The efficacy of the anticoagulation in preventing thromboembolic complications (TEC) and the usefulness of the CHA 2 DS 2 VASc score for assessing stroke risk during cardioversion of acute atrial fibrillation (AF) are unclear. Thus, our objectives were to assess the ability of the CHA 2 DS 2 VASc score to predict TEC and to evaluate the efficacy of anticoagulation in the prevention of TEC in Finnish CardioVersion (FinCV) study. The FinCV is a retrospective, multicenter study of 3,143 patients, who underwent 7,660 cardioversions for acute AF. The value of the CHA 2 DS 2 VASc score in predicting TEC was analyzed separately in cardioversions performed without and with anticoagulation. A total of 40 definite TEC (0.6%) occurred after 7,237 successful cardioversions and 1 stroke (0.2%) after 423 unsuccessful procedures. In 5,362 cardioversions performed without anticoagulation, the risk of definite TEC increased significantly from 0.4% in patients with a CHA 2 DS 2 VASc score of 0 to 1 to 2.3% in those with score of ≥5 (p <0.001 for trend). The C-statistic of the CHA 2 DS 2 VASc score was 0.72 (0.61 to 0.83) in predicting definite TEC in non-anticoagulated patients with first cardioversion. The incidence of definite TEC was significantly lower in 2,298 cardioversions performed during anticoagulation (0.1% vs 0.7%, p = 0.001), and the preventive effect of anticoagulation was significant in patients with a score of ≥2 (0.2% vs 1.1%, p = 0.001). In conclusion, CHA 2 DS 2 VASc score is a strong predictor of TEC in cardioversion of acute AF performed without anticoagulation. Importantly, periprocedural anticoagulation reduced the risk of TEC by 82%. The overall risk of these complications was low after failed cardioversion.
The CHA 2 DS 2 VASc score is the risk stratification scheme in everyday clinical practice to assess the need of anticoagulation in patients with atrial fibrillation (AF), but its value in predicting adverse events in patients who underwent cardioversion of acute AF has not been assessed. Anticoagulation therapy is recommended for patients with acute (duration ≤48 hours) AF and high risk for stroke with no specific CHA 2 DS 2 VASc score limits, but there is limited research data on the efficacy of anticoagulation in this acute setting. Our previous analysis of the Finnish CardioVersion (FinCV) study confirmed the high risk of stroke when cardioversion was performed without adequate periprocedural anticoagulation in patients with conventional stroke risk factors. In the present analysis, we sought to determine whether the CHA 2 DS 2 VASc score is useful to predict the risk of thromboembolic complications (TEC) after cardioversion of acute AF and whether anticoagulation prevents TEC in high- and low-risk patients. Third, we evaluated whether the CHA 2 DS 2 VASc score predicts failure of cardioversion, early recurrence of AF, and bradyarrhythmic complications.
Methods
The FinCV study ( ClinicalTrials.gov identifier: NCT01380574 ) is a multicenter retrospective study including patients who underwent cardioversion for acute AF. The study is a part of wider protocol in progress to assess acute cardiac procedures in Western Finland. Study protocol was approved by the Ethics Committees of the Hospital District of Southwest Finland and the National Institutes for Health and Welfare. Patients with a diagnosis of AF at 2 university hospitals from 2003 to 2010 and at 1 central hospital in 2010 were identified from institutional discharge registers by the International Classification of Diseases, Tenth Revision , code I48.0. The emergency clinic admission records were reviewed to include all patients with acute AF who underwent cardioversion within 48 hours from symptom onset during the study period. All patient records were reviewed with a standardized data collection protocol, and only patients >18 years and living in the hospital catchment area were included to ensure adequate follow-up data of 30 days after the cardioversion. The study hospitals are the only referral hospital responsible for acute care of patients with cardiac and stroke events in their catchment areas. Cardioversions were performed according to contemporary guidelines as previously described. Electrical cardioversions (90%) were performed under general anesthesia, and majority of pharmacologic cardioversions were performed using flecainide. In anticoagulated patients, cardioversions were performed during long-term warfarin treatment (98%) or under cover of heparins.
We identified 3,143 patients who underwent 7,660 cardioversions for acute AF. Cardioversions were divided into 4 groups according to the CHA 2 DS 2 VASc score of the patients: score ≤1, 2, 3 to 4, and ≥5. The risk of TEC in patients with and without anticoagulation was compared in these 4 groups. The independent predictors of TEC were sought, and the value of CHA 2 DS 2 VASc score and the CHADS 2 score in predicting TEC was evaluated. Finally, we evaluated whether CHA 2 DS 2 VASc score predicts failure of cardioversion, recurrence of AF after successful cardioversion, and bradyarrhythmic complications.
The primary end point of the study was TEC, which was defined as stroke or systemic embolism confirmed by imaging (magnetic resonance imaging or computerized tomography), surgery, or autopsy. Transient ischemic attack (TIA) was classified as probable TEC. Secondary end points were unsuccessful cardioversion, early recurrence of AF episode after successful cardioversion, and bradyarrhythmic complications after cardioversion. Cardioversion was defined as successful if sinus rhythm was obtained and patient was discharged in sinus rhythm. Early recurrence was assessed from patient records during the 30-day follow-up period. Bradyarrhythmia was defined as heart rate <40 beats/min and/or asystole >5 seconds immediately after the cardioversion.
Continuous variables are presented as means and SD or medians and interquartile range as appropriate and analyzed with the Student’s t test, Mann-Whitney U test, and Kruskal-Wallis test. Categorical variables are expressed as absolute numbers and percentages and analyzed with the chi-square test, Fisher’s exact test, and Cochran-Armitage test for trend. Multivariable logistic regression analysis with repeated measure option with covariates chosen according to our earlier reports was used in the evaluation of primary and secondary end points. Because the same patient could have repeated cardioversions during study period, only the first cardioversion of a patient was included in the receiver-operating characteristic (ROC) area under the curve analyses of CHA 2 DS 2 VASc and CHADS 2 scores. The method of DeLong was used to calculate the difference between these area under the curves of ROC curves. A 2-sided p value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS for Windows 22.0 software (IBM Corp., Armonk, NY) and SAS software, version 9.3 (SAS Institute Inc., Cary, NC).
Results
At the time of cardioversion, the mean age of patients was 62.2 ± 12.3 years, 2,798 (36.5%) were women, and the median CHA 2 DS 2 VASc score was 2 (interquartile range 1 to 3). The baseline characteristics of patients according to their CHA 2 DS 2 VASc scores are presented in Table 1 . The overall success rate of cardioversions was 94.5% (7,237 of 7,660), and 5,362 (70.0%) cardioversions were performed without anticoagulation.
| Characteristic | CHA 2 DS 2 VASc score | P value | |||
|---|---|---|---|---|---|
| 0-1 (n=3362) | 2 (n=1610) | 3-4 (n=1997) | 5-9 (n = 691) | ||
| Age (years) | 54.3 ± 10.3 | 63.4 ± 10.8 | 70.0 ± 8.5 | 74.8 ± 6.7 | < 0.001 |
| Women | 416 (12.4%) | 690 (42.9%) | 1174 (58.8%) | 518 (75.0%) | < 0.001 |
| Heart failure | 33 (1.0%) | 54 (3.4%) | 179 (9.0%) | 137 (19.8%) | < 0.001 |
| Hypertension | 762 (22.7%) | 913 (56.7%) | 1438 (72.0%) | 610 (88.3%) | < 0.001 |
| Diabetes mellitus | 24 (0.7%) | 124 (7.7%) | 361 (18.1%) | 233 (33.7%) | < 0.001 |
| Vascular disease | 250 (7.4%) | 468 (29.1%) | 974 (48.8%) | 523 (75.7%) | < 0.001 |
| Previous thromboembolism | 0 | 36 (2.2%) | 241 (12.1%) | 419 (60.6%) | < 0.001 |
| Implanted pacemaker | 102 (3.0%) | 101 (6.3%) | 105 (5.3%) | 83 (12.0%) | < 0.001 |
| First episode of atrial fibrillation | 794 (23.6%) | 315 (19.6%) | 445 (22.3%) | 141 (20.4%) | 0.01 |
| Electrical cardioversion | 2997 (89.1%) | 1445 (89.8%) | 1826 (91.4%) | 638 (92.3%) | 0.01 |
| Duration of symptoms < 12 hours | 1520 (45.2%) | 785 (48.8%) | 904 (45.3%) | 334 (48.3%) | 0.06 |
| Ventricular rate of atrial fibrillation (bmp) | 108.5 ± 26.9 | 109.6 ± 25.1 | 111.1 ± 33.4 | 114.5 ± 24.4 | < 0.001 |
| Anticoagulation therapy | 590 (17.5%) | 516 (32.0%) | 852 (42.7%) | 340 (49.2%) | < 0.001 |
| Beta-blockers | 2293 (68.2%) | 1327 (82.4%) | 1688 (84.5%) | 601 (87.0%) | < 0.001 |
| Class I antiarrhythmic drugs | 885 (26.3%) | 372 (23.1%) | 343 (17.2%) | 89 (12.9%) | < 0.001 |
| Class III antiarrhythmic drugs | 130 (3.9%) | 73 (4.5%) | 77 (3.9%) | 45 (6.5%) | 0.01 |
A total of 41 (0.5%) definite TEC occurred within 30 days after the cardioversion with a median delay of 2 days (range 1 to 27 days). Forty (0.6%) definite TEC occurred after 7,237 successful procedures, and patients were on anticoagulation therapy only during 2 of these cardioversions. The INR values of patients on oral anticoagulation ranged from 2.9 to 3.5 at the time of cardioversion and the thromboembolic event occurred at 2 and 23 days after cardioversion. A total of 423 cardioversions (5.5%) failed and 1 patient (0.2%) treated with periprocedural heparin had a stroke 2 days after failed cardioversion. This patient underwent spontaneous conversion to sinus rhythm before the stroke. The incidence of definite TEC after cardioversion was significantly lower in the anticoagulated patients (0.1% [3 of 2,298] vs 0.7% [38 of 5,362], p = 0.001).
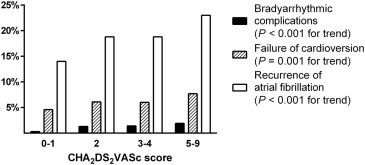
There was a significant increase in the incidence of definite TEC with higher CHA 2 DS 2 VASc scores in cardioversions performed without anticoagulation (p <0.001 for trend; Figure 1 ). In patients with a CHA 2 DS 2 VASc score of ≥2, the rate of definite TEC was significantly lower after cardioversion performed with anticoagulation (0.2% [3 of 1,708] vs 1.1% [28 of 2,590], p = 0.001), but the benefit of anticoagulation did not reach statistical significance in patients with a CHA2DS2VASc score of 0 to 1 (0.0% [0 of 590] vs 0.4% [10 of 2,772], p = 0.23). In non-anticoagulated patients with the first cardioversion during the study period, the C-statistics were 0.72 (95% confidence interval [CI] 0.61 to 0.83, p <0.001) for CHA 2 DS 2 VASc score and 0.66 (95% CI 0.55 to 0.78, p = 0.006) for CHADS 2 score in predicting definite TEC, and CHA 2 DS 2 VASc score was a better (p = 0.003) predictor of the risk of definite TEC than CHADS 2 score. Multivariable analysis showed that age (per year) (odds ratio [OR] 1.05; 95% CI 1.02 to 1.09, p <0.001), duration of AF episode >12 hours (OR 3.89; 95% CI 1.76 to 8.60, p = 0.001), heart failure (OR 3.37; 95% CI 1.39 to 8.19, p = 0.007), diabetes mellitus (OR 2.66; 95% CI 1.25 to 5.69, p = 0.012), and female gender (OR 2.11; 95% CI 1.04 to 4.28, p = 0.038) were independent predictors of definite TEC in cardioversions performed without anticoagulation.
In addition to definite TEC, 6 TIA episodes (0.1%) occurred within 30 days after cardioversion, 5 after successful cardioversion and 4 in patients without anticoagulation. The median CHA 2 DS 2 VASc score was 2.5 in patients without anticoagulation. Two patients with anticoagulation had CHA 2 DS 2 VASc scores of 4 and 5.
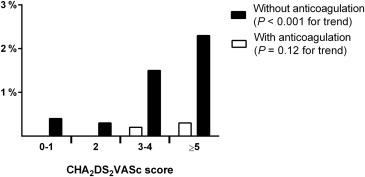
The failure rate of cardioversion, the rate of early recurrence of AF after successful cardioversion, and incidence of bradyarrhythmic complications increased with higher CHA 2 DS 2 VASc scores ( Figure 2 ). The CHA 2 DS 2 VASc score was an independent predictor of unsuccessful cardioversion (OR 1.09; 95% CI 1.03 to 1.16, p = 0.006), recurrence of AF after successful cardioversion (OR 1.17; 95% CI 1.12 to 1.22, p <0.001), and bradyarrhythmic complications (OR 1.44; 95% CI 1.27 to 1.62, p <0.001).