Fig. 3.1
Patient positioned for robotic-assisted cardiac surgery
Venous and Arterial Cannulation
As for standard cardiac surgery patients, a central venous line is placed for fluid and medication administration and to enable Swan-Ganz catheter placement. However, for robotic cardiac surgery central venous cannulation may involve placement of several additional catheters. For example, a coronary sinus catheter, a superior vena caval (SVC) cannula, and a pulmonary artery drain all may need to be placed in the right internal jugular (IJ) vein (See Chap. 5). Thus, it is useful to place the standard central line in an alternate site, such as the left IJ or a subclavian vein.
Venous Cannulation
A 15–17 Fr Biomedicus® (Medtronic Corp, Minneapolis, MN) catheter is placed in the right IJ vein for superior vena caval drainage (SVC) (Fig. 3.2). The SVC cannula requires direct-line insertion into the right IJ for proper drainage passage into the right atrium. The SVC drainage cannula is placed using the standard Seldinger guide-wire technique. To verify guide-wire placement within the right IJ vein, surface ultrasound imaging is helpful. TEE is used to confirm passage of the wire into the right atrium. To avoid IJ vein perforation during cannula insertion, which can occur at the subclavian IJ vein junction, the SVC cannula should meet little resistance and never be forced. This cannula tip has a slight step-up ledge as it passes over the coaxial dilator, and this may cause resistance as it enters the skin and platysma muscle. A generous skin incision with traction can help overcome this resistance. Once placed over the dilator, the cannula should be positioned in the right atrium under TEE guidance (Fig. 3.3). Once seen in the right atrium, the cannula can be withdrawn into the SVC and positioned just above the right atrial junction. This position is often out of TEE view in the mid-esophageal bi-caval window. If this cannula is not positioned correctly, the left robotic arm can injure either the superior cava or right atrium. Generally, this results from the left instrument arm rubbing tissue that is stretched across the hard cannula tip. Because of a tapered neck, the SVC cannula can become dislodged easily if not secured tightly. Therefore, the cannula must be sutured or taped securely to the neck after positioning. To avoid thrombus formation after SVC cannulation (patient not heparinized fully), a dilute heparin solution (1,000 units in 500 mL) is infused through a micro-dripper.
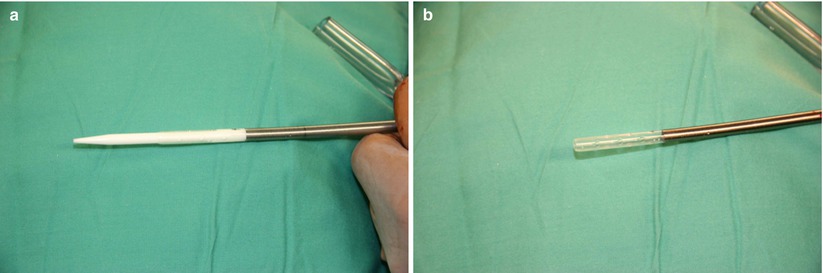
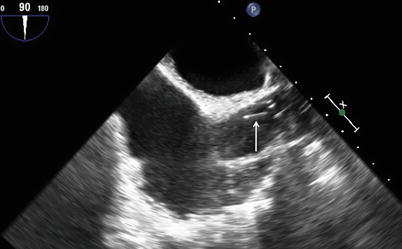
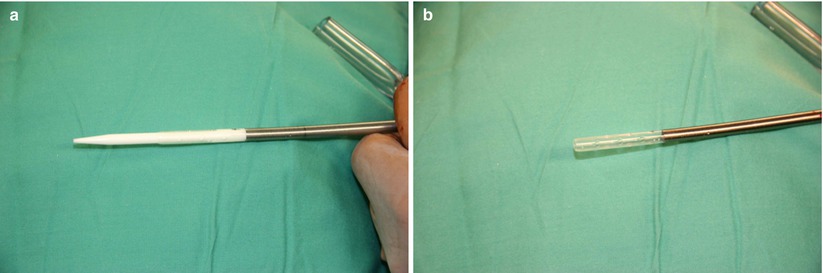
Fig. 3.2
A superior vena cava 17 Fr drainage cannula with the introducer in place (a) and with the introducer removed (b)
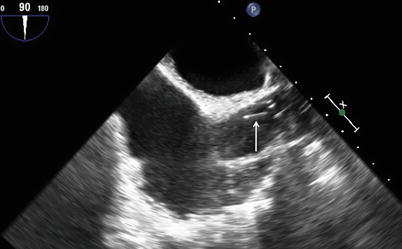
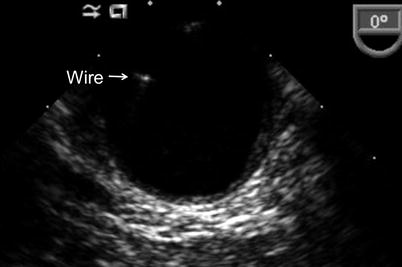
Fig. 3.3
Mid-esophageal bi-caval TEE view showing the superior vena cava drainage cannula (arrow) in the right atrium
Routinely, we place a single-stage inferior vena cava (IVC) drainage cannula, which is passed over a guide-wire into the right atrium into the right femoral vein either percutaneously or through a small incision. During IVC cannula placement, the guide-wire and drainage cannula are directed by selecting the bi-caval TEE mid-esophageal view. By guiding lower venous cannulation using real-time TEE, IVC cannula passage, either through a patent foramen ovale or into the SVC, can be avoided. The ideal position for the best cardiac drainage is just below the IVC-right atrial junction. Two-stage cannulas must be passed into the SVC for maximal drainage (Fig. 3.4).
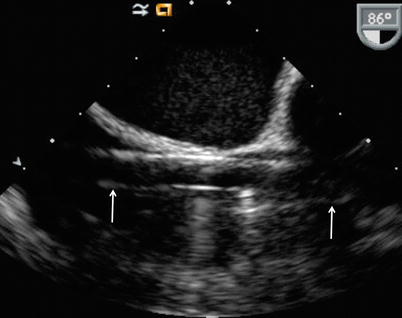
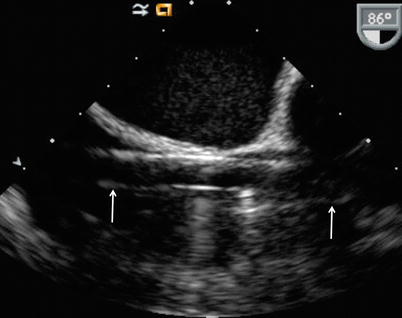
Fig. 3.4
Mid-esophageal bi-caval TEE view showing a two-stage drainage cannula (arrows) traversing the inferior vena cava, right atrium, and superior vena cava
Arterial Cannulation and Endoballoon Placement
Prior to femoral arterial cannulation, it is important to view the guide-wire in the aortic lumen with TEE (Fig. 3.5). Guide-wire verification decreases the risk of a retrograde aortic dissection with the initiation of cardiopulmonary bypass. The TEE is also useful for Endoballoon (Edwards Lifesciences, Irvine, Calif) placement, when it is used to clamp the aorta instead of an external direct clamp. The proper Endoballoon resting position should be just above the aortic sino-tubular junction, and well below the origins of the innominate artery and cerebral vessels (Fig. 3.6). Stability of the endoballoon position in the ascending aorta should be monitored with TEE throughout the operation. During antegrade cardioplegia administration and with varying systemic pressures, these balloons can migrate and cause complications. However, tracheal air echo artifacts can obscure the exact Endoballoon ascending aortic position. Therefore, when using the Endoballoon aortic occlusion, it is safest to place bi-lateral arterial pressure catheters and cerebral oximetry patches to alert anesthesiologists and surgeons for possible migration to cover the innominate artery origin (i.e. right carotid artery).