Aortic Valve Disease
Brian R. Lindman
Suzanne V. Arnold
High-Yield Concepts
LVOT dimension is a significant source of error when measuring AVA
Make sure the numbers are internally consistent (AVA, gradients, LVEF)
Subvalvular obstruction: Evaluate flow through the LVOT
Low-dose dobutamine test is helpful in patients suspected of having severe AS in the setting of low flow, low gradients
LV size, shape, and function are helpful in determining acute (normal LV size) versus chronic AR (dilated LV)
Key Views
Parasternal long axis—initial screening for AS severity (ability of valve to open, calcification) and AR severity (width of jet, LV dimensions); LVOT measurement
Parasternal short axis—AoV morphology
Apical long axis and apical five-chamber views—quantitative assessment of AS and AR: LVOT and AoV gradients, AR PHT using Doppler
Apical four chamber—LV dimensions and LV function for AR chronicity
TEE—higher resolution views for valve morphology, planimetry for AVA, AR severity
Severity of Aortic Stenosis
See Table 9-1.
Table 9-1 Severity of Aortic Stenosis | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||
Severity of Aortic Regurgitation
See Table 9-2.
Table 9-2 Severity of Aortic Regurgitation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Anatomy
Leaflets
The normal aortic valve (AoV) is trileaflet.
A bicuspid valve occurs in 1% to 2% of the population, unicuspid and quadricuspid valves are rare. The abnormal leaflet number may cause inherent valvular stenosis and regurgitation.
Annulus
The leaflets form semi-lunar attachments at the annulus forming a “crown”-like interlocking of ventricular and arterial tissue.
They also attach at the sinotubular junction.
Sinuses of Valsalva
As the proximal aortic root meets the left ventricular outlet there are three sinuses that bulge out and form the supporting structure for the corresponding aortic valve leaflets.
The sinuses and corresponding valve leaflet (or cusp) are named according to the origin of the coronary arteries.
Two sinuses give rise to coronary arteries (right and left) while the third, lying immediately adjacent to the mitral valve, does not (non).
Sinotubular junction
The place where the superior portion of the sinuses narrows and joins the proximal tubular portion of the ascending aorta.
Aortic Stenosis
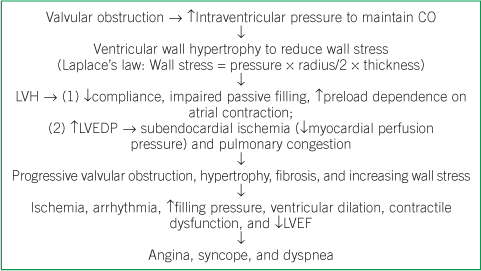
Pathophysiology
The pathophysiology for aortic stenosis (AS) involves both the valve and the ventricular adaptation to the stenosis. Within the valve, there is growing evidence for an active biologic process that begins much like the formation of an atherosclerotic plaque and eventually leads to calcified bone formation.
Etiology and morphology
See Table 9-3 and Figure 9-1.
Table 9-3 Etiology and Morphology of Aortic Valve Disease
Etiology
Prevalence, presentation, and associated features
Normal
- Asymptomatic
Calcific/Degenerative
- Most common cause in the United States
- Presents in seventh to ninth decades (mean age mid-70s)
- Risk factors similar to CAD
- Calcification leading to stenosis affects both trileaflet and bicuspid valves
Bicuspid
- 1–2% of population (the most common congenital lesion)
- Presents in sixth to eighth decades (mean age mid-late 60s)
- More prone to endocarditis than trileaflet valves
- Associated with aortopathies (i.e., dissection, aneurysm, coarctation)
Rheumatic
- Most common cause worldwide, much less common in the United States
- Presents in third to fifth decades
- Almost always accompanied by mitral valve involvement
Adapted from Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16(7):777–802, with permission from Elsevier.
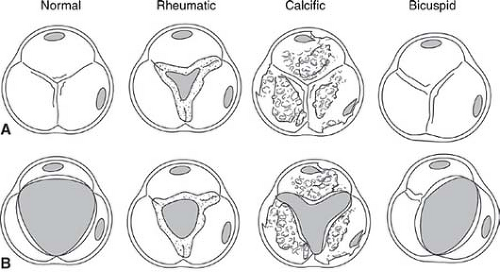
Figure 9-1. Typical appearance of aortic valve in diastole (row A) and systole (row B) suggestive of underlying etiology. (Adapted from C. Otto, Principles of Echocardiography, 2007.)
Echocardiographic assessment of AS
2D assessment
Leaflets
Motion of the valve
Aortic valve area (AVA) can be planimetered in the parasternal short-axis view—this is most often only possible in TEE studies using a side-by-side zoomed short-axis 2D image with corresponding color Doppler image to ensure that correct margins are drawn.
Ensure that your visual estimate of valve orifice area corresponds with other measurements; if, for example, the valve appears to open fairly well but measured gradients are considerably higher than you would expect, there may be a supra/subvalvular obstruction. Conversely if the valve appears calcified and stenotic; however, the recorded gradients are lower than expected consider: (1) Doppler acquisition not parallel to flow, (2) low flow, low gradient, reduced LVEF AS, (3) low flow, low gradient, normal LVEF AS (discussed later).
Eccentric closure, doming, and prolapse of the valve in the parasternal long-axis view suggest the presence of a bicuspid valve.
Bicuspid aortic valves (BAVs)—most commonly due to fusion of the right and left coronary cusps (∼80%) or fusion of the right and non-coronary cusps (∼20%); bicuspid valves have an elliptical orifice during systole; they can easily be mistaken for trileaflet valves during diastole, particularly when a raphe is present. Leaflet doming is present because of restricted leaflet motion. Valvular regurgitation is usually highly eccentric and posteriorly directed (Fig. 9-2E). There may be associated aortic abnormalities (dilation of aortic root, coarctation).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


