Arrhythmias
 Just the facts
Just the factsIn this chapter, you’ll learn:
♦ ways to identify various arrhythmias
♦ causes of each type of arrhythmia
♦ significance of, treatment for, and nursing implications of each type of arrhythmia
♦ assessment findings for each type of arrhythmia.
A look at arrhythmias
Cardiac arrhythmias are variations in the normal pattern of electrical stimulation of the heart. Arrhythmias vary in severity—from those that are mild, cause no symptoms, and require no treatment (such as sinus arrhythmia) to those that require emergency intervention (such as catastrophic ventricular fibrillation). Arrhythmias are generally classified according to their origin (ventricular or supraventricular). Their effects on cardiac output and blood pressure determine their clinical significance. Lethal arrhythmias, such as pulseless ventricular tachycardia and ventricular fibrillation, are a major cause of cardiac death.
The most common types of arrhythmias include sinus node arrhythmias, atrial arrhythmias, junctional arrhythmias, ventricular arrhythmias, and atrioventricular (AV) blocks.
 |
Sinus node arrhythmias
 When a heart is functioning normally, the sinoatrial (SA) node, also called the sinus node, acts as the primary pacemaker. The sinus node assumes this role because its automatic firing rate exceeds that of the heart’s other pacemakers. In an adult at rest, the sinus node has an inherent firing rate of 60 to 100 times per minute.
When a heart is functioning normally, the sinoatrial (SA) node, also called the sinus node, acts as the primary pacemaker. The sinus node assumes this role because its automatic firing rate exceeds that of the heart’s other pacemakers. In an adult at rest, the sinus node has an inherent firing rate of 60 to 100 times per minute.What nerve!
The SA node’s blood supply comes from the right coronary artery and left circumflex artery. The autonomic nervous system richly innervates the sinus node through the vagus nerve, a parasympathetic nerve, and several sympathetic nerves. Stimulation of the vagus nerve decreases the node’s firing rate, and stimulation of the sympathetic system increases it.
Types of sinus node arrhythmias include sinus arrhythmia, sinus bradycardia, sinus tachycardia, sinus arrest, and sick sinus syndrome.
Sinus arrhythmia
 In sinus arrhythmia, the pacemaker cells of the SA node fire irregularly. The cardiac rate stays within normal limits, but the rhythm is irregular and corresponds to the respiratory cycle. Sinus arrhythmias commonly occur in athletes, children, and elderly people but rarely occur in infants. Conditions unrelated to respiration may also produce sinus arrhythmia, including inferior-wall myocardial infarction (MI), advanced age, use of digoxin (Lanoxin) or morphine, and increased intracranial pressure.
In sinus arrhythmia, the pacemaker cells of the SA node fire irregularly. The cardiac rate stays within normal limits, but the rhythm is irregular and corresponds to the respiratory cycle. Sinus arrhythmias commonly occur in athletes, children, and elderly people but rarely occur in infants. Conditions unrelated to respiration may also produce sinus arrhythmia, including inferior-wall myocardial infarction (MI), advanced age, use of digoxin (Lanoxin) or morphine, and increased intracranial pressure.How it happens
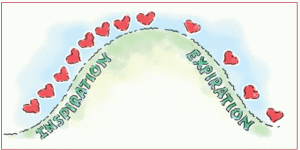
During inspiration, blood flow to the heart increases. This increase reduces vagal tone, which in turn increases heart rate. During expiration, venous return decreases. This increases vagal tone, slowing the heart rate. (See Breathing and sinus arrhythmia.)
What to look for
To identify sinus arrhythmia, observe the patient’s heart rhythm during respiration. The atrial and ventricular rates should be within normal limits (60 to 100 beats/minute) but increase during inspiration and slow with expiration. Electrocardiogram (ECG) complexes fall closer together during inspiration, shortening the P-P interval (the time elapsed between two consecutive P
waves). During expiration, the P-P interval lengthens. The difference between the shortest and longest P-P intervals exceeds 0.12 second. (See Recognizing sinus arrhythmia, page 144.)
waves). During expiration, the P-P interval lengthens. The difference between the shortest and longest P-P intervals exceeds 0.12 second. (See Recognizing sinus arrhythmia, page 144.)
Breathing easy
Check the patient’s peripheral pulse rate. It, too, should increase during inspiration and decrease during expiration. If the arrhythmia is caused by an underlying condition, you may note signs and symptoms of that condition as well.
When evaluating sinus arrhythmia, be sure to check the monitor carefully. A marked variation in P-P intervals in an elderly patient may indicate sick sinus syndrome, a related but more serious phenomenon. (See A longer look at sinus arrhythmia, page 144.)
On the alert
If sinus arrhythmia is caused by drugs, such as morphine or other sedatives, the doctor may decide to continue those medications. If a patient taking digoxin suddenly develops sinus arrhythmia, notify the doctor immediately. The patient may be experiencing digoxin toxicity.
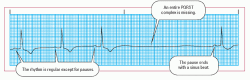
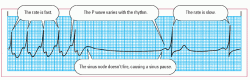
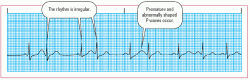
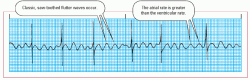
Recognizing sinus arrhythmia
Take a look at this example of how sinus arrhythmia appears on a rhythm strip. Notice its distinguishing characteristics.
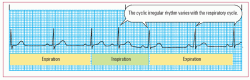 |
• Rhythm: Irregular
• Rate: 60 beats/minute
• P wave: Normal
• PR interval: 0.16 second
• QRS complex: 0.06 second
• T wave: Normal
• QT interval: 0.36 second
• Other: Phasic slowing and quickening
Sinus bradycardia
 In sinus bradycardia, the sinus rate falls below 60 beats/minute while the rhythm remains regular. It may occur normally during sleep or in a person with a well-conditioned heart—an athlete, for instance. That’s because a well-conditioned heart can pump more blood with each contraction, maintaining a normal cardiac output with fewer beats.
In sinus bradycardia, the sinus rate falls below 60 beats/minute while the rhythm remains regular. It may occur normally during sleep or in a person with a well-conditioned heart—an athlete, for instance. That’s because a well-conditioned heart can pump more blood with each contraction, maintaining a normal cardiac output with fewer beats.How it happens
Sinus bradycardia usually occurs as a normal response to a reduced demand for blood flow. In this case, vagal stimulation increases and sympathetic stimulation decreases. As a result, automaticity (the tendency of cells to initiate their own impulses) in the SA node diminishes.
Sinus bradycardia commonly occurs after an inferior-wall MI involving the right coronary artery, which supplies blood to the SA node. Numerous other conditions and the use of certain drugs may also cause sinus bradycardia. (See Causes of sinus bradycardia.)
 Advice from the experts
Advice from the expertsA longer look at sinus arrhythmia
Don’t mistake sinus arrhythmia for other rhythms. At first glance, it may look like atrial fibrillation, normal sinus rhythm with premature atrial contractions, sinoatrial block, or sinus pauses. Observe the monitor and the patient’s respiratory pattern for several minutes to determine the rate and rhythm. As always, check the patient’s pulse.
Causes of sinus bradycardia
Sinus bradycardia may be caused by:
• noncardiac disorders, such as hyperkalemia, increased intracranial pressure, hypothyroidism, hypothermia, sleep, and glaucoma
• conditions producing excess vagal stimulation or decreased sympathetic stimulation, such as sleep, deep relaxation, Valsalva’s maneuver, carotid sinus massage, and vomiting
• cardiac diseases, such as sinoatrial node disease, cardiomyopathy, myocarditis, myocardial ischemia, and heart block; sinus bradycardia can also occur immediately following an inferior-wall myocardial infarction
• certain drugs, especially beta-adrenergic blockers, digoxin (Lanoxin), calcium channel blockers, lithium (Eskalith), and antiarrhythmics, such as sotalol (Betapace), amiodarone (Cordarone), propafenone (Rythmol), and quinidine.
What to look for
In sinus bradycardia, the heartbeat is regular with a rate less than 60 beats/minute. All other ECG findings are normal: a P wave precedes each QRS complex and the PR interval, QRS complex, T wave, and QT interval are all normal. (See Recognizing sinus bradycardia, page 146.)
No symptoms? No problem.
The clinical significance of sinus bradycardia depends on the rate and whether the patient is symptomatic. Most adults can tolerate a sinus bradycardia of 45 to 59 beats/minute.
Symptoms? Problem!
However, if the rate falls below 45 beats/minute, patients usually have signs and symptoms of decreased cardiac output, such as hypotension, dizziness, confusion, or syncope (Stokes-Adams attack). Keep in mind, too, that patients with underlying cardiac disease may be less tolerant of a drop in heart rate.
Bradycardia may also trigger more serious arrhythmias as well. Ectopic beats, such as premature atrial, junctional, or ventricular contractions, may also occur, causing palpitations and an irregular pulse.
In a patient with acute inferior-wall MI, sinus bradycardia is considered a favorable prognostic sign, unless it’s accompanied by hypotension. That’s because, with a slower heart rate, the heart uses less oxygen and avoids ischemia.
Sinus bradycardia rarely affects children. When it occurs in an ill child, it’s considered an ominous sign.
 |
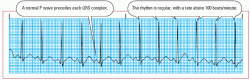
Recognizing sinus bradycardia
Take a look at this example of how sinus bradycardia appears on a rhythm strip. Notice its distinguishing characteristics.
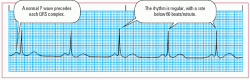 |
• Rhythm: Regular
• Rate: 48 beats/minute
• P wave: Normal
• PR interval: 0.16 second
• QRS complex: 0.08 second
• T wave: Normal
• QT interval: 0.50 second
• Other: None
How you intervene
If the patient is asymptomatic and his vital signs are stable, treatment isn’t necessary. Continue to observe his heart rhythm, monitoring the progression and duration of bradycardia. Evaluate his tolerance of the rhythm at rest and with activity. Also, review the drugs he’s taking. Check with the doctor about stopping medications that may be depressing the SA node, such as digoxin, beta-adrenergic blockers, and calcium channel blockers. Before giving those drugs, make sure the heart rate is within a safe range.
If the patient is symptomatic, treatment aims to identify and correct the underlying cause. Meanwhile, drugs such as atropine, epinephrine, and dopamine, or a temporary or permanently implanted pacemaker, help to maintain an adequate heart rate. Patients with chronic, symptom-producing sinus bradycardia may require insertion of a permanent pacemaker. (See Treating symptom-producing bradycardia.)
Check the ABCs
If the patient abruptly develops a significant sinus bradycardia, assess his airway, breathing, and circulation (ABCs). If these are adequate, determine whether the patient has an effective cardiac output. If not, he may develop these signs and symptoms:
• hypotension
• cool, clammy skin
 |
 Peak technique
Peak techniqueTreating symptom-producing bradycardia
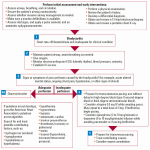 |
See also:
2010 Handbook of Emergency Cardiovascular Care for Healthcare Providers. © 2010, American Heart Association
Advanced Cardiovascular Life Support Provider Manual. © 2011, American Heart Association
Reproduced with permission. 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. © 2010, American Heart Association.
• altered mental status
• dizziness
• blurred vision
• crackles, dyspnea, and a third heart sound (S3), which indicate heart failure
• chest pain
• syncope.
When administering atropine, be sure to give the correct dose: Doses lower than 0.5 mg may have a paradoxical effect, slowing the heart rate even further. Keep in mind that a patient with a transplanted heart won’t respond to atropine and may require pacing for emergency treatment.
Sinus tachycardia
 If sinus bradycardia is the tortoise of the sinus arrhythmias, sinus tachycardia is the hare. Sinus tachycardia in an adult is characterized by a sinus rate greater than 100 beats/minute. The rate rarely exceeds 180 beats/minute except during strenuous exercise; the maximum rate achievable with exercise decreases with age.
If sinus bradycardia is the tortoise of the sinus arrhythmias, sinus tachycardia is the hare. Sinus tachycardia in an adult is characterized by a sinus rate greater than 100 beats/minute. The rate rarely exceeds 180 beats/minute except during strenuous exercise; the maximum rate achievable with exercise decreases with age.How it happens
The clinical significance of sinus tachycardia depends on the underlying cause. (See Causes of sinus tachycardia.)
Causes of sinus tachycardia
Sinus tachycardia may be a normal response to exercise, pain, stress, fever, or strong emotions, such as fear and anxiety. It can also occur:
• with certain cardiac conditions, such as heart failure, cardiogenic shock, and pericarditis
• as a compensatory mechanism in shock, anemia, respiratory distress, pulmonary embolism, sepsis, and hyperthyroidism
• when taking such drugs as atropine, isoproterenol (Isuprel), aminophylline, dopamine, dobutamine, epinephrine, alcohol, caffeine, nicotine, and amphetamines.
Sinus tachycardia in a patient who has had an acute MI suggests massive heart damage and is a poor prognostic sign. Persistent tachycardia may also signal impending heart failure or cardiogenic shock.
What to look for
In sinus tachycardia, atrial and ventricular rhythms are regular. Both rates are equal, generally 100 to 160 beats/minute. As in sinus bradycardia, the P wave is of normal size and shape and precedes each QRS, but it may increase in amplitude. As the heart rate increases, the P wave may be superimposed on the preceding T wave and difficult to identify. The PR interval, QRS complex, and T wave are normal. The QT interval normally shortens with tachycardia. (See Recognizing sinus tachycardia.)
Pulse check!
When assessing a patient with sinus tachycardia, look for a peripheral pulse rate of more than 100 beats/minute with a regular rhythm. Usually, the patient will be asymptomatic.
Recognizing sinus tachycardia
Take a look at this example of how sinus tachycardia appears on a rhythm strip. Notice its distinguishing characteristics.
 |
• Rhythm: Regular
• Rate: 120 beats/minute
• P wave: Normal
• PR interval: 0.14 second
• QRS complex: 0.06 second
• T wave: Normal
• QT interval: 0.34 second
• Other: None
If cardiac output falls and compensatory mechanisms fail, the patient may experience hypotension, syncope, and blurred vision. He may report chest pain and palpitations, commonly described as a pounding chest or a sensation of skipped heartbeats. He may also report a sense of nervousness or anxiety. If heart failure develops, he may exhibit lung crackles, an extra heart sound (S3), and jugular vein distention. (See What happens in tachycardia, page 150.)
Hard on the heart
Because the heart demands more oxygen at higher rates, tachycardia can trigger chest pain in patients with coronary artery disease (CAD). An increase in heart rate can also be detrimental for patients with obstructive types of heart conditions, such as aortic stenosis and hypertrophic cardiomyopathy.
How you intervene
No treatment for sinus tachycardia is necessary if the patient is asymptomatic or if the rhythm is the result of physical exertion. In other cases, the underlying cause may be treated, which usually resolves the arrhythmia. For example, if sinus tachycardia is caused by hemorrhage, treatment includes stopping the bleeding and replacing blood and fluid.
 |
What happens in tachycardia
Tachycardia can lower cardiac output by reducing ventricular filling time and the amount of blood pumped by the ventricles during each contraction. Normally, ventricular volume reaches 120 to 130 ml during diastole. In tachycardia, decreased ventricular volume leads to hypotension and decreased peripheral perfusion.
As cardiac output plummets, arterial pressure and peripheral perfusion decrease. Tachycardia worsens myocardial ischemia by increasing the heart’s demand for oxygen and reducing the duration of diastole—the period of greatest coronary flow.
Slow it down
If sinus tachycardia leads to cardiac ischemia, treatment may include medications to slow the heart rate. The most commonly used drugs include beta-adrenergic blockers, such as metoprolol (Lopressor) and atenolol (Tenormin), and calcium channel blockers such as verapamil (Isoptin) and diltiazem (Cardizem).
The goal of an intervention for the patient with sinus tachycardia is to maintain adequate cardiac output and tissue perfusion and to identify and correct the underlying cause.
Getting at the history
Check the patient’s medication history. Over-thecounter sympathomimetic agents, which mimic the effects of the sympathetic nervous system, may contribute to sinus tachycardia. These agents may be contained in nose drops and cold formulas.
You should also ask about the patient’s use of caffeine, nicotine, herbal supplements, alcohol, and such illicit drugs as cocaine and amphetamines—any of which could trigger tachycardia. Advise him to avoid these substances.
 |
Part of the plan
Here are other steps you should take for the patient with sinus tachycardia:
• Because sinus tachycardia can lead to injury of the heart muscle, check for chest pain or angina. Also assess for signs and symptoms of heart failure, including crackles, an S3 heart sound, and jugular vein distention.
• Monitor intake and output as well as daily weight.
• Check the patient’s level of consciousness (LOC) to assess cerebral perfusion.
• Provide the patient with a calm environment. Help reduce fear and anxiety, which can fuel the arrhythmia.
• Teach about procedures and treatments. Include relaxation techniques in the information you provide.
• Be aware that a sudden onset of sinus tachycardia after an MI may signal extension of the infarction. Prompt recognition is vital so treatment can be started.
Sinus arrest
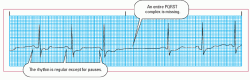
 A disorder of impulse formation, sinus arrest results from a lack of electrical activity in the atrium (atrial standstill). During atrial standstill, the atria aren’t stimulated and an entire PQRST complex is missing from the ECG strip.
A disorder of impulse formation, sinus arrest results from a lack of electrical activity in the atrium (atrial standstill). During atrial standstill, the atria aren’t stimulated and an entire PQRST complex is missing from the ECG strip.Except for this missing complex, or pause, the ECG usually remains normal. Atrial standstill is called sinus pause when one or two beats aren’t formed and sinus arrest when three or more beats aren’t formed.
Sinus arrest closely resembles third-degree SA block, also called exit block, on the ECG strip. (See Understanding sinoatrial blocks, pages 152 and 153.)
 |
How it happens
Sinus arrest occurs when the SA node fails to generate an impulse. Such failure may result from several conditions, including acute infection, heart disease, and vagal stimulation. Pauses of 2 to 3 seconds normally occur in healthy adults during sleep and occasionally in patients with increased vagal tone or hypersensitive carotid sinus disease. Sinus arrest may be associated with sick sinus syndrome, a collection of sinus arrhythmias that includes sinus bradycardia and other abnormalities of the sinus conduction system. (See Causes of sinus arrest, page 154.)
What to look for
When assessing for sinus pause, you’ll find on the ECG that atrial and ventricular rhythms are regular except for a missing complex at the onset of atrial standstill. Atrial and ventricular rates are equal and are usually within normal limits. The rate may vary, however, as a result of the pauses. (See Recognizing sinus arrest, page 155.)
Failing to make an appearance
A P wave that’s of normal size and shape precedes each QRS complex but is absent during a pause. The PR interval is normal and constant when the P wave is present and not measurable when it’s absent. The QRS complex, the T wave, and the QT interval are normal when present and are absent during a pause.
 Now I get it!
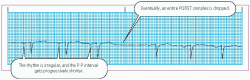
Now I get it!Understanding sinoatrial blocks
In sinoatrial (SA) block, the SA node discharges impulses at regular intervals. Some of those impulses, though, are delayed on their way to the atria. Based on the length of the delay, SA blocks are divided into three categories: first, second, and third degree. Second-degree block is further divided into type I (Wenckebach block) and type II (Mobitz II).
First-degree SA block consists of a delay between the firing of the sinus node and depolarization of the atria. Because the electrocardiogram (ECG) doesn’t show sinus node activity, the only indication of first-degree atrioventricular (AV) block may be a prolongation of the PR interval (greater than 0.20 second). However, you can detect the other three types of SA block.
Second-degree type I block
In second-degree type I block, conduction time between the sinus node and the surrounding atrial tissue becomes progressively longer until an entire cycle is dropped. The pause is less than twice the shortest P-P interval.
 |
 |
Second-degree type II block
In second-degree type II block, conduction time between the sinus node and atrial tissue is normal until an impulse is blocked. The duration of the pause is a multiple of the P-P interval.
 |
Third-degree block
In third-degree block, some impulses are blocked, causing long sinus pauses. The pause isn’t a multiple of the sinus rhythm. On an ECG, third-degree SA block looks similar to sinus arrest but results from a different cause. There is no correlation between P waves and QRS complexes.
Third-degree SA block is caused by a failure to conduct impulses; sinus arrest results from failure to form impulses. Failure in each case causes atrial activity to stop.
In sinus arrest, the pause commonly ends with a junctional escape beat. In third-degree block, the pause lasts for an indefinite period and ends with a sinus beat.
 |
Causes of sinus arrest
Sinus arrest can be caused by:
• sinus node disease, such as fibrosis and idiopathic degeneration
• increased vagal tone, as occurs with Valsalva’s maneuver, carotid sinus massage, and vomiting
• digoxin (Lanoxin), quinidine, procainamide (Pronestyl), and salicylates, especially if given at toxic levels
• excessive doses of beta-adrenergic blockers, such as metoprolol (Lopressor) and propranolol (Inderal)
• cardiac disorders, such as chronic coronary artery disease, acute myocarditis, cardiomyopathy, and hypertensive heart disease
• acute inferior-wall myocardial infarction.
Junctional escape beats, including premature atrial, junctional, or ventricular contractions, may also be present. With sinus arrest, the length of the pause isn’t a multiple of the previous R-R intervals.
Taking a break
You won’t be able to detect a pulse or heart sounds when sinus arrest occurs. If the pauses are short and infrequent, the patient will most likely be asymptomatic and won’t require treatment. He may have a normal sinus rhythm for days or weeks between episodes of sinus arrest, and he may not be able to feel the arrhythmias at all.
Too many for too long
Recurrent and prolonged pauses may cause signs of decreased cardiac output, such as low blood pressure; altered mental status; and cool, clammy skin. The patient may also complain of dizziness or blurred vision. The arrhythmias can produce syncope or near-syncopal episodes within 7 seconds of asystole.
 |
How you intervene
An asymptomatic patient needs no treatment. For a patient displaying mild symptoms, treatment focuses on maintaining cardiac output and identifying the cause of the sinus arrest. That may involve stopping medications that contribute to SA node suppression, such as digoxin, beta-adrenergic blockers, and calcium channel blockers.
Don’t let sleeping pauses lie
Examine the circumstances under which sinus pauses occur. A sinus pause may be insignificant if detected while the patient
is sleeping. If the pauses are recurrent, assess the patient for evidence of decreased cardiac output, such as altered mental status; low blood pressure; and cool, clammy skin.
is sleeping. If the pauses are recurrent, assess the patient for evidence of decreased cardiac output, such as altered mental status; low blood pressure; and cool, clammy skin.
Recognizing sinus arrest
Take a look at this example of how sinus arrest appears on a rhythm strip. Notice its distinguishing characteristics.
 |
• Rhythm: Regular, except for the missing PQRST complexes
• Rate: 88 beats/minute except during pause
• P wave: Normal; missing during pause
• PR interval: 0.20 second
• QRS complex: 0.08 second; absent during pause
• T wave: Normal; absent during pause
• QT interval: 0.40 second; absent during pause
• Other: None
Ask him whether he’s dizzy or light-headed or has blurred vision. Does he feel as if he has passed out? If so, he may be experiencing syncope from a prolonged sinus arrest.
Document the patient’s vital signs and how he feels during pauses as well as what activities he was involved in when they occurred. Activities that increase vagal stimulation, such as Valsalva’s maneuver or vomiting, increase the likelihood of sinus pauses.
When matters get even worse
Assess for a progression of the arrhythmia. Notify the doctor immediately if the patient becomes unstable. Withhold medications that may contribute to sinus pauses and check with the doctor about whether those drugs should be continued.
If appropriate, be alert for signs of digoxin (Lanoxin), quinidine, or procainamide (Pronestyl) toxicity. Obtain a serum digoxin level and a serum electrolyte level.
Arresting the arrest
A patient who develops signs of circulatory collapse needs immediate treatment. As with sinus bradycardia, emergency treatment
includes administration of atropine or epinephrine and the use of a temporary pacemaker. A permanent pacemaker may be implanted for long-term management.
includes administration of atropine or epinephrine and the use of a temporary pacemaker. A permanent pacemaker may be implanted for long-term management.
The goal for the patient with sinus arrest is to maintain adequate cardiac output and perfusion. Be sure to record and document the frequency and duration of pauses. Determine whether a pause is the result of sinus arrest or SA block. If a pacemaker is implanted, give the patient discharge instructions about pacemaker care.
Sick sinus syndrome
 Also called sinus nodal dysfunction, sick sinus syndrome refers to a wide spectrum of SA node abnormalities. The syndrome is caused by disturbances in the way impulses are generated or the inability to conduct impulses to the atrium.
Also called sinus nodal dysfunction, sick sinus syndrome refers to a wide spectrum of SA node abnormalities. The syndrome is caused by disturbances in the way impulses are generated or the inability to conduct impulses to the atrium.Sick sinus syndrome usually shows up as bradycardia, with episodes of sinus arrest and SA block interspersed with sudden, brief periods of rapid atrial fibrillation. Patients are also prone to paroxysms of other atrial tachyarrhythmias, such as atrial flutter and ectopic atrial tachycardia, a condition sometimes referred to as bradycardia-tachycardia (or brady-tachy) syndrome.
Most patients with sick sinus syndrome are older than age 60, but anyone can develop the arrhythmia. It’s rare in children except after open-heart surgery that results in SA node damage. The arrhythmia affects men and women equally. The onset is progressive, insidious, and chronic.
How it happens
Sick sinus syndrome results either from a dysfunction of the sinus node’s automaticity or from abnormal conduction or blockages of impulses coming out of the nodal region. These conditions, in turn, stem from a degeneration of the area’s autonomic nervous system and partial destruction of the sinus node, as may occur with an interrupted blood supply after an inferior-wall MI. (See Causes of sick sinus syndrome.)
Causes of sick sinus syndrome
Sick sinus syndrome may result from:
• conditions leading to fibrosis of the sinoatrial (SA) node, such as increased age, atherosclerotic heart disease, hypertension, and cardiomyopathy
• trauma to the SA node caused by open-heart surgery (especially valvular surgery), pericarditis, or rheumatic heart disease
• autonomic disturbances affecting autonomic innervation, such as hypervagotonia and degeneration of the autonomic system
• cardioactive medications, such as digoxin (Lanoxin), beta-adrenergic blockers, and calcium channel blockers.
Blocked exits
In addition, certain conditions can affect the atrial wall surrounding the SA node and cause exit blocks. Conditions that cause inflammation or degeneration of atrial tissue can also lead to sick sinus syndrome. In many patients, though, the exact cause of sick sinus syndrome is never identified.
What to look for
Sick sinus syndrome encompasses several potential rhythm disturbances that may be intermittent or chronic. (See Recognizing sick sinus syndrome.) Those rhythm disturbances include one or a combination of the following conditions:
• sinus bradycardia
• SA block
• sinus arrest
• sinus bradycardia alternating with sinus tachycardia
• episodes of atrial tachyarrhythmias, such as atrial fibrillation and atrial flutter
• failure of the sinus node to increase heart rate with exercise.
Check for speed bumps
Look for an irregular rhythm with sinus pauses and abrupt rate changes. Atrial and ventricular rates may be fast, slow, or alternating periods of fast rates and slow rates interrupted by pauses.
The P wave varies with the rhythm and usually precedes each QRS complex. The PR interval is usually within normal limits but varies with changes in the rhythm. The QRS complex and T wave are usually normal, as is the QT interval, which may vary with rhythm changes.
 |
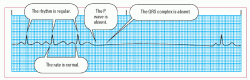
Recognizing sick sinus syndrome
Take a look at this example of how sick sinus syndrome appears on a rhythm strip. Notice its distinguishing characteristics.
 |
• Rhythm: Irregular
• Rate: Atrial—60 beats/minute; ventricular—70 beats/minute
• P wave: Configuration varies
• PR interval: Varies with rhythm
• QRS complex: 0.10 second
• T wave: Configuration varies
• QT interval: Varies with rhythm changes
• Other: None
Make up your mind!
The patient’s pulse rate may be fast, slow, or normal, and the rhythm may be regular or irregular. You can usually detect an irregularity on the monitor or when palpating the pulse, which may feel inappropriately slow and then become rapid.
If you monitor the patient’s heart rate during exercise or exertion, you may observe an inappropriate response to exercise such as a failure of the heart rate to increase. You may also detect episodes of brady-tachy syndrome, atrial flutter, atrial fibrillation, SA block, or sinus arrest on the monitor.
That sinking feeling
The patient may show signs and symptoms of decreased cardiac output, such as hypotension, blurred vision, and syncope, a common experience with this arrhythmia. The length of a pause significant enough to cause syncope varies with the patient’s age, posture at the time, and cerebrovascular status. Consider any pause that lasts 2 to 3 seconds significant.
Other assessment findings depend on the patient’s condition. For instance, he may have crackles in the lungs, an S3 heart sound, or a dilated and displaced left ventricular (LV) apical impulse if he has underlying cardiomyopathy.
How you intervene
The significance of sick sinus syndrome depends on the patient’s age, the presence of other diseases, and the type and duration of the specific arrhythmias that occur. If atrial fibrillation is involved, the prognosis is worse, most likely because of the risk of thromboembolic complications.
As with other sinus node arrhythmias, no treatment is necessary if the patient is asymptomatic. If the patient is symptomatic, however, treatment aims to alleviate signs and symptoms and correct the underlying cause of the arrhythmia.
Atropine or epinephrine may be given initially for an acute attack. A pacemaker may be used until the underlying disorder resolves. Tachyarrhythmias may be treated with antiarrhythmic medications, such as metoprolol and digoxin.
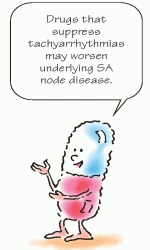
When the solution is part of the problem
Unfortunately, medications used to suppress tachyarrhythmias may worsen underlying SA node disease and bradyarrhythmias. The patient may need anticoagulants if he develops sudden bursts, or paroxysms, of atrial fibrillation. The anticoagulants help prevent thromboembolism and stroke, a complication of the condition. Because the syndrome is progressive and chronic, a symptomatic patient needs lifelong treatment.
 |
Keep a running total
When caring for a patient with sick sinus syndrome, monitor and document all arrhythmias he experiences and signs or symptoms he develops. Assess how his rhythm responds to activity and pain and look for changes in the rhythm.
Watch the patient carefully after starting calcium channel blockers, beta-adrenergic blockers, or other antiarrhythmic medications. If treatment includes anticoagulant therapy and/or the insertion of a pacemaker, make sure the patient and his family receives appropriate instruction.
Atrial arrhythmias
 Atrial arrhythmias, the most common cardiac rhythm disturbances, result from impulses originating in areas outside the SA node. These arrhythmias can affect ventricular filling time and diminish the strength of the atrial kick, a contraction that normally provides the ventricles with up to 30% of their blood.
Atrial arrhythmias, the most common cardiac rhythm disturbances, result from impulses originating in areas outside the SA node. These arrhythmias can affect ventricular filling time and diminish the strength of the atrial kick, a contraction that normally provides the ventricles with up to 30% of their blood.Triple play
Atrial arrhythmias are thought to result from three mechanisms— altered automaticity, circuit reentry, and afterdepolarization. Let’s take a look at each cause and review specific atrial arrhythmias:
• Altered automaticity—An increase in the automaticity (the ability of cardiac cells to initiate impulses on their own) of the atrial fibers can trigger abnormal impulses. Causes of increased automaticity include extracellular factors, such as hypoxia, hypocalcemia, and digoxin toxicity, and conditions in which the function of the heart’s normal pacemaker, the SA node, is diminished. For example, increased vagal tone or hypokalemia can increase the refractory period of the SA node and allow atrial fibers to fire impulses.
• Circuit reentry—In circuit reentry, an impulse is delayed along a slow conduction pathway. Despite the delay, the impulse remains active enough to produce another impulse during myocardial repolarization. Circuit reentry may occur with CAD, cardiomyopathy, or an MI.
• Afterdepolarization—Afterdepolarization can occur with cell injury, digoxin toxicity, and other conditions. An injured cell sometimes only partly repolarizes. Partial repolarization can lead to a repetitive ectopic firing called triggered activity. The depolarization produced by triggered activity is known as afterdepolarization and can lead to atrial or ventricular tachycardia.
 |
Atrial arrhythmias include premature atrial contractions (PACs), atrial flutter, atrial fibrillation, and atrial tachycardia. Let’s examine each atrial arrhythmia in detail.
Premature atrial contractions
 PACs originate outside the SA node and usually result from an irritable spot, or focus, in the atria that take over as pacemaker for one or more beats. The SA node fires an impulse, but then an irritable focus jumps in, firing its own impulse before the SA node can fire again.
PACs originate outside the SA node and usually result from an irritable spot, or focus, in the atria that take over as pacemaker for one or more beats. The SA node fires an impulse, but then an irritable focus jumps in, firing its own impulse before the SA node can fire again.PACs may not be conducted through the AV node and the rest of the heart, depending on their prematurity and the status of the AV and intraventricular conduction system. Nonconducted or blocked PACs don’t trigger a QRS complex.
How it happens
PACs commonly occur in a normal heart and are rarely dangerous in a patient who doesn’t have heart disease. In fact, they usually cause no symptoms and can go unrecognized for years. (See Causes of PACs.)
Causes of PACs
Premature atrial contractions (PACs) may be triggered by:
• alcohol and cigarette use
• anxiety
• fatigue
• fever
• infection
• coronary or valvular heart disease
• acute respiratory failure or hypoxia
• pulmonary disease
• digoxin toxicity
• electrolyte imbalances.
A sign of things to come
However, in patients with heart disease, PACs may lead to more serious arrhythmias, such as atrial fibrillation and atrial flutter. In a patient who has had an acute MI, PACs can serve as an early sign of heart failure or an electrolyte imbalance. PACs can also result from the release of the neurohormone catecholamine during episodes of pain or anxiety.
What to look for
With PACs, atrial and ventricular rates are irregular, but the underlying rhythm may be regular. When the PAC is conducted through the ventricles, the QRS complex appears normal on the patient’s ECG.
Because the PAC depolarizes the SA node early, the SA node must reset itself. This action causes a pause after the PAC, disrupting the normal cycle. The next sinus beat then occurs sooner than it normally would, causing the P-P interval between two normal beats that have been interrupted by a PAC to be shorter than three consecutive sinus beats. This occurrence is referred to as noncompensatory pause. (See Recognizing PACs.)
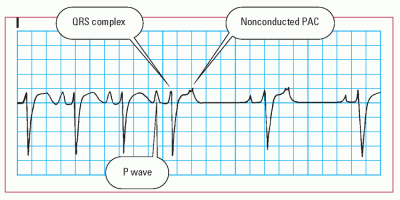
Recognizing PACs
Take a look at this example of how premature atrial contractions (PACs) appear on a rhythm strip. Notice the distinguishing characteristics.
 |
• Rhythm: Irregular
• Rate: 90 beats/minute
• P wave: Abnormal with PAC; some lost in previous T wave
• PR interval: 0.12 second
• QRS complex: 0.08 second
• T wave: Abnormal with some embedded P waves
• QT interval: 0.32 second
• Other: Noncompensatory pause
A hallmark moment
The hallmark ECG characteristic of a PAC is a premature P wave with an abnormal configuration (when compared with a sinus P wave). It may be lost in the previous T wave, distorting that wave’s configuration. (The T wave might be bigger or have an extra bump.) Varying configurations of the P wave indicate more than one ectopic site. (See Nonconducted PACs and second-degree AV block, page 162.)
The PR interval is usually normal but may be shortened or slightly prolonged, depending on the origin of the ectopic focus. If no QRS complex follows the premature P wave, a nonconducted PAC has occurred.
PACs may occur in bigeminy (every other beat is a PAC), trigeminy (every third beat is a PAC), or couplets (two PACs at a time). The patient may have an irregular peripheral or apical pulse rhythm when the PACs occur. He may complain of palpitations, skipped beats, or a fluttering sensation. In a patient with heart disease, signs and symptoms of decreased cardiac output—such as hypotension and syncope—may occur.
 Advice from the experts
Advice from the expertsNonconducted PACs and second-degree AV block
Don’t confuse nonconducted premature atrial contractions (PACs) with type II second-degree atrioventricular (AV) block. In type II second-degree AV block, the P-P interval is regular. A nonconducted PAC, however, is an atrial impulse that arrives early to the AV node, when the node isn’t yet repolarized.
As a result, the premature P wave fails to be conducted to the ventricle. The rhythm strip below shows a P wave embedded in the preceding T wave.
 |
How you intervene
Most patients who are asymptomatic don’t need treatment. If the patient is symptomatic, however, treatment may focus on eliminating the cause, such as caffeine or alcohol. People who have frequent PACs may be treated with drugs that prolong the refractory period of the atria. Those drugs include digoxin, procainamide, and quinidine.
The patient’s part
When caring for a patient with PACs, assess him to help determine what’s triggering the ectopic beats. Tailor your patient teaching to help the patient correct or avoid the underlying cause. For example, the patient might need to avoid caffeine or smoking or learn stress reduction techniques to lessen his anxiety.
If the patient has ischemic or valvular heart disease, monitor him for signs and symptoms of heart failure, electrolyte imbalances, and the development of more severe atrial arrhythmias.
 |
Atrial flutter
 Atrial flutter, a supraventricular tachycardia (a rapid rhythm in which the impulse comes from above the ventricle), is characterized by an atrial rate of 250 to 400 beats/minute, although it’s generally around 300 beats/minute. Originating in a single atrial focus, this rhythm results from circuit reentry and possibly increased automaticity.
Atrial flutter, a supraventricular tachycardia (a rapid rhythm in which the impulse comes from above the ventricle), is characterized by an atrial rate of 250 to 400 beats/minute, although it’s generally around 300 beats/minute. Originating in a single atrial focus, this rhythm results from circuit reentry and possibly increased automaticity.How it happens
Atrial flutter is commonly associated with second-degree block. In that instance, the AV node fails to allow conduction of all the impulses to the ventricles. As a result, the ventricular rate is slower. Atrial flutter rarely occurs in a healthy person. When it does, it may indicate intrinsic cardiac disease. (See Causes of atrial flutter.)
Causes of atrial flutter
Atrial flutter may be caused by:
• conditions that enlarge atrial tissue and elevate atrial pressures, such as severe mitral valve disease, hyperthyroidism, pericardial disease, and primary myocardial disease
• cardiac surgery
• acute myocardial infarction
• chronic obstructive pulmonary disease
• systemic arterial hypoxia.
What to look for
Atrial flutter is characterized by abnormal P waves that lose their distinction because of the rapid atrial rate. The waves blend together, creating a saw-toothed or shark fin appearance and are called flutter waves, or F waves. Varying degrees of AV block produce ventricular rates one-half to one-fourth of the atrial rate. The QRS complex is usually normal but may be widened if flutter waves are buried in the complex. You won’t be able to identify a T wave, nor will you be able to measure the QT interval. (See Recognizing atrial flutter, page 164.)
A flitter, a flutter
The atrial rhythm may vary between fibrillatory waves and flutter waves, an arrhythmia commonly referred to as atrial fibrillation and flutter. Fibrillatory waves are uneven baseline fibrillation waves caused by the initiation of chaotic impulses from multiple ectopic sites in the atria. Depolarization can’t spread in an organized manner because the atria quiver instead of contract.
Rating the ratio
The clinical significance of atrial flutter is determined by the number of impulses conducted through the node—expressed as a conduction ratio, for example, 2:1 or 4:1 (meaning that for every 2 atrial impulses, 1 is conducted; or for every 4, 1 is conducted)— and the resulting ventricular rate. If the ventricular rate is too slow (less than 40 beats/minute) or too fast (more than 150 beats/minute), cardiac output may be seriously compromised.
Usually the faster the ventricular rate, the more dangerous the arrhythmia. The rapid rate reduces ventricular filling time and coronary perfusion, which can cause angina, heart failure, pulmonary edema, hypotension, and syncope.
Recognizing atrial flutter
Take a look at this example of how atrial flutter appears on a rhythm strip. Notice its distinguishing characteristics.
 |
• Rhythm: Atrial—regular; ventricular— irregular
• Rate: Atrial—280 beats/minute; ventricular—60 beats/minute
• P wave: Classic saw-toothed appearance
• PR interval: Unmeasurable
• QRS complex: 0.08 second
• T wave: Unidentifiable
• QT interval: Unidentifiable
• Other: None
One of the most common rates is 150 beats/minute. With an atrial rate of 300, that rhythm is referred to as a 2:1 block. (See Atrial flutter and sinus tachycardia.)
Misleading pulses
When caring for a patient with atrial flutter, you may note that his peripheral or apical pulse is normal in rate and rhythm. That’s because the pulse reflects the number of ventricular contractions, not the number of atrial impulses.
If the ventricular rate is normal, the patient may be asymptomatic. However, if the ventricular rate is rapid, the patient may exhibit signs and symptoms of reduced cardiac output and cardiac decompensation.
How you intervene
If the patient is asymptomatic and with no other acute underlying or associated conditions, monitor him. He may be prescribed medications such as digoxin or a calcium channel blocker to decrease the rate if needed. However, atrial flutter with a rapid ventricular response and reduced cardiac output requires immediate intervention. Therapy aims to control the ventricular rate and convert the atrial ectopic rhythm to a normal sinus rhythm. Although stimulation of the vagus nerve may temporarily increase
the block ratio and slow the ventricular rate, the effects won’t last. For that reason, cardioversion remains the treatment of choice for a symptomatic patient exhibiting atrial flutter.
the block ratio and slow the ventricular rate, the effects won’t last. For that reason, cardioversion remains the treatment of choice for a symptomatic patient exhibiting atrial flutter.
 Advice from the experts
Advice from the expertsAtrial flutter and sinus tachycardia
Whenever you see sinus tachycardia with a rate of 150 beats/minute, take another look. That rate is a common one for atrial flutter with 2:1 conduction. Look closely for flutter waves, which may be difficult to see if they’re hidden in the QRS complex. You may need to check another lead to clearly see them.
A shocking solution
Synchronized cardioversion delivers an electrical stimulus during depolarization. The stimulus makes part of the myocardium refractory to ectopic impulses and terminates circuit reentry movements.
Become a convert
Drug therapy includes digoxin and calcium channel blockers, which decrease AV conduction time. Quinidine may be given to convert flutter to fibrillation, an easier arrhythmia to treat. If digoxin and quinidine therapy is used, the patient must first be given a loading dose of digoxin. Ibutilide (Corvert) may be used to convert recent-onset atrial flutter to sinus rhythm. If possible, the underlying cause of the atrial flutter should be treated. However, it should only be used if the atrial flutter or fibrillation have been going on for less than 48 hours, and there is a high risk for arrhythmias in patients who show LV dysfunction. If treatment is to be administered, synchronized cardioversion is still the best option, especially for the unstable patient.
 |
Keeping watch
Because atrial flutter may be an indication of intrinsic cardiac disease, monitor the patient closely for signs and symptoms of low cardiac output. If cardioversion is indicated, prepare the patient for IV administration of a sedative or anesthetic as ordered. The American Heart Association (AHA) recommends caution with the use of sedation and/or analgesia if the patient is hypotensive (systolic blood pressure [SBP] <90) or has any neurologic compromise; however, it should be remembered that this is an extremely uncomfortable and even painful procedure for most patients. Keep resuscitative equipment at the bedside. Be alert to the effects of digoxin, which depresses the SA node. Also, be alert for bradycardia because cardioversion can decrease the heart rate.
Atrial fibrillation
 Atrial fibrillation, sometimes called A-fib, is defined as chaotic, asynchronous, electrical activity in atrial tissue. The ectopic impulses may fire at a rate of 400 to 600 times/minute, causing the atria to quiver instead of contract. The previously described atrial kick no longer exists.
Atrial fibrillation, sometimes called A-fib, is defined as chaotic, asynchronous, electrical activity in atrial tissue. The ectopic impulses may fire at a rate of 400 to 600 times/minute, causing the atria to quiver instead of contract. The previously described atrial kick no longer exists.The ventricles respond only to those impulses that make it through the AV node. On an ECG, atrial activity is no longer represented by P waves but by erratic baseline waves called fibrillatory waves, or F waves. This rhythm may either be sustained or paroxysmal (occurring in bursts). It can be preceded by, or result from, PACs.
 |
How it happens
Atrial fibrillation occurs more commonly than atrial flutter or atrial tachycardia. It stems from the firing of several impulses in circuit reentry pathways. (See Causes of atrial fibrillation.)
What to look for
In atrial fibrillation, small sections of the atria are activated individually. This situation causes the atrial muscle to quiver, or fibrillate, instead of contract. On an ECG, you’ll see uneven baseline F waves rather than clearly distinguishable P waves. Also, when several ectopic sites in the atria fire impulses, depolarization can’t spread in an organized manner, which causes an irregular ventricular response. (See Recognizing atrial fibrillation.)
That fabulous filter
The AV node protects the ventricles from the 400 to 600 erratic atrial impulses that occur each minute by acting as a filter and
blocking some of the impulses. The AV node itself doesn’t receive all the impulses, however. If muscle tissue around the AV node is in a refractory state, impulses from other areas of the atria can’t reach the AV node, which further reduces the number of atrial impulses conducted through to the ventricles. These two factors help explain the characteristic wide variation in R-R intervals in atrial fibrillation.
blocking some of the impulses. The AV node itself doesn’t receive all the impulses, however. If muscle tissue around the AV node is in a refractory state, impulses from other areas of the atria can’t reach the AV node, which further reduces the number of atrial impulses conducted through to the ventricles. These two factors help explain the characteristic wide variation in R-R intervals in atrial fibrillation.
Causes of atrial fibrillation
Atrial fibrillation may be caused by:
• cardiac surgery
• heart conditions, such as mitral insufficiency, mitral stenosis, hyperthyroidism, infection, coronary artery disease, acute myocardial infarction, pericarditis, hypoxia, and atrial septal defects
• coffee, alcohol, or cigarette use
• fatigue or stress
• certain drugs, such as aminophylline and digoxin (Lanoxin)
• catecholamine release during exercise.
Recognizing atrial fibrillation
Take a look at this example of how atrial fibrillation appears on a rhythm strip. Notice its distinguishing characteristics.
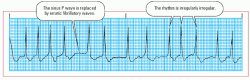 |
• Rhythm: Irregularly irregular
• Rate: Atrial—indiscernible; ventricular—130 beats/minute
• P wave: Absent; replaced by fine fibrillatory waves
• PR interval: Indiscernible
• QRS complex: 0.08 second
• T wave: Indiscernible
• QT interval: Unmeasurable
• Other: None
Fast and furious
The atrial rate is almost indiscernible but is usually greater than 400 beats/minute. The ventricular rate usually varies from 100 to 150 beats/minute but can be lower. Atrial fibrillation is called coarse if the F waves are pronounced; the fibrillation is called fine if they aren’t. Atrial fibrillation and flutter may also occur simultaneously. Look for a configuration that varies between fibrillatory waves and flutter waves.
As with other atrial arrhythmias, atrial fibrillation eliminates atrial systole (also known as atrial kick). That loss, combined with the decreased filling times associated with rapid rates, can lead to clinically significant problems. If the ventricular response is greater than 100 beats/minute—a condition called uncontrolled atrial fibrillation or rapid ventricular response—the patient may develop heart failure, angina, or syncope.
 |
Preexisting problems
Patients with preexisting cardiac disease, such as hypertrophic obstructive cardiomyopathy, mitral stenosis, rheumatic heart disease, and mitral prosthetic valves, tend to tolerate atrial fibrillation poorly and may develop shock and severe heart failure.
Left untreated, atrial fibrillation can lead to cardiovascular collapse, thrombus formation, and systemic arterial or pulmonary embolism.
How you intervene
When assessing a patient with atrial fibrillation, assess both the peripheral and apical pulses. You may find that the radial pulse rate is slower than the apical rate. That’s because the weaker contractions of the heart don’t produce a palpable peripheral pulse.
If the ventricular rate is rapid, the patient may show signs and symptoms of decreased cardiac output, including hypotension and light-headedness. His heart may be able to compensate for the decrease if the fibrillation lasts long enough to become chronic. In those cases, however, the patient is at a greater-than-normal risk for developing pulmonary, cerebral, or other emboli and may exhibit signs of those conditions.
Goal: Reduce the rate
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree