Aortic Stenosis after a Modified Ross Procedure
The patient is a 23-year-old man with a history of aortic stenosis, status post modified Ross procedure at age 9, complicated by complete heart block requiring a pacemaker, which was subsequently converted to a biventricular pacemaker 6 years ago and a battery change 2 years ago. His only complaints have been that he fatigues easily and experiences occasional light-headedness with an increase in activity such as power walking.
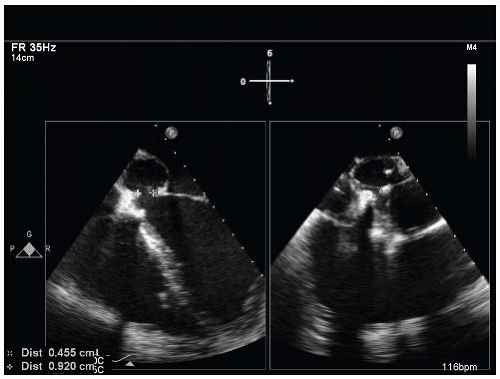
Six years ago, a small fistula was found near his left ventricular outflow tract (LVOT). A recent cardiac catheterization demonstrated that his left ventricular outflow fistula had enlarged (Fig. 3-1).
A. Intracardiac shunt
B. Pseudoaneurysm
View Answer
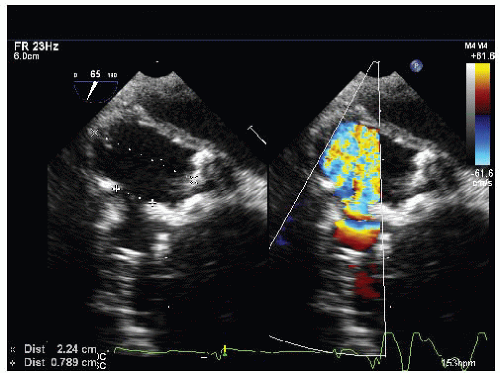
ANSWER 1: B. Flow is seen between the aortic outflow tract and the aortic root. The flow enters a confined space and does not appear to communicate with another intracardiac structure. A computed tomographic angiogram confirmed a 3.5-cm pseudoaneurysm extending from the aortic outflow tract in a posterior direction and an aortic root measuring up to 4.8 cm in maximal diameter.
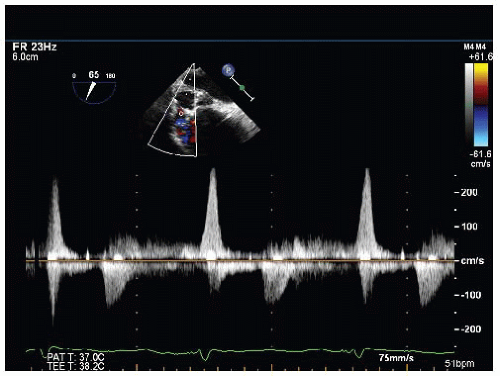
QUESTION 2. The aneurysm does not communicate with another chamber; thus the flow through the aneurysm is going back and forth. In Figure 3-3, the size of the aneurysm is the largest in:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree