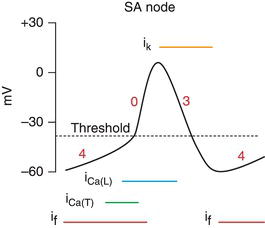
Figure 21.1 Pacemaker current and ion traffic. (See Color plate 21.1). (Source: http://www.cvphysiology.com/Arrhythmias/SAN%20action%20potl.gif, with permission from Dr Richard Klabunde).
This conduction process follows five phases of depolarization and repolarization (Figure 21.2). The resting membrane potential is set by phase 4. When the action potential reaches the cell, it raises the resting membrane potential until it reaches a threshold potential that opens voltage gated sodium (Na+) channels. The rapid influx of sodium ions causes a rapid depolarization that characterizes phase 0. This is immediately followed by phase 1 that is governed by potassium efflux. This is subsequently followed by phase 2, which consists of a balance between calcium ion (Ca2+) influx and potassium ion (K+) efflux. Therefore, phase 2 creates a plateau phase that effectively prolongs the action potential. In the myocardium, this is important as it allows sufficient time for calcium influx to bind to the contractile elements and initiate myocardial contraction. Finally, phase 3 of the action potential is caused by potassium ion (K+) efflux, which returns the membrane potential back to its resting state.
Figure 21.2 The cardiac action potential. (See Color plate 21.2). (Source: Richard N. Fogoros. Electrophysiologic Testing 5th edition, 2012. Reproduced with permission of John Wiley & Sons Ltd.).
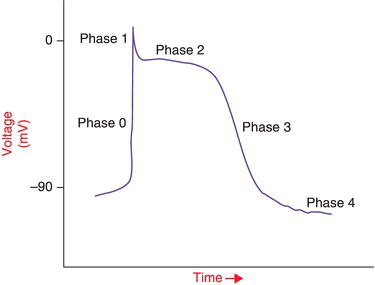
Figure 21.3 The effect of antiarrhythmic drugs on the cardiac action potential. The solid lines represent the baseline action potential and the dotted lines represent the changes that result in the action potential when various classes of antiarrhythmic drug are given. (See Color plate 21.3). (Source: Richard N. Fogoros. Electrophysiologic Testing 5th edition, 2012. Reproduced with permission of John Wiley & Sons Ltd.).
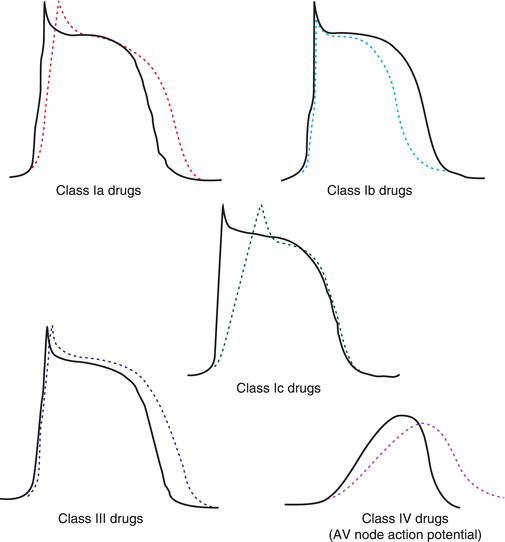
The Vaughan-Williams classification system groups antiarrhythmic drugs into four classes based upon which phase of the action potential is altered (Table 21.1). Class I agents mostly influence sodium channels. This class is further subdivided into three subclasses based upon the degree of sodium channel blockade that these agents produce (Figure 21.3). Class IA agents produce moderate sodium channel blockade, which causes slow phase 0 conduction and prolongs repolarization. Examples of agents in this class are quinidine, disopyramide and procainamide. Class IB agents produce mild sodium channel blockade, which shortens repolarization and has little effect on phase 0 depolarization in normal tissues. However, in abnormal tissue, this causes depressed phase 0 conduction. Examples of agents in this class are lidocaine and mexiletine. The IC agents produce marked sodium channel blockade, which causes a significant depression of phase 0 conduction but only a slight effect upon repolarization. Examples of agents in this class are flecainide and propafenone.
Class II agents produce sympatholytic, anti-ischemic, and anti-fibrillatory effects. Beta-blockers, such as propranolol and metoprolol, are the prototypical agents for this class.
Class III agents produce prolonged repolarization via potassium channel blockade. The typical agents for this class are sotalol and amiodarone. Both of these agents also have actions in other classes – sotalol is also a beta-blocker and amiodarone has properties of each of the four classes of antiarrhythmics. Dofetilide is an antiarrhythmic with pure class III properties.
Finally, the Class IV agents are calcium channel blockers, such as verapamil and diltiazem.
21.3 DISEASE-SPECIFIC THERAPY
21.3.1 Ventricular Tachycardia
Many studies have examined the efficacy of antiarrhythmic medications on ventricular tachycardia and sudden cardiac death. Large randomized controlled clinical trials have shown limited efficacy of antiarrhythmic therapy utilizing the endpoint of sudden cardiac death. Beta-blockers are a notable exception, in which case multiple trials in patients with a spectrum of cardiovascular conditions, including ventricular tachycardia, showed improved survival. Beta blockade is effective in preventing sudden cardiac death (SCD) and ventricular fibrillation (VF), but less so in suppressing spontaneous ectopy or monomorphic ventricular tachycardia (VT). Consequently, antiarrhythmic medication is used as adjunctive therapy to implantable cardioverter defibrillator (ICD) and/or catheter-based ablation procedures in most patients with structural heart disease.
Table 21.2 Major Side Effects and Recommended Monitoring for Patients on Amiodarone.
| Side effect | Monitoring/precautions |
| Hyperthyroidism/hypothyroidism | Thyroid functions tests at baseline and every 6 months |
| Abnormal liver enzymes1 | Liver function tests at baseline and every 6 months |
| Pulmonary toxicity symptoms including cough, fever, dyspnea | Pulmonary function tests with the diffusing capacity at baseline with yearly chest X-ray |
| Corneal deposits/optic neuropathy | Eye examination at baseline with repeat examinations as needed |
| Conduction abnormalities including prolonged QT | ECG at baseline and yearly |
| Photosensitivity to UV light | Avoid sunlight and use sunscreen |
| Blue-gray skin discoloration | Reduce dose or discontinue medication |
1Defined as AST or ALT elevation ≥2x upper limit of reference range.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


