Aortic and Peripheral Aneurysms
Eugene S. Lee
Kevin Lindholm
David L. Dawson
The term “aneurysm” comes from the Greek aneurysma, meaning “a widening.” Aneurysms are segments of arterial dilatation, usually caused by degenerative changes in the vessel wall. Continued weakening of the vessel wall can lead to aneurysm expansion and vessel rupture. Thrombus can develop in areas of reduced flow velocity within an aneurysm, but the amount of mural thrombus is not an indicator of rupture risk.1 Major predictors for rupture of an abdominal aortic aneurysm (AAA) are aneurysm diameter, female gender, chronic obstructive pulmonary disease (COPD), higher blood pressure, current tobacco use, cardiac or renal transplant, and critical wall stress.2 Rapid expansion of an AAA of greater than 0.5 cm within a 6-month interval has been considered a risk factor for rupture and justification for AAA repair. Mural thrombus rarely causes clinically significant problems in aortic aneurysms, but thrombosis and embolism are important causes of complications with peripheral artery aneurysms.3,4,5,6 Aneurysms can also cause complications due to compression of adjacent structures (e.g., nerves7 or veins8,9,10).
An AAA may be palpable, and aortic palpation is a crucial component of a thorough vascular physical examination. However, the accuracy of detecting an AAA on physical examination is unreliable. Studies have found that the sensitivity of abdominal palpation for determining the presence of an AAA can range from 29% for diameters of 3.0 to 3.9 cm to 76% for large AAAs with diameters over 5.0 cm.11 Ultrasonography, on the other hand, has a sensitivity and specificity for AAA detection approaching 100%.2 Hence, the need for vascular sonography in the detection of AAA is crucially important.
Notably, evaluation of the aorta was one of the earliest applications of vascular sonography.12,13 Because of its safety, low cost, and reliability, ultrasound remains the imaging modality of choice for screening, confirmation of a physical examination finding suggesting the presence of an aneurysm, or follow-up measurements of aneurysms under clinical surveillance.14,15 Ultrasound imaging is the best noninvasive study for detecting an AAA, though many aneurysms are found incidentally with other imaging studies.
ABDOMINAL AORTIC ANEURYSMS: INDICATIONS AND APPLICATIONS
The infrarenal segment of the abdominal aorta is the most common location for an arterial aneurysm. The presence of an AAA is associated with advancing age, family history of AAA, male sex, and a history of current or past tobacco use.2 The diagnosis of AAA is made when the aortic diameter is ≥3.0 cm. An AAA is typically asymptomatic until rupture. When rupture does occur, either sudden death ensues or there is immediate onset of excruciating back and abdominal pain. Over 16,000 deaths occur annually from AAA rupture, and this is the 15th leading cause of death in the United States today.
In general, an aortic diameter of ≥5.5 cm is an indication for elective surgical repair.2 Elective treatment is performed to prevent rupture or thromboembolism.16 Repair can be done by open surgical replacement of the diseased arterial segment with an interposition graft or by endovascular aortic repair (EVAR). The endovascular approach has become the primary means for AAA treatment for patients with suitable anatomy, which is generally assessed by CT angiography. The lower mortality risk, lower early complication rate, and quicker recovery from EVAR make it preferred over open surgical repair. Further, multiple studies have confirmed the benefit of EVAR over open repair for emergency treatment of ruptured aneurysms. Open repair of a ruptured AAA carries a mortality rate of 42%, compared to emergency EVAR with a mortality rate of 30%.17 Thus, EVAR has also become the treatment of choice for ruptured AAA if the anatomy permits.
Anatomic Patterns
There are several anatomic patterns of AAAs. The descriptions are clinically relevant, as different techniques for repair are used for different types of aneurysms. The most common type is the infrarenal aneurysm, which is located distal to the renal artery origins with a neck of nondilated aorta between the aneurysm and the renal arteries. Infrarenal aneurysms may be repaired with commercially available endografts (See Chapter 16, Fig. 16.5) or by open surgical repair. The aorta may be clamped and sutured distal to the renal arteries with open surgical repair of an infrarenal aneurysm (Fig. 15.1).
Juxtarenal aneurysms have no intervening segment of normal aorta distal to the renal arteries. With this type of aneurysm, endovascular repair is possible with specialized techniques or fenestrated grafts. Commercial fenestrated grafts became available in the in the United States in 2012, with the initial FDA approval for the treatment of AAAs with short infrarenal aortic necks (4 to 15 mm). The proximal segments of these custom-fabricated endografts have holes (fenestrations) so that stents can be placed into the renal arteries, thus providing secure proximal fixation.18 Endovascular repair also makes use of specialized techniques, including the use of endostapling (where the proximal graft is anchored to a short aortic neck), snorkeling, or the use of endografts that do not rely solely on proximal stent fixation. Open surgical repair is more common for the treatment of juxtarenal aneurysms, but suprarenal or supraceliac aortic clamping is required, increasing the risk of visceral ischemia during the procedure.
Suprarenal aneurysms involve the aorta above the renal arteries, and the renal arteries arise from an aneurysmal segment. Suprarenal aneurysms require concomitant renal or visceral artery reconstruction when open surgical repair is performed. Use of fenestrated or branched endografts for suprarenal aneurysms is an option in some cases, though still experimental in the United States in 2014.
Thoracic aortic aneurysms (TAA) cannot be evaluated by ultrasound due to imaging limitations from the air in the chest (ultrasound is not transmitted through the lungs). Thoracoabdominal aortic aneurysms (TAAA) can involve both the thoracic and abdominal segments of the aorta.19 Repair of a TAAA requires exposure of the aorta above and below the diaphragm. TAAAs are functionally classified considering the nature of surgical repair required.20 Suprarenal aortic aneurysms that extend proximally to include the celiac artery origin require aortic clamping and the proximal anastomosis be performed in the chest. This is a Type IV TAAA. Though the thoracic aorta cannot be visualized with ultrasound imaging, the possibility of a TAAA should be considered if the proximal extent of aneurysmal dilatation cannot be defined on an abdominal ultrasound examination. CT or MR angiography is needed for complete evaluation of any TAAA or suprarenal aneurysm.
Pathogenesis
Aneurysms can also be described by their morphology. The most common shape is fusiform—widest in the middle and tapering proximally and distally (Fig. 15.2). This descriptor is derived from the Latin fusus, meaning “spindle.” A more focal dilation is described as a saccular aneurysm. A saccular aneurysm resembles a small sac or outpouching. This term is derived from sacculus, the Latin word for small pouch or sac.
The most common cause of aortic and iliac artery aneurysms is a chronic degenerative change in the arterial wall leading to a focal arterial dilation. Though patients with aneurysms share risk factors with patients who have atherosclerosis,21 the term “atherosclerotic aneurysm” is no longer used, as the pathophysiology of AAA is distinct from atherosclerosis. The pathogenesis of an AAA is based on four broad cellular and molecular processes that include proteolytic degradation of the aortic wall, inflammation and immune responses, biomechanical wall stress, and molecular genetics.22 Multiple factors play a role in localized hemodynamic stress, and genetic predisposition attracts inflammatory cells (monocytes and lymphocytes) to the area of the infrarenal aorta.
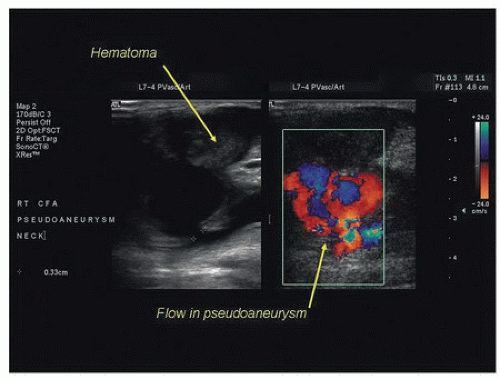
Pseudoaneurysms, or “false” aneurysms, are the result of disruption of the arterial wall from injury or infection, or breakdown of an arterial anastomosis, such as the anastomosis of a prosthetic graft to a native artery (Fig. 15.3). Pseudoaneurysms tend to be saccular in appearance. Aneurysms occurring at, or adjacent to, the anastomosis of a graft (“juxta-anastomotic” or “para-anastomotic” aneurysms) are often pseudoaneurysms from disruption of the anastomosis, but they can also represent late aneurysmal degeneration of the remaining native vessel.23,24 Juxta-anastomotic aneurysms are rare enough that routine, regular surveillance is not recommended after uncomplicated open aortic procedures, at least not for several years after the initial operation.25 Pseudoaneurysm formation at one or more anastomotic sites can be a late presentation of a prosthetic graft infection.23,26,27,28,29,30,31
Infection is an unusual cause for primary aneurysm formation, although the aorta, peripheral arteries, cerebral arteries, and visceral arteries (in descending order of frequency) can be affected by bacterial arteritis and false aneurysm formation. The most common causal pathogens are Staphylococcus and Streptococcus species. Imaging features of infected aneurysms include findings of a lobulated vascular mass, an indistinct irregular arterial wall, edema, or a perianeurysmal soft tissue mass. Perianeurysmal gas, aneurysm thrombosis, aneurysmal wall calcification, and disrupted arterial calcification have also been described with infected aneurysms, though these findings are less common.32
Threshold for AAA Treatment
Multicenter trials have found that there is no benefit for early surgical repair of small fusiform infrarenal AAAs (the most common type), compared to careful surveillance with serial ultrasound examinations.33,34 Small aneurysms can be safely observed.35 Based on a review of published data, the estimated average annual rate of rupture or acute expansion is almost nil for an AAA less than 4.0 cm in diameter.36 In a meta-analysis of 15,471 patients, small AAAs grew an average of 1.3 to 1.9 mm/year for 3.0 to 3.5 cm AAAs, 2.4 to 3.0 mm/year for 4.0 to 4.5 cm, and 3.6 mm/year for AAAs larger than 5.0 cm. Rupture rates of small aneurysms were found to be very low in this meta-analysis. The growth rates and rupture rates were found to be significantly higher in women than men.36
The Society for Vascular Surgery (SVS) guidelines for management of small aneurysms suggest serial ultrasound imaging at intervals that depend on aortic diameter.2 This strategy appears to be safe for men until the AAA reaches 5.5 cm in diameter, as the expected annual rupture rate is less than the risk of perioperative mortality with surgical repair observed in clinical trials.16,37,38,39 Repair is generally recommended if the expansion rate is greater than 0.5 cm in 6 months or if symptoms develop.40 Recommendations have been made to consider repair of AAAs at 5.0 cm in diameter for women, as rupture is more common in women with aneurysms, and female gender appears to be a risk factor for adverse outcomes.41,42,43
Because perioperative mortality with EVAR is less than with open repair, it has been suggested that EVAR could be considered at a smaller AAA size threshold. Two recently completed randomized controlled trials evaluated the efficacy of surveillance versus early EVAR for small AAAs. These trials found that mortality and rupture rates for AAAs less than 5.5 cm were low, and no clear advantage was shown with either an early or delayed EVAR strategy. Hence, the authors of both studies concluded that surveillance of small AAAs is safe if careful surveillance is possible.44,45,46
Screening and Ultrasound Diagnosis of AAA
Since AAAs are typically asymptomatic until rupture, screening for AAA is important. This allows AAA treatment in an elective setting. Physical examination is too insensitive to be relied upon for initial diagnosis, especially if the aneurysm is not large or if the patient is heavy,47 but over 90% of aortic aneurysms are infrarenal in location where ultrasound imaging is practical.
AAA screening has a demonstrated benefit. A large United Kingdom trial, the Multicentre Aneurysm Screening Study (MASS), was a randomized, controlled trial of over 65,000 population-based men 65 to 74 years of age who smoked at least 100 cigarettes in their lifetimes. One-half of the men were invited for AAA screening, while the control group was followed for clinical events but not invited for screening. The results of this multiyear study demonstrated the ability of screening to significantly reduce aneurysm-related deaths as well as reduce all-cause mortality.48,49,50 Recognizing the significance of this, Medicare has covered an aortic screening ultrasound (for new Medicare beneficiaries at risk) since 2007. Current recommendations call for a one-time ultrasound screening to be offered to men aged 65 to 75 years who have smoked 100 or more cigarettes in their lifetime or to men and women 50 years of age or older with a family history of AAA.14 In utilizing these criteria for screening a population at risk for AAA, a prevalence of 5.1% was detected in a contemporary series, which is similar to multiple other studies where the prevalence ranged from 3.9% to 7.2%.51
Aortic diameter measurements are used to diagnose an ectatic or aneurysmal aorta, stratify for risk of rupture, and guide the need for long-term follow-up. The normal diameter of the infrarenal aorta is generally less than 2 cm in transverse dimension. The aortic diameter is larger in men, and it increases
with body size and age.52,53 An aneurysm is diagnosed when the abdominal aortic diameter is 1.5 times the normal value or when the aorta is 3 cm or greater in diameter. The aorta is deemed “ectatic” if the aorta measures 2 to 3 cm in diameter (greater than normal aortic size but less than 1.5 times the diameter of the undiseased adjacent aorta). Ultrasound follow-up is recommended for patients with aortic diameters of 2.6 to 2.9 cm at 5-year intervals, 3.0 to 3.4 cm at 3-year intervals, and for those with aortas of 3.5 to 4.4 cm, annual follow-up is recommended. Patients with larger AAAs of 4.5 to 5.4 cm in diameter should be followed at 6-month intervals.2
with body size and age.52,53 An aneurysm is diagnosed when the abdominal aortic diameter is 1.5 times the normal value or when the aorta is 3 cm or greater in diameter. The aorta is deemed “ectatic” if the aorta measures 2 to 3 cm in diameter (greater than normal aortic size but less than 1.5 times the diameter of the undiseased adjacent aorta). Ultrasound follow-up is recommended for patients with aortic diameters of 2.6 to 2.9 cm at 5-year intervals, 3.0 to 3.4 cm at 3-year intervals, and for those with aortas of 3.5 to 4.4 cm, annual follow-up is recommended. Patients with larger AAAs of 4.5 to 5.4 cm in diameter should be followed at 6-month intervals.2
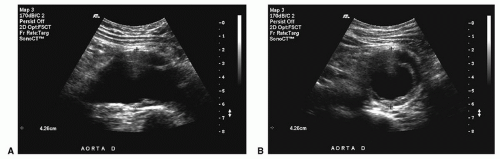
Ultrasonography is recommended for both initial screening and the diagnosis of AAA but is relatively imprecise in measuring aneurysm size. The Intersocietal Accreditation Commission Standards and Guidelines for Vascular Testing state that aneurysms should be measured at the widest point of the aorta from outer wall to outer wall (Fig. 15.4). The outer wall to outer wall measurement was found to have less intraobserver variability and has been suggested as the method for measuring AAA size in the large MASS trial.54 However, a more recent study has questioned the utility of outer to outer wall measurements and published data that interobserver reliability is greater with the inner wall to inner wall measurement.55
Ultrasound imaging may be limited in patients with large body habitus, overlying bowel gas, or those who are unable to cooperate with the examination. In these instances, an abdominal CT scan is more appropriate for making the initial diagnosis of AAA. CT is more reproducible for diameter measurement than ultrasound, and CT is the primary modality for surgical planning. However, in almost all other cases, ultrasound is the preferred modality for initial AAA diagnosis and follow-up.
Given the utility of ultrasonography in screening for AAAs, point-of-care examinations are being used more commonly, especially in underserved and rural areas where primary care clinics are performing AAA screening. The increasing availability of compact, low-cost, ultrasound systems is making point-of-care studies more commonplace, leading experts to believe that ultrasonography will be a basic skill in routine medical practice in the near future (see Chapter 27).56 The use of contrast-enhanced ultrasonography and 3D ultrasound have found some benefits in follow-up after EVAR, to detect endoleak or to find vascular branches (see Chapter 16), but these advanced applications are not particularly useful in the initial diagnosis of AAA.57
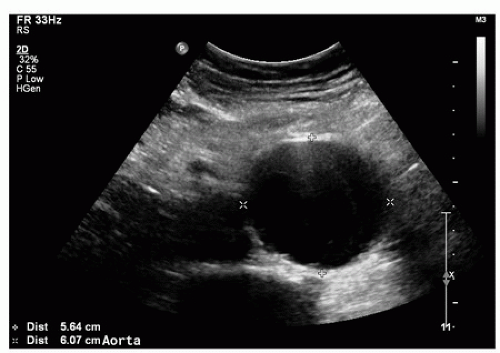 FIGURE 15.4. B-mode image of an abdominal aortic aneurysm in transverse view. The abdominal wall is the most superficial structure at the top of the image, and the vertebral column is deep to the aorta at the bottom of the image. Specular reflections from the deep and superficial walls of the aorta (+) are more distinct than those from the lateral walls (×). Therefore, the lateral resolution of ultrasound is less that the depth resolution, making accurate anterior-posterior (AP) diameter measurements easier to obtain.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|