Primary percutaneous coronary intervention (PCI) is the preferred reperfusion method in patients with ST-elevation myocardial infarction (STEMI) if it can be performed in a timely manner in high-volume centers. Regional STEMI networks improve timely access to PCI but are frequently criticized for being single center. To determine if results of regional STEMI systems could be replicated and achieve similar outcomes in 2 separate geographic regions, we examined the prospective databases of 2 large regional STEMI networks that use identical standardized protocols and integrated transfer systems. The Minneapolis Heart Institute (MHI) database included 2,266 patients with STEMI from 31 hospitals (498 at the PCI hospital, 1,033 transferred from 11 hospitals <60 miles away, and 735 transferred from 19 hospitals 60 to 210 miles away). The Iowa Heart Center (IHC) database included 1,206 patients with STEMI from 24 hospitals (710 at the PCI hospital, 266 transferred from 10 hospitals <60 miles away, and 230 transferred from 13 hospitals 60 to 120 miles away). Median total door-to-balloon times for the PCI hospital, zone 1, and zone 2 patients were 64, 95, and 123 minutes for the MHI and 59, 102, and 136 for the IHC (p <0.05 for each comparison between MHI and IHC). Overall in-hospital, 30-day, and 1-year mortalities was 4.8%, 5.4%, and 8.0% respectively (p = NS for each comparison between MHI and IHC). In conclusion, the use of identical protocols in 2 large regional STEMI systems in geographically separate locations produced nearly identical outcomes, adding to evidence that regional STEMI centers expand timely access to PCI.
For patients with ST-elevation myocardial infarction (STEMI) transferred for primary percutaneous coronary intervention (PCI), current American College of Cardiology/American Heart Association and European Society of Cardiology STEMI guidelines recommend a total door-to-balloon (D2B) time of <120 minutes. However, United States data have consistently shown that a minority of patients with STEMI transferred for PCI meet these time-to-treatment guidelines. Data from the National Cardiovascular Data Registry from 2005 to 2006 indicated the median total D2B time in patients with STEMI transferred for primary PCI was 152 minutes (interquartile range 116 to 211) and only 28% had a total D2B time <120 minutes, with only 9% having a D2B time <90 minutes. Recently, regional STEMI networks have demonstrated that timely transfer of patients with STEMI for primary PCI is safe and effective. However, it is difficult to disseminate innovative health care delivery models. Our objective was to determine if a successful regional STEMI system using a standardized protocol could be replicated and achieve similar outcomes in 2 separate geographic regions.
Methods
The Minneapolis Heart Institute (MHI) is a group of 61 cardiovascular specialists with a practice centered at Abbott Northwestern Hospital, a 619-bed hospital in Minneapolis, Minnesota, with referral relations with community hospitals throughout Minnesota and Wisconsin. The Iowa Heart Center (IHC) is a group of 50 cardiovascular specialists practicing at Mercy Medical Center, a 567-bed hospital in Des Moines, Iowa, with referral relations with community hospitals in Iowa.
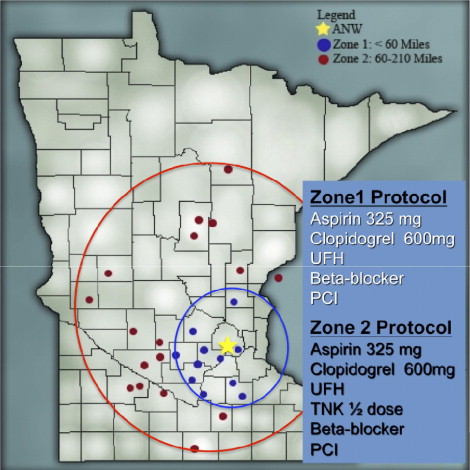
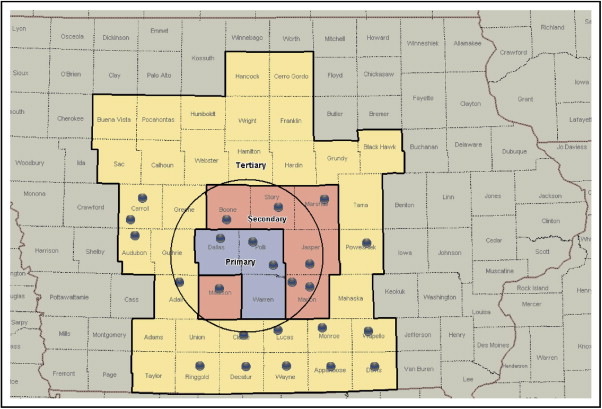
The MHI level 1 program commenced in March 2003 and the design and initial outcomes have been previously reported. Thirty referring/community hospitals participate in the MHI level 1 program. Currently there are 11 hospitals within 60 miles of Abbott Northwestern Hospital and 19 hospitals 60 to 210 miles of Abbott Northwestern Hospital, which are designated as zone 1 and 2 hospitals, respectively ( Figure 1 ). The IHC level 1 program began in February 2004 using a protocol modeled a priori after the MHI level 1 program. Currently there are 10 hospitals within 60 miles of Mercy Medical Center and 13 hospitals 60 to 120 miles of Mercy Medical Center, which are designated as zone 1 and 2 hospitals, respectively ( Figure 2 ) .
At the MHI, detailed data on baseline clinical characteristics, times to treatment, laboratory measurements, electrocardiographic values, angiographic details, and mortality are prospectively collected from medical records and entered in a dedicated Microsoft Access database (Microsoft, Redmond, Washington). Patient medical records were reviewed and co-morbid conditions listed under medical history, such as hyperlipidemia and hypertension, indicated the presence of the condition as baseline. Patients are enrolled in long-term follow up for 5 years. Mortality at 30 days, 1 year, and 5 years is abstracted from hospital electronic medical records (Excellian, Madison, Wisconsin), patient/family telephone calls, and/or the Social Security Death Index.
The IHC level 1 program uses CARIS (Mercy Medical Center, Des Moines, Iowa), the cardiac catheterization laboratory record-keeping system, and medical records to collect demographic characteristics, treatment times, clinical and angiographic information, adverse events, and mortality. In 2007 the IHC joined the National Cardiovascular Data Registry and began routinely collecting more detailed information. Out-of-hospital mortality was obtained from the Social Security Death Index for this investigation. The present analysis includes variables that were available in the 2 databases using similar definitions.
Inclusion and exclusion criteria for the MHI and IHC are identical, except for the time from symptom onset to presentation. Patients with STEMI or new left bundle branch block who presented within 24 hours of symptom onset were included in the MHI level 1 program and those who presented within 12 hours of symptom onset were included in the IHC level 1 program. No patients were excluded from either program because of a poor clinical prognosis for reasons such as advanced age, cardiogenic shock, or out-of-hospital cardiac arrest. Patients were excluded only if the emergency physician believed the patient was not a candidate for reperfusion therapy for reasons such as advanced metastatic cancer or end-stage dementia.
A detailed description of the MHI standardized treatment protocol has been described elsewhere. Briefly, patients who present at a zone 1 hospital receive aspirin 325 mg, clopidogrel 600 mg, unfractionated heparin, β blocker (unless contraindicated), and transfer for primary PCI. Because of expected delays owing to long distances, all patients in zone 2 are treated with a pharmaco-invasive strategy using the same protocol as in zone 1 with the addition of a decreased dose fibrinolytic, unless contraindicated, and transfer for immediate PCI. The treatment protocol at the IHC for the study period was identical to that of the MHI.
Patients are described based on regional level 1 program (MHI and IHC) and location of initial presentation (PCI center, zone 1, and zone 2). Baseline characteristics are presented for all patients with STEMI in the MHI level 1 program from March 2003 through December 2008 and for all patients in the IHC program after September 2007, when the hospital joined the National Cardiovascular Data Registry. Continuous data are presented as mean ± SD and were compared with t tests or 1-way analysis of variance. Proportions were compared with Pearson chi-square test. Time data are presented as median in minutes (25th and 75th percentiles) and were compared with Kruskal–Wallis tests. Kaplan–Meier methods were used to compute time-to-death curves and compared with log-rank tests. All analyses were performed using STATA 10.1 (STATA Corp., College Station, Texas).
Results
From March 2003 through December 31, 2008, 2,266 patients with STEMI or new left bundle branch block (within 24 hours of symptom onset) presented, representing 2,204 unique patients, at the 31 participating hospitals in the MHI level 1 program (498 at the PCI center, 1,033 at zone 1 hospitals, and 735 at zone 2 hospitals). From February 2004 through December 31, 2008, there were 1,206 consecutive encounters of STEMI or new left bundle branch block (within 12 hours of symptom onset), representing 1,176 unique patients, at the 24 participating hospitals in the IHC level 1 program (710 at the PCI center, 266 at zone 1 hospitals, and 230 at zone 2 hospitals).
Baseline clinical characteristics for unique patients stratified by regional STEMI program are presented in Table 1 . Patients in the MHI were older and more likely to have hyperlipidemia. Patients in the IHC had slightly more diabetes and were more often current smokers.
| Variable | MHI and IHC (n = 3,380) | MHI (n = 2,204) | IHC † (n = 1,176) | p Value, MHI vs IHC |
|---|---|---|---|---|
| Age (years), mean ± SD | 61.8 ± 13.9 | 62.5 ± 14.5 | 60.4 ± 12.7 | <0.0001 |
| Age ≥75 years | 21.2% (715/3,380) | 24.1% (532/2,204) | 15.6% (183/1,176) | <0.0001 |
| Men | 71.0% (2,399/3,380) | 71.5% (1,576/2,204) | 70.0% (823/1,176) | 0.35 |
| Hyperlipidemia | 50.2% (1,248/2,487) | 51.2% (1,125/2,199) | 42.7% (123/288) | 0.007 |
| Hypertension | 55.0% (1,369/2,490) | 55.6% (1,225/2,202) | 50.0% (144/288) | 0.07 |
| Diabetes mellitus | 15.8% (393/2,488) | 15.3% (337/2,200) | 19.4% (56/288) | 0.07 |
| Current smoker | 39.8% (983/2,473) | 38.5% (842/2,185) | 49.0% (141/288) | 0.001 |
⁎ Repeat admissions occurred in the Minneapolis Heart Institute and Iowa Heart Center systems during the study period. Baseline characteristics are presented for unique patients.
† Baseline characteristics available after the Iowa Heart Center joined the National Cardiovascular Data Registry.
Total time-to-treatment intervals comparing the 2 regional systems are presented in Table 2 and cumulative distribution curves in Figure 3 . Door-in/door-out and transport times were slightly faster for patients in the MHI compared to those in the IHC, but times from presentation at the PCI hospital to balloon were nearly identical in patients in zones 1 and 2. Overall, 76% of patients in zone 1 and 41% of patients in zone 2 met American College of Cardiology/American Heart Association and European Society of Cardiology guidelines of a total D2B time of <120 minutes. D2B times at the PCI center were slightly faster at the IHC compared to the MHI. Although median times were statistically different, total D2B times were only 5, 7, and 13 minutes different for the PCI Hospital, zone 1, and zone 2, respectively.
| MHI and IHC | MHI | IHC | p Value, MHI vs IHC | |
|---|---|---|---|---|
| Door in to door out | ||||
| Zone 1 | 49 (36, 66) | 49 (36, 67) | 50 (40, 61) | 0.99 |
| Zone 2 | 63 (50, 85) | 61 (48, 83) | 72 (57, 90) | 0.0001 |
| Transport time | ||||
| Zone 1 | 23 (16, 32) | 22 (16, 31) | 25 (19, 40) | 0.0001 |
| Zone 2 | 35 (27, 48) | 35 (26, 48) | 38 (30, 50) | 0.002 |
| Percutaneous coronary intervention hospital to balloon | ||||
| Zone 1 | 21 (17, 28) | 21 (17, 27) | 22 (17, 30) | 0.14 |
| Zone 2 | 20 (16, 27) | 20 (16, 26) | 22 (18, 29) | 0.0004 |
| Total door-to-balloon time | ||||
| Percutaneous coronary intervention hospital | 61 (46, 77) | 64 (44, 83) | 59 (46, 71) | 0.02 |
| Zone 1 | 97 (83, 118) | 95 (81, 117) | 102 (90, 121) | 0.0008 |
| Zone 2 | 127 (105, 154) | 123 (101, 152) | 136 (122, 167) | 0.0001 |
In-hospital, 30-day, and 1-year mortalities are listed in Table 3 . There were no significant differences between patients in the MHI and those in the IHC in mortality for any zone of presentation. Overall, in-hospital mortality was 4.8%, 30-day mortality was 5.4%, and 1-year mortality was 8.0%. Log-rank tests for time to death indicated no significant differences between the Level 1 programs (p = 0.22; Figure 4 ) or the zone of presentation (p = 0.20; Figure 5 ).



