Antiphospholipid Antibody Syndrome
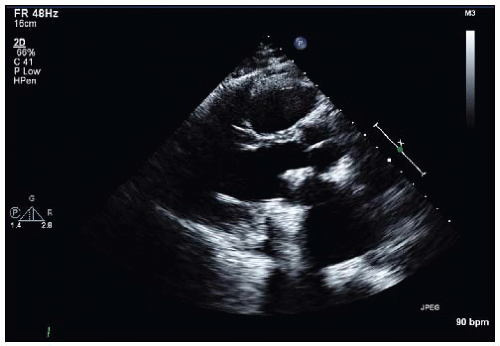
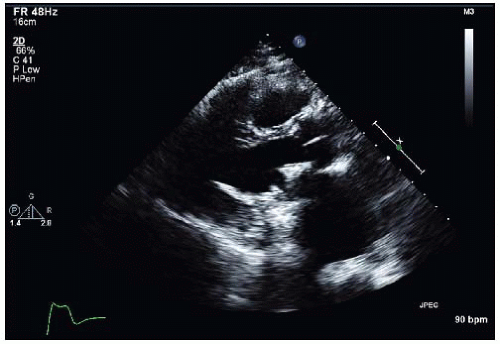
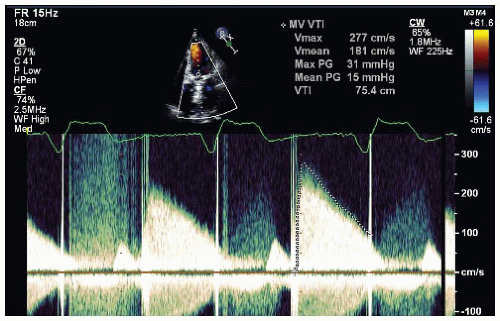
A 50-year-old woman with a history of antiphospholipid antibody syndrome, a history of ST segment elevation (Q wave) myocardial infarction involving the left anterior descending artery, history of recurrent deep vein thrombosis status post inferior vena cava filter, and who is status post mitral valve replacement presents with 1 week of increasing dyspnea on exertion, now with dyspnea at rest. Her prescribed medications include fondaparinux and clopidogrel. A transthoracic echocardiogram is performed (Figs. 31-1, 31-2 and 31-3), followed by a 3D transesophageal echocardiogram (Figs. 31-4 and 31-5).
QUESTION 1. The recommended treatment for this condition is:
A. Immediate surgery
B. Fibrinolytics
C. Plasmapheresis
D. Pulse steroids
E. More than one of the choices
View Answer
ANSWER 1: E. This patient has thrombosis of her prosthetic mitral valve. There is no consensus among the major societies for initial therapy for prosthetic valve thrombosis (PVT). Furthermore, in this case—and not addressed in the guidelines—is the value of steroids and plasmapheresis in the treatment of PVT associated with antiphospholipid antibody syndrome.1
The various guideline recommendations for PVT are summarized here:
American College of Cardiology/American Heart Association2:
Fibrinolytic therapy for a left-sided prosthetic valve obstructed by thrombus is associated with significant risks (cerebral emboli in 12% to 15% of cases) and is often ineffective. Fibrinolytic therapy in such patients is reserved for those in whom surgical intervention carries a high risk and those with contraindications to surgery. In patients with a “small clot” who are in NYHA functional class I or II, treatment with short-term intravenous UFH therapy or continuous infusion of fibrinolytic therapy may be considered.
European Society of Cardiology3:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree