Most common agents for occupational asthma
Workers at risk of exposure
Isocyanates
Rigid or flexible polyurethane foam makers, polyurethane foam insulation installers, urethane spray painters, users of adhesives
Flour
Bakers, bakery workers
Cleaning products
Health-care workers, cleaners
Wood dusts
Carpenters, sawmill workers, forestry workers
Enzymes, amylase
Laboratory workers, pharmaceutical workers, food industry workers, detergent workers
Animal antigens, mites
Farmers, veterinarians, cleaners
Solder/colophony
Welders, electronics workers
Glues and adhesives
Multiple, autobody workers
Chlorine
Chemical plant workers, cleaners, pool attendants
Irritant-induced occupational asthma
Definite (reactive airways dysfunction) | Probable/possiblea |
|---|---|
New asthma onset with no previous lung disease | History of childhood asthma that resolved and asthma recurred with exposure, History of smoking with no previous documented pulmonary function measures. |
Symptoms begin within 24 hours after a single presumed high-level irritant exposure | Symptoms begin after 24 hours but within days following a presumed high-level irritant exposure, or more than one exposure |
Symptoms severe enough to lead to an unscheduled medical visit or emergency visit | No acute visit for symptoms |
Objective evidence of asthma from a bronchodilator response or test of airway hyperresponsiveness | Objective evidence of asthma from a bronchodilator response or test of airway hyperresponsiveness |
Asthma persists at least 3 months | Symptoms clear within 3 months |
No other explanation for findings | Other explanations possible but cannot be proven |
In contrast to occupational asthma, work-exacerbated asthma usually occurs in patients with a pre-existing history of asthma prior to entering the workplace in question. While this may seem to be fairly clear in principle, in practice the under-diagnosis and over-diagnosis of asthma are common [14]. This may further complicate matters when patients apply for workers’ compensation as it may be difficult to distinguish with certainty between de novo occupational asthma, undiagnosed pre-existing asthma, or a coincidental onset of asthma with work-exacerbation. Furthermore, patients with pre-existing asthma can become sensitized to occupational asthmagens and then have worsening asthma in the workplace that clinically would be managed in the same way as sensitizer-induced occupational asthma. The workers’ compensation board classification of these cases (as occupational asthma or work-exacerbated asthma) may vary in different jurisdictions. Conditions in the workplace that can lead to work-exacerbation of asthma are common and may be present in a wide variety of occupations. In one study in the United States from 1993 to 1995 [15], workers with work-exacerbated asthma were most likely to be employed in the service industry (40%), manufacturing (22%) and public administration (16%). In the same study, the most common reported responsible agents were in descending order, mineral and inorganic dusts, indoor air pollutants, chemicals, cleaning agents, paint and cigarette smoke. A Canadian study of work-exacerbated asthma claims in a workers’ compensation population identified production workers, government office workers, health-care workers, teachers and other indoor workers as the most common occupations [4]. What is important to note in both these studies is the high frequency of office and non-industrial indoor work occupations – work environments that might not initially be suspected as high risk for work-related asthma.
5.2 Diagnosis
Despite the importance of early intervention in work-related asthma, the diagnosis is often delayed. In a Canadian study of work-related asthma , the median time to suspicion by the physician of work-relatedness was 2 years, with a definite diagnosis of asthma 4 years after onset of symptoms [16]. Possible reasons for delay in diagnosis include workers’ fear of job loss and reduction in income, lack of recognition by workers that work exposures can cause asthma and failure of health-care providers to consider work-relatedness [17–19]. Work-related asthma must therefore be considered by the health-care provider in all patients with new adult onset asthma and in all workers with pre-existing asthma.
Is there a difference in asthma symptoms when away from work? On weekends or holidays?
Were there any changes in the workplace processes that preceded the onset of symptoms?
Was there an unusual work exposure within 24 hours of the onset of initial symptoms?
Reported improvement in asthma symptoms when away from work on weekends or holidays has been found to have high sensitivity (approximately 88%) for occupational asthma from a sensitizer [20] but has low specificity as it can also occur with work-exacerbated asthma. Typical patterns of work-related symptoms mirror the patterns in serial peak flow monitoring (see below under investigations). Workers typically describe a steady progression of symptoms over a work week with improvement on weekends or holidays. This history may be more difficult to elicit in the case of shift work or rotating schedules. Some patients may describe worsening within minutes of exposure to a workplace asthmagen with improvement rapidly after finishing a work shift, and some may describe symptoms only when doing specific work processes that may not be daily or regularly part of their work routine. A history of acute onset symptoms after an unusual work exposure to a likely respiratory irritant would raise suspicion for acute irritant-induced asthma. Workers who have been exposed for a prolonged period of time may no longer experience improvement in symptoms on the weekends off work, or after short durations of removal from the workplace. Workers may also not appreciate a work-related pattern of symptoms when the worsening of symptoms occurs several hours after the work exposure, which may be seen in isolated late asthmatic responses, particularly with low molecular weight sensitizers. Eliciting a history of symptoms of rhinoconjunctivitis in the workplace suggests sensitization to a workplace antigen and may precede the development of respiratory symptoms of occupational asthma by months to years [21].
When exploring the exposure history, it is best to ask the worker to describe their work process rather than rely on job titles alone. For example, a job description of “machinist” may comprise a wide spectrum of tasks with different exposures depending on the type of machinery, materials and tools used. Additionally, workers are rarely isolated in the workplace and exposures may come from work processes performed by nearby co-workers. Processes that may be expected to produce airborne agents such as welding and spray painting are particularly suspect. The use of respiratory protection in the workplace can provide another clue to the possibility of exposure to harmful airborne substances. Additionally, even strict compliance with use of advised respiratory protective devices in the workplace does not completely remove exposure and does not eliminate the potential for sensitization to an asthmagen.
In many instances, workers may not be aware of the exact agents they are exposed to – often describing substances they work with only by their physical description, odor or trademark name. Material Safety Data Sheets (MSDSs) / Safety Data Sheets (SDSs) obtained from the workplace can be helpful in identifying exposures, though their reliability in identifying safety and toxicity information can be incomplete [22]. The single question “Does/did this job expose you to vapors, gas, dust or fumes (VGDF)” is a useful screening question that identifies workers at risk for airway irritation (and occupational chronic obstructive airways disease) [23]. A history of high intensity exposure is associated with a higher risk of developing occupational asthma , with episodes of very high concentration exposures more associated with acute onset irritant-induced asthma. However, sensitization can occur even with allowable exposure levels at work, and once an individual has been sensitized to an occupational asthmagen, even low levels of exposure can cause exacerbations of asthma symptoms.
Atopy and prior allergic disease may suggest the possibility of pre-existing asthma and subsequent work-exacerbated asthma. However, patients with atopy (as well as a history of cigarette smoking [24]) are at an increased risk for the development of occupational asthma from some high-molecular weight sensitizers, and an atopic background should not be used to exclude the diagnosis. The differentiation of occupational asthma as opposed to undiagnosed pre-existing asthma with work-exacerbation can be challenging in this situation. Review of previous medical records to exclude prior lung disease is helpful but may not always be possible. However, the distinction may be important in cases of worker’s compensation claims, especially for the diagnosis of work-related irritant-induced asthma and in attempting to distinguish new-onset asthma due to an occupational sensitizer from pre-existing asthma with additional sensitization at work. However, for those with work-sensitization contributing to asthma, even if there was pre-existing asthma, removal from further exposure to the workplace sensitizer is essential.
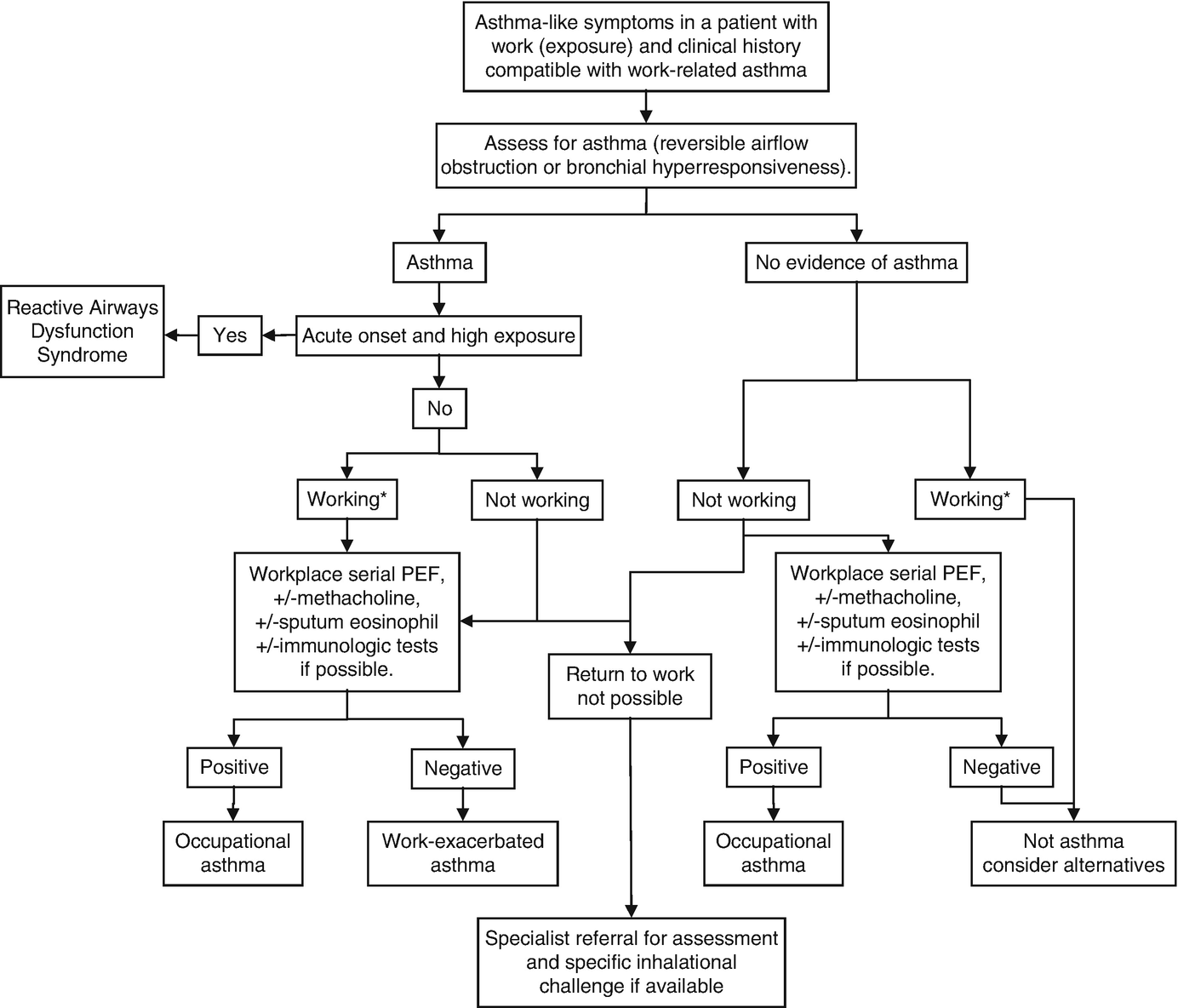
Diagnostic algorithm for work-related asthma. ∗“working” implies the same work conditions as suspected to cause work-related symptoms
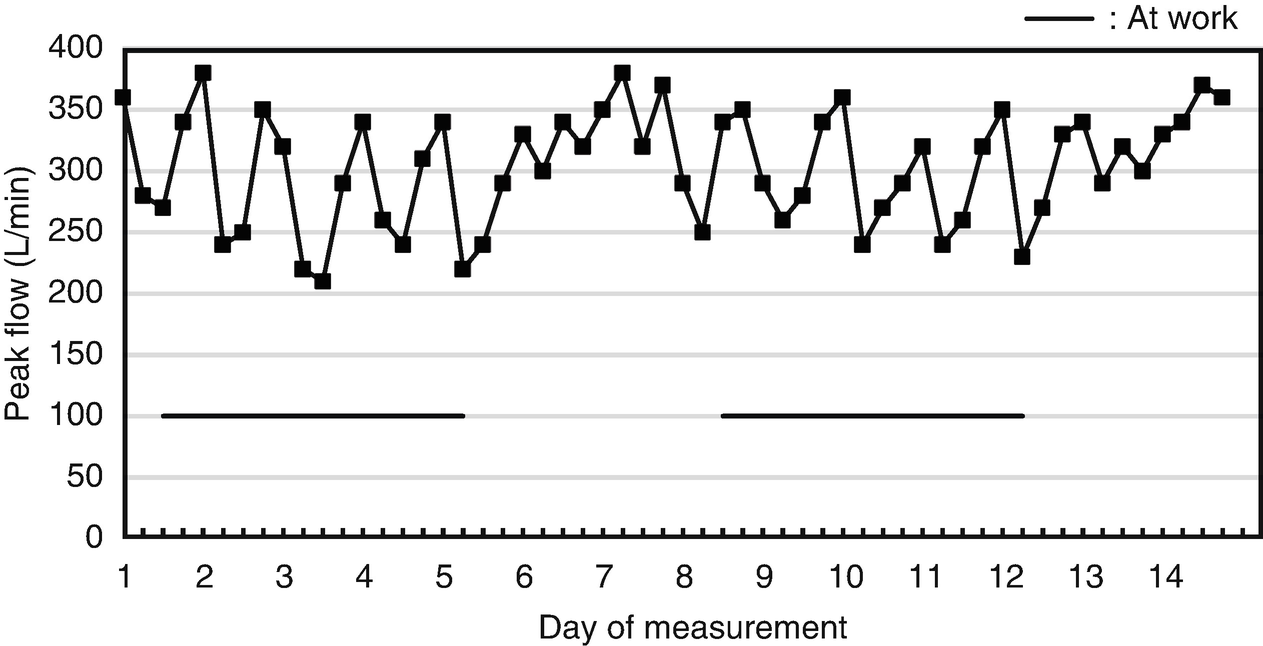
Spirometry can be used to measure serial changes in airflow limitation during periods of work and away from the workplace and is often the first test used by the clinician to diagnose asthma. However, frequent (daily) measurements of FEV1 with in-office spirometry is not practical, while a single pair of measurements on and off-work is not sensitive for the diagnosis of occupational asthma . Portable spirometry recordings, or more commonly serial peak expiratory flow measurements, are frequently used to investigate occupational asthma. The current cost of portable spirometers limits their usage. Peak flow metres are relatively inexpensive, require minimal training due to ease of use and can allow for frequent measurement of airflow obstruction. The ability to test while in the workplace is one of the most important strengths of peak expiratory flow monitoring, providing a realistic exposure challenge that may be difficult or impossible to reproduce in a laboratory inhalational challenge. In complex work environments where the exact asthmagen cannot be identified, at-work and off-work serial peak flow monitoring provides useful information on the work-relatedness of symptoms.
Measurements are ideally made in triplicate, a minimum of four times per day for at least 2 weeks at work and a similar period away from work. Symptom scores and as-needed short-acting bronchodilator use should also be recorded while other asthma medications are kept stable. Increased frequency of measurements may improve accuracy of data but must be balanced with increased patient burden, lower compliance and likelihood of less reliable data.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


