18.4 ATRIAL FLUTTER WITH 2:1 CONDUCTION
The pathophysiology of atrial flutter is complex, and beyond the scope of this chapter (See Chapter 20). Overall, it is characterized by rapid atrial depolarization generated by an electrical circuit that circles the tricuspid annulus at 300 bpm. However, there is usually 2:1, 3:1, or 4:1 conduction across the AV node. Consequently, the ventricular response is usually some multiple of the flutter rate (in the absence of AV node dysfunction or antiarrhythmic drugs that slow the flutter circuit and AV conduction). For example, 2:1 flutter will usually manifest a ventricular response of 150 bpm; 3:1 flutter will usually manifest a ventricular response of 100 bpm; and 4:1 flutter will have a ventricular response of 75 bpm.
As a rule, whenever a narrow complex tachycardia is seen at a rate of 140–160 bpm, atrial flutter with 2:1 conduction should be suspected. With 2:1 conduction, the classic “saw-tooth” pattern may not be apparent, especially given that there will be only two flutter waves between QRS complexes that are narrowly-spaced (Figure 18.2). Flutter waves are best seen in leads V1 and II, although inspection of all leads is important. In addition, they should be completely uniform and occur at a regular rate, usually at 300 beats/min.
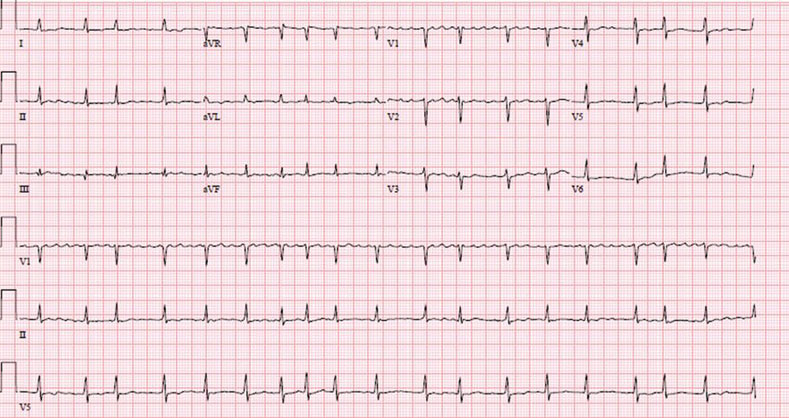
Atrial flutter is often misdiagnosed and overlooked. It may be very difficult to discern atrial flutter from atrial tachycardia with 2:1 conduction (often manifested by digitalis toxicity) (Figure 18.3). The atrial morphology in these two distinct arrhythmias is similar. However, treatment of these two disorders is different – one requiring some combination of anticoagulation, rate-controlling agents, and/or possibly radiofrequency ablation, and the other simply the cessation of digitalis, if toxicity is suspected. This illustrates the importance of a clinical history and medication review when faced with a stable narrow or wide complex tachycardia. In addition, it is important to note that coarse atrial fibrillation may be mistaken for atrial flutter with variable block (Figure 18.4). As above, flutter waves should be uniform in the same lead and occur at a regular rate, even in the presence of variable block.
18.5 PAROXYSMAL SUPRAVENTRICULAR TACHYCARDIAS
The paroxysmal supraventricular tachycardias (PSVTs) include the triad of AVNRT, AVRT, and atrial tachycardia. They are regular, narrow complex tachycardias with a rapid onset and offset, and occur across all age groups. AVNRT and AVRT require the AV node for the initiation and maintenance of the tachycardia, while atrial tachycardia is generated by a rapidly firing ectopic atrial pacemaker in the right or left atrium. These tachyarrhythmias are often difficult to distinguish on the surface 12-lead ECG, but there are certain clues that may help.
Figure 18.2 Regular, narrow complex tachycardia at approximately 120 bpm. This demonstrates atrial flutter with 2:1 AV conduction, along with RBBB. Flutter waves are best seen in lead V1, particularly between the 10th and 11th and 12th and 13th beats, where the rate transiently slows (arrows). The ventricular response is slightly less than expected for 2:1 flutter, which raises the suspicion of the concomitant use of a drug that acts on the AV node (e.g. beta-blocker, calcium-channel blocker, digitalis, amiodarone), often used in patients with atrial flutter.
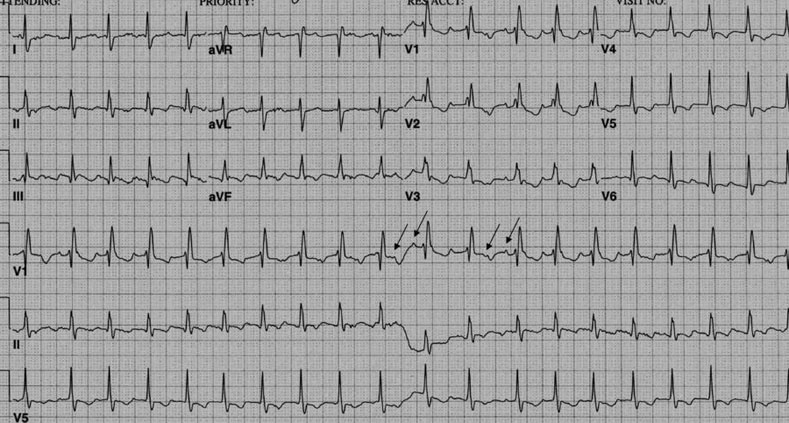
Figure 18.3 Atrial tachycardia with 2:1 block at a rate of 107 bpm in a patient who was taking digitalis. This arrhythmia often is confused with atrial flutter with 2:1 conduction. Ectopic atrial waves at a rate of 214 bpm are best seen in lead V1 (arrows, inset).
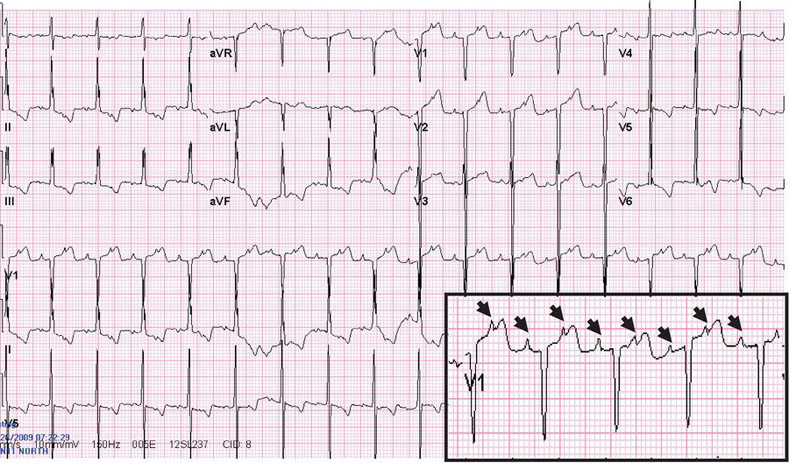
Figure 18.4 Coarse atrial fibrillation resembling atrial flutter. Note that the P waves in Lead V1 are not completely uniform and are often at a rate in excess of 300 bpm. thus excluding atrial flutter.
18.6 MECHANISMS
18.6.1 Atrioventricular Nodal Reentrant Tachycardia (AVNRT)
AVNRT is perhaps the most common of the PSVTs, and the rate is usually 180–200 bpm, but can range from 110–250 bpm. It is often seen in young adults without structural heart disease, 70% of which are women (pregnancy can often be a trigger for AVNRT). Some other triggers of AVNRT include nicotine, stimulants, exercise, or (paradoxically) hypervagotonic states. It is most often manifested by palpitations, although light-headedness and dyspnea can occur. Angina is less common. A sustained episode can theoretically result in syncope but, in general, PSVTs do not manifest with a loss of consciousness – in fact, if syncope is present after an episode of palpitations, ventricular tachycardia should strongly be suspected if coronary disease is present.
A simple diagram of AVNRT is illustrated in Figure 18.5. The AV is comprised of two sets of tissue, the so-called slow and fast pathways. During sinus rhythm, the sinus impulse travels down both the fast and slow pathways. The impulse that traverses the fast pathway enters the His-bundle prior to the impulse that is traveling down the slow pathway. As such, the slow pathway is rendered refractory and the impulse in that pathway is terminated, while the impulse in the His-bundle depolarizes the ventricles.
Figure 18.5 A Normal conduction system of the heart. B With AVNRT, conduction travels down the slow pathway of AV node and retrogradely up the bypass tract (fast pathway). (See Color plate 18.1). (Source: Wang, PJ and Estes NA. Supraventricular Tachycardia. Circulation 2002: 106: e206–208. Reproduced with permission of Wolters Kluwer Health).
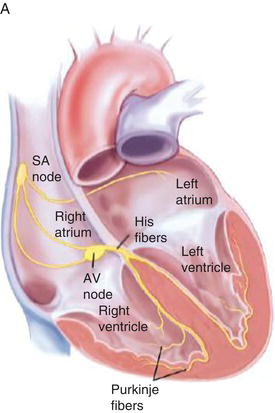
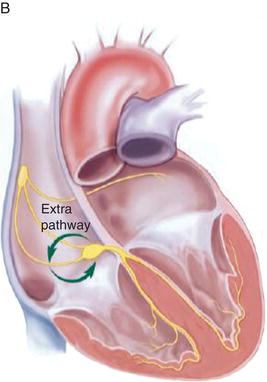
One important feature of these pathways is their relative refractory time. The fast pathway has a longer refractory period than the slow pathway. This is important in the initiation of typical AVNRT. A properly and specifically timed premature atrial complex (PAC) enters the AV node, but must travel down the slow pathway, given that the fast pathway (with a longer refractory period) will still be refractory from the prior sinus impulse. By the time the impulse reaches the His-bundle, the fast pathway has recovered, and the impulse will travel both retrogradely up the fast pathway and down the His-bundle into the ventricles. As a consequence, both a QRS complex (from normal His-Purkinje depolarization) and a retrograde P wave (from retrograde, or reverse travel up the AV node into the atria) are often witnessed (Figure 18.1). This circuit then perpetuates itself with subsequent antegrade conduction back down the slow pathway and retrograde conduction up the fast pathway. AVNRT may terminate spontaneously or another PAC may disrupt the cycle.
18.6.2 Atrioventricular Reentrant Tachycardia (AVRT)
AVRT is similar in pathophysiology to AVNRT, with the exception that it incorporates
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


