irregular ventricular response with normal QRS complexes (Fig. 5-2).
2. Causes: Same as those for atrial flutter.
3. Significance: Atrial fibrillation usually suggests a significant pathology. Rapid ventricular rate and the loss of coordinated contraction of the atria and ventricles decrease cardiac output. Atrial thrombus formation is quite common.
4. Treatment: Treatment of atrial fibrillation is similar to that described under atrial flutter. If atrial fibrillation has been present more than 48 hours, the patient should receive anticoagulation with warfarin for 3 to 4 weeks to prevent systemic embolization of atrial thrombus, if the conversion can be delayed. Anticoagulation is continued for 4 weeks after restoration of sinus rhythm. If cardioversion cannot be delayed, heparin should be started with subsequent oral anticoagulation. Digoxin is given to slow the ventricular rate. Propranolol (1.0 to 4.0 mg/kg/day, orally in three or four doses) may be added. Class I antiarrhythmic agents (e.g., quinidine, procainamide, flecainide) and the class III agent amiodarone may be used. In patients with chronic atrial fibrillation, anticoagulation with warfarin should be considered to reduce the incidence of thromboembolism. Quinidine may prevent recurrence.
SUPRAVENTRICULAR TACHYCARDIA
1. Description: Three groups of tachycardia are included in SVT: atrial, nodal, and AV reentrant tachycardias. The great majority of SVTs are due to reentry AV tachycardia rather than to rapid firing of a single focus in the atria (atrial tachycardia) or in the AV node (nodal tachycardia). The heart rate is extremely rapid and regular (usually 240 ± 40 beats/min) (Fig. 5-3). The P wave is usually invisible, but when it is visible, it has an abnormal P axis and either precedes or follows the QRS complex. The QRS duration is usually normal, but occasionally aberrancy will prolong the QRS, making differentiation of this arrhythmia from ventricular tachycardia difficult.
3. Significance: It may decrease cardiac output and result in CHF in infants (with irritability, tachypnea, poor feeding, and pallor). When CHF develops, the infant’s condition can deteriorate rapidly. Older children and adults may express a fairly unique complaint of “pounding sensation” in the neck, probably caused by cannon waves when the atrium contracts against a simultaneously contracting ventricle.
5. Preventing recurrence of SVT
C. RHYTHMS ORIGINATING IN THE AV NODE
Rhythms originating in the AV node (Fig. 5-4) are characterized by the following:
FIG. 5-4 Arrhythmias originating in the atrioventricular node.
(From Park MK: Pediatric cardiology for practitioners, ed 5, Philadelphia, 2008, Mosby.)
1. The P wave may be absent, or inverted P waves may follow the QRS complex.
2. The QRS complex is usually normal in duration and configuration.
NODAL PREMATURE BEATS
1. Description: A normal QRS complex occurs prematurely. P waves are usually absent, but inverted P waves may follow QRS complexes. The compensatory pause may be complete or incomplete (Fig. 5-4).
2. Causes: Usually idiopathic in an otherwise normal heart but may result from cardiac surgery or digitalis toxicity.
3. Significance: Usually no hemodynamic significance.
4. Treatment: Treatment is not indicated unless the cause is digitalis toxicity.
NODAL ESCAPE BEAT
1. Description: When the sinus node impulse fails to reach the AV node, the node-His (NH) region of the AV node will initiate an impulse (nodal or junctional escape beat). The QRS complex occurs later than the anticipated normal beat. The P wave may be absent, or an inverted P wave may follow the QRS complex (Fig. 5-4).
2. Causes: It may follow cardiac surgery involving the atria (e.g., Fontan operation) or may be seen in otherwise healthy children.
3. Significance: Little hemodynamic significance.
NODAL OR JUNCTIONAL RHYTHM
1. Description: If there is a persistent failure of the sinus node, the AV node may function as the main pacemaker of the heart with a relatively slow rate (40 to 60 beats/min). Either P waves are absent or inverted P waves follow QRS complexes (Fig. 5-4).
2. Causes: It may be seen in an otherwise normal heart, after cardiac surgery, in conditions of an increased vagal tone (e.g., increased intracranial pressure, pharyngeal stimulation), and with digitalis toxicity. Rarely, it may be seen in children with polysplenia syndrome.
3. Significance: The slow heart rate may significantly decrease the cardiac output and produce symptoms.
4. Treatment: No treatment is indicated if the patient is asymptomatic. Atropine or electric pacing is indicated for symptoms. Treatment is directed to digitalis toxicity if caused by digitalis.
ACCELERATED NODAL RHYTHM
1. Description: In the presence of normal sinus rate and AV conduction, if the AV node (NH region) with enhanced automaticity captures the pacemaker function (60 to 120 beats/min), the rhythm is called accelerated nodal (or AV junctional) rhythm. Either P waves are absent or inverted P waves follow QRS complexes.
2. Causes: Idiopathic, digitalis toxicity, myocarditis, or previous cardiac surgery.
3. Significance: Little hemodynamic significance.
4. Treatment: No treatment is necessary unless the cause is digitalis toxicity.
NODAL TACHYCARDIA
1. Description: The ventricular rate varies from 120 to 200 beats/min. Either P waves are absent or inverted P waves follow QRS complexes. The QRS complex is usually normal, but aberration may occur. Nodal tachycardia is difficult to separate from atrial tachycardia. Therefore, both arrhythmias are grouped under SVT (Fig. 5-4).
2. Causes: Similar to those of atrial tachycardia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree