Arrhythmias
The cardiac conduction system
Cardiac action potential
The resting cardiac myocyte is electrically negative, with a transmembrane voltage of between –50 mV and –95 mV. This is due to the distribution of K+, Na+, Cl–, and Ca2+ ions across the cell membrane. The negativity is maintained by the energy-consuming Na+/K+ pump, which transports three Na+ ions out of the cell for two K+ ions inward. During phase 4 of the action potential, the voltage slowly increases until a threshold of –60 mV is reached, which opens voltage-gated Na+ channels and triggers depolarization. The voltage changes in one cell are spread to adjacent cells via gap junctions between them, such that a wavefront of electrical activation is propagated. At least ten distinct ion channels modulate the voltage changes that occur in the action potential (Figs. 10.1 and 10.2).
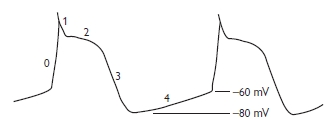
Fig. 10.1 The cardiac action potential.
The action potential has five parts:
0 rapid influx of Na+ causing fast depolarization
1 rapid early repolarization due to efflux of Na+
2 plateau phase where repolarization is slowed by an influx of Ca2+
3 repolarization due to the the efflux of K+
4 diastole with a steady-state resting transmembrane voltage.
The plateau phase distinguishes the cardiac from neuronal action potential. The release of Ca2+ during phase 2 triggers mechanical contraction of the cell.
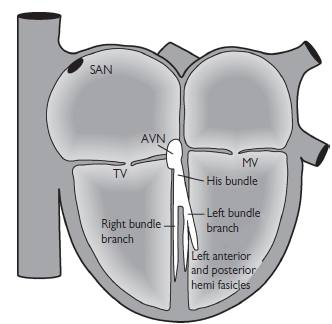
Fig. 10.2 Anatomy of the normal conduction system. AVN = atrioventricular node; MV = mitral valve;. SAN = sinoatrial node; TV = tricuspid valve.
This is the ability of all cardiac cells to spontaneously depolarize. It is caused by the inward flow of positive ions during diastole. At potentials more negative than –60 mV, ion channels open allowing a slow influx of cations. The slow influx of Ca2+ in the sinoatrial node (SAN) allows it to depolarize more rapidly and therefore suppress other potential pacemaker sites.
Sinoatrial node
Automaticity
The SAN sits high in the lateral right atrium (RA) just below the superior vena cava (SVC). It is 1–2 cm in length, 2–3 mm wide, and less than 1 mm from the epicardial surface. It is the dominant site of impulse generation; impulses are conducted out of the sinus node to depolarize the surrounding RA. The SAN is richly innervated with both adrenergic and cholinergic receptors, which alter the rate of depolarization hence controlling the heart rate. Activation spreads out from the SAN to the rest of the RA and left atrium (LA) via specialized interatrial connections including Bachmann’s bundle.
Atrioventricular node
The atrioventricular node (AVN) is found in the RA anterior to the mouth of the coronary sinus and directly above the insertion of the septal leaflet of the tricuspid valve. It is the only electrical connection to the ventricle, via the bundle of His, which, like the SAN it is also densely innervated with sympathetic and parasympathetic fibres.
His–Purkinje system
The electrical impulse conducts rapidly through the bundle of His into the upper part of the interventricular septum, where it splits into two branches: the right bundle branch, which continues down the right side of the septum to the apex of the right ventricle and the base of the anterior papillary muscle, and the left bundle branch, which further splits into two fascicles, anterior and posterior. The terminal Purkinje fibres connect with the ends of the bundle branches, forming an interweaving network on the endocardial surface so that a cardiac impulse is transmitted almost simultaneously to the entire right and left ventricles.
Bradycardia: general approach
Investigations
| • 12-lead electrocardiogram (ECG) and rhythm strip | Look specifically for the relationship between P waves and QRS complex. A long rhythm strip is sometimes necessary to detect complete heart block if atrial and ventricular rates are similar |
| • Blood tests | Full blood count (FBC), biochemistry, glucose (urgently) Ca2+, Mg2+ (especially if on diuretics) Biochemical markers of cardiac injury |
| • Where appropriate | Blood cultures, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) Thyroid function tests (TFTs) Drug levels. Arterial blood gases |
| • Chest x-ray | Heart size ?Signs of pulmonary oedema |
Emergency nanagement
Haemodynamically unstable patients
Haemodynamically stable patients
Long-term management
External cardiac pacing
Sinus bradycardia
In sinus bradycardia, the SAN discharges <60/min. P waves are normal but slow. It may be normal (e.g. in sleep, healthy resting hearts).
Causes
Sinus pause
The SAN fails to generate impulses (sinus arrest) or the impulses are not conducted to the atria (SA exit block). A single dropped P wave with a PP interval that is a multiple of the basic PP interval suggests exit block. A period of absent P waves suggests sinus arrest. Causes include, excess vagal tone, acute myocarditis, MI, aging (fibrosis), stroke, digoxin toxicity, and anti-arrhythmic drugs.
Sick sinus syndrome
This syndrome encompasses a number of conduction system problems: persistent sinus bradycardia not caused by drugs, sinus pauses, AV conduction disturbances, and paroxysms of atrial arrythmias. It is usually diagnosed by ambulatory cardiac monitoring.
Atrioventricular block
This can occur at the AVN (nodal) or His–Purkinje system (infranodal). Common causes are ischaemic heart disease (IHD), conduction system fibrosis (aging), calcific aortic stenosis, congenital, cardiomyopathy, hypothermia, hypothyroidism, trauma, radiotherapy, infection, connective tissue disease, sarcoidosis, and anti-arrhythmic drugs. AV block is further classified:
First-degree AV block
Every impulse conducts to the ventricle but the conduction time is prolonged. Every P wave is followed by a QRS but with a prolonged PR interval (>200 ms). If the QRS width is normal then the block is at the AV node, if the QRS shows aberration (right (RBBB) or left bundle branch block (LBBB)), then the block may be at the AV node or the His–Purkinje system.
Second-degree AV block
Third-degree AV block (complete heart block)
There is no conduction to the ventricle. The ECG shows dissociation between the P and QRS complexes. An escape pacemaker rhythm takes over. A narrow QRS indicates AVN block, and the His bundle is the pacemaker, which is faster and more stable than more distal sites. A wide QRS indicates infranodal block and a distal ventricular pacemaker site. Asystole may occur; therefore, this carries a worse prognosis. This type of heart block always requires implantation of a permanent pacemaker.
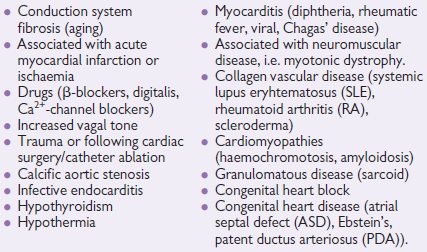
Causes of atrioventricular block
Bundle branch block
This is due to disease in the His–Purkinje system causing a QRS>120 ms. Common causes are conduction system fibrosis (aging), IHD, hypertension, cardiomyopathies, cardiac surgery, infiltrative diseases (e.g. amyloid).
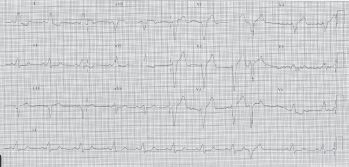
Fig. 10.3 ECG showing LBBB. There is a wide QRS complex with large notched R waves in leads I and V6 and a deep S wave in V1.
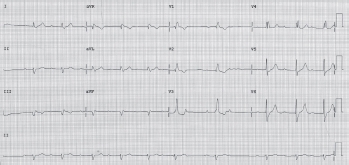
Fig. 10.4 ECG showing bifasicular block. There is a wide QRS complex with an rSr pattern in V1 and deep slurred S wave in V6 (=RBBB). The QRS in lead 1 is positive and lead aVF negative (=left anterior hemiblock). There is also 2nd-degree AV nodal block (Mobitz type 1 or Wenkebach). Observing the rhythm strip from the first P wave, there is a gradually prolonging PR interval and the P wave that follows the 6th QRS complex is blocked.
Management
Common causes of bundle branch block
Tachycardia: general approach
Tachyarrhythmias may present with significant symptoms and haemo- dynamic compromise. The approach to patients depends upon the following factors:
The effect of the rhythm on the patient
Record an ECG/rhythm strip and treat immediately with synchronized DC shock
Diagnosing the arrhythmia
The main distinctions to make are:
Investigations for patients with tachyarrhythmias
| 12-lead ECG and rhythm strip | • Regular vs. irregular rhythm • Narrow vs. broad QRS complex |
| Blood tests | • FBC, biochemistry, glucose (urgently) • Ca2+, Mg2+ (especially if on diuretics) • Biochemical markers of myocardial injury |
| Where appropriate | • Blood cultures, CRP, ESR • Thyroid function tests • Drug levels • Arterial blood gases |
| Chest X-ray (CXR) | • Heart size • Evidence of pulmonary oedema • Other pathology (e.g. Ca2+ bronchus→AF, pericardial effusion→sinus tachycardia, hypotension ± AF) |
Tachycardia: emergency management
History
Previous cardiac disease, palpitations, dizziness, chest pain, symptoms of heart failure and recent medication. Ask specifically about conditions known to be associated with certain cardiac arrhythmias (e.g. AF—alcohol, thyrotoxicosis, mitral valve disease, IHD, pericarditis; VT—previous MI, LV aneurysm).
Examination
BP, heart sounds and murmurs, signs of heart failure, carotid bruits.
Management (Fig. 10.5)
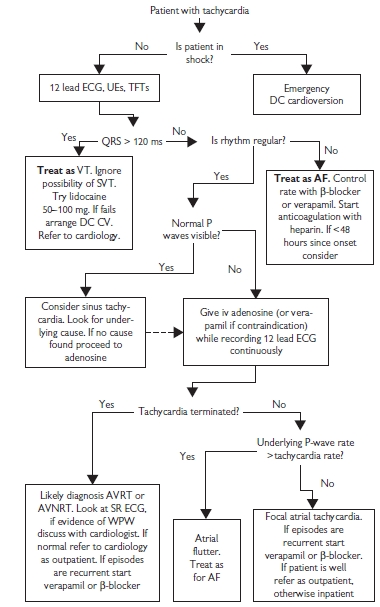
Fig. 10.5 Guidelines to the safe management of arrhythmias in the emergency department (adapted from Barts and the London NHS Trust A+E guidelines). CV = cardioversion; UEs = urea and electrolytes.
Haemodynamically unstable patients
Tachyarrhythmias causing severe haemodynamic compromise require urgent correction, usually with external defibrillation. Drug therapy requires time and haemodynamic stability.
 PaO2 (partial pressure of oxygen in the arterial blood),
PaO2 (partial pressure of oxygen in the arterial blood),  PaCO2 (partial pressure of carbon dioxide in the arterial blood), acidosis or
PaCO2 (partial pressure of carbon dioxide in the arterial blood), acidosis or  K+. Give Mg2+ (8 mmol IV stat) and shock again. Amiodarone 150–300 mg bolus IV may also be used.
K+. Give Mg2+ (8 mmol IV stat) and shock again. Amiodarone 150–300 mg bolus IV may also be used.Haemodynamically stable patients
Tachyarrhythmias: classification
Fast heart rates can be classified in various ways; however, an anatomical approach should be used, which can then be subdivided mechanistically. This provides a simple foundation for understanding the ECG appearance and the tachycardia mechanism.
Atrial tachyarrhythmias
These are contained completely in the atria (or SAN) and are characterized by:
Atrioventricular tachyarrhythmias
These are dependent on activation between the atrium and ventricle (or AV node). They are characterized by:
Ventricular tachyarrhythmias
These are contained completely in the ventricle and are characterized by:
Features of a broad complex tachycardia suggesting ventricular origin
Supraventricular causes of a broad complex tachycardia
ECG diagnosis of tachyarrhythmias
By following simple rules when interpreting the ECG, any tachycardia can be classified to the categories described earlier; however, the ECG should always be considered in the clinical context. A broad complex tachycardia (BCT) must always be diagnosed as VT in the acute setting, as treating such patients incorrectly may be fatal. View the ECG in both tachycardia and the patients’ usual rhythm to make a diagnosis (e.g. may see features of WPW). For narrow complex tachycardias (NCTs), use carotid sinus massage or adenosine boluses to see the underlying atrial rhythm.
A simple approach follows (Fig. 10.6):
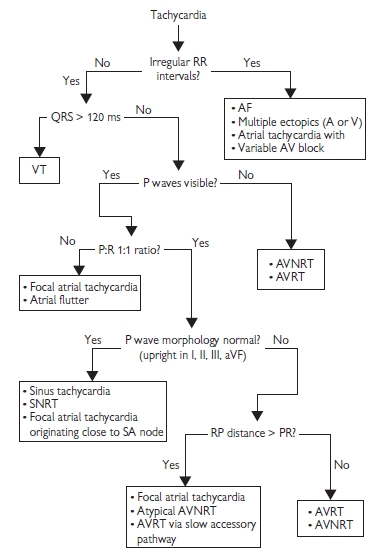
Fig. 10.6 ECG diagnosis of tachycardia.
1. Is the tachycardia regular?
Grossly irregular RR intervals regardless of other ECG features indicate AF (or VF; however expect the patient to be unconscious!). A slight irregularity can occur in other tachycardias, particularly at their onset. Alternatively, multiple atrial and/or ventricular ectopic beats or atrial tachycardia with variable AV block can give irregularity.
2. Is the QRS complex broad (>120 ms)?
Yes—ventricular in origin, no—supraventricular.
SVT should only be considered for a BCT when there is strong clinical suspicion (e.g. young patient, no previous cardiac history, normal RV and LV function, no accompanying cardiovascular compromise) and after discussion with senior colleagues. NB: Look at the SR ECG (if available) for pre-existing bundle branch block or pre-excitation (suggesting an accessory pathway).
3. Identify P waves, their morphology and P:R ratio
4. Response to AV block (adenosine or carotid massage)
If a rapid P-wave rate persists despite induced AV nodal block, then the tachycardia is independent of the AV node, i.e. macro-re-entrant or focal atrial tachycardia and SNRT. If tachycardia is terminated by AV nodal block, it is either AVRT or AVNRT (rarely, junctional tachycardia). Focal atrial tachycardia and SNRT may also be terminated by adenosine, not due to AV nodal block, but because they are adenosine sensitive.
Supraventricular tachycardia (see Fig. 10.7)
This section deals with the diagnosis and pharmacological management of individual SVTs. Their mechanisms and ablation are discussed in detail in Chapter 11.
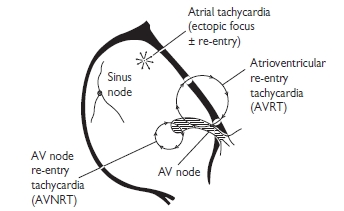
Fig. 10.7 Types of supraventricular tachycardia. Reproduced with permission from Ramrakha P, Moore K, and Sam M (2010). Oxford Handbook of Acute Medicine. 3rd ed. Oxford: Oxford University Press.
Sinus tachycardia
Defined as a sinus rate >100/min, this may be physiological (e.g. exercise or emotion) or pathological. Look for and treat the underlying cause—anaemia, drug related (e.g. caffeine, cocaine, salbutamol, etc.) hyperthyroidism, pain, hypoxia, pyrexia, or hypovolaemia. If no underlying cause is found, consider SNRT or focal atrial tachycardia as alternative diagnoses. These will be paroxysmal in nature, have sudden onset or offset and are usually terminated by IV adenosine. If no underlying cause is found, it may be termed inappropriate sinus tachycardia. β-blockers are useful for symptomatic persistent inappropriate sinus tachycardia, and vital in controlling the sinus rate in hyperthyroidism or heart failure, or post MI.
Sinus nodal re-entrant tachycardia
This is a rare cause of narrow complex tachycardia due to a micro re-entry circuit within the SAN. ECG is identical to sinus tachycardia, making diagnosis difficult. β-blockers or calcium-channel antagonists are the first-line treatment. Modification of the SA node by radiofrequency ablation (RFA) is reserved for drug-refractory cases or those not wishing to take drugs.
| Regular tachycardia | Irregular tachycardia |
| • Sinus tachycardia • SNRT • Atrial tachycardia ( see Atrial tachycardia, p. 496 ). • focal atrial tachycardia • macro-re-entrant atrial tachycardia (atrial flutter). • AVRT (i.e. with accessory path, e.g. WPW) (see Atrioventricular re-entrant tachycardia (AVRT), p. 498 ) • AVNRT (see Atrioventicular nodal re-entrant tachycardia (AVNRT), p. 498 ) | • Atrial fibrillation (see Atrial fibrillation, p. 500 ) • Atrial flutter with variable AV block • SR with frequent atrial or ventricular ectopic beats |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


