Fig. 1.1
Human heart with pericardium splayed (black arrows) revealing epicardial fat (asterisk)
The normal pericardial thickness is less than 2 mm as seen on imaging studies and less than 1 mm on anatomical studies [2]. The pericardial space between the visceral and parietal layers normally contains less than 50 ml of serous fluid which in normal hearts is contained in the pericardial recesses and sinuses mostly over the atrial-ventricular and inter-ventricular grooves [3] (Fig. 1.1).
Serosal Pericardium
The serosal layer is composed of a surface layer of flattened mesothelial cells whose luminal surface is completely lined with surface microvilli and few cilia which are thought to serve as both specialized friction-bearing surfaces as well as to increase the cell surface area available for fluid transport [4]. Histologic examination of the serosal pericardium suggests the capability of the luminal surface to modify its configuration as well as the ability to permit both transport through intercellular spaces and across the cytoplasm by vesicular transport [4].
Fibrous and Parietal Pericardium
The parietal pericardium is composed of the serosal and fibrosal layers as well as an outer layer of epipericardial tissue. The fibrous pericardium is composed of connective tissue cells, microvasculature, lymphatics, collagen fibers, and small elastic fibers. The epipericardial layer is composed of connective tissue as well as neural elements and blood vessels [4]. Coarse collagenous bundles in the epipericardial layer form the sternopericardial ligaments. Mast cells, lymphocytes, and histiocytes can be found in both the fibrosal and epipericardial layers [4]. The varied orientation and the wavy arrangement of the collagen fibers in the fibrous layer are such that they allow for some degree of multidirectional stretch to occur. However, given the inextensible nature of collagen fibrils, once the collagen fibrils are straightened out, further stretching of the fibrous layer is limited [4]. It has also been shown that the waviness of the pericardial collagen is maximal in young adulthood and decreases thereafter with age [4] (Fig. 1.2).
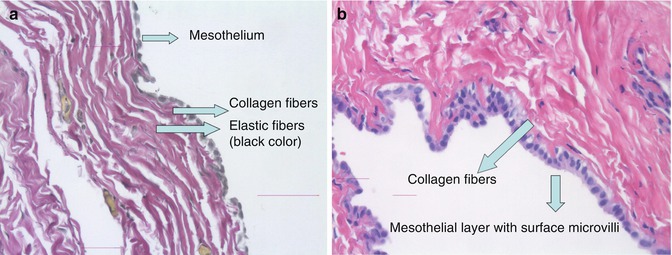
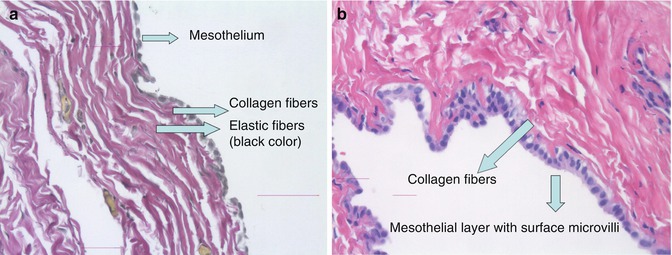
Fig. 1.2
Parietal pericardium. (a) EVG stain of parietal pericardium displaying the serosal (mesothelial) layer and fibrous layers composed of collagen and elastic fibers. (b) H&E stain of parietal pericardium displaying serosal (mesothelial) layer and collagen fibers (Courtesy of Dr. Shweta Gera and Dr. Pushpa Kancherla, Mt. Sinai St. Luke’s Pathology Department, New York, NY)
Pericardial Sinuses and Recesses
The visceral pericardium envelopes the heart and its attached vessels and is reflected into the parietal pericardium forming a sac around the heart. This reflection creates two invaginations one enclosing the aorta and pulmonary trunk and the other enclosing the venae cavae and pulmonary veins. At these reflections about the vessels the pericardial cavity forms the pericardial sinuses and recesses which are continuous with the pericardial cavity. Normally, much of the pericardial fluid is contained within these sinuses and recesses. Familiarity with the anatomy of the sinuses and recesses may prove helpful in diagnostic and therapeutic procedures. For example, for patients requiring physiologic (atrial-ventricular) pacing who have limited venous access, placement of epicardial pacemaker leads through the pericardial reflections has been shown to be effective [5].
The transverse sinus is a passage between these two invaginations with the aorta and pulmonary trunk anteriorly and the atria and veins posteriorly. Bachmann’s bundle, a source of certain atrial arrhythmias, lines the floor of the transverse sinus (roof of the left atrium) and can be a target for radiofrequency ablation (RFA) [6]. The oblique sinus is a cul-de-sac like space that lies behind the left atrium and formed about the pulmonary veins and the inferior vena cava. The oblique vein of Marshall, also a potential source of arrhythmia, lies within the oblique sinus and is amenable to RFA via an epicardial approach [6].
Smaller spaces formed by reflections of pericardium between adjacent structures are called pericardial recesses. These recesses are named according to the structures that delineate them. The superior (aortic) pericardial recess is an extension of the transverse sinus that lies anteriorly, posteriorly and to the right of the ascending aorta and is bordered posteriorly by the superior vena cava. The superior pericardial recess can be misinterpreted as an aortic dissection, lymphadenopathy, or a cystic mediastinal mass on computed tomography (CT) imaging [7]. The inferior aortic recess is an extension of the transverse sinus that lies between the lower part of the ascending aorta and the right atrium. The anterior left ventricular outflow tract (LVOT) and proximal aorta (and aortic valve cusps) can be accessed for RFA via the inferior aortic recess [6]. The post caval recess lies behind the superior vena cava and is separated from the transverse sinus above by the right pulmonary artery and below by the right upper pulmonary vein. The left and right pulmonic recesses are lateral extensions of the transverse sinus that lie inferior to the left and right pulmonary arteries respectively. The left and right pulmonary venous recesses lie behind the left atrium between the upper and lower pulmonary veins (Fig. 1.3).
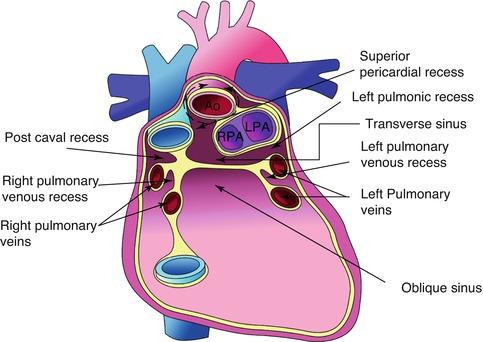
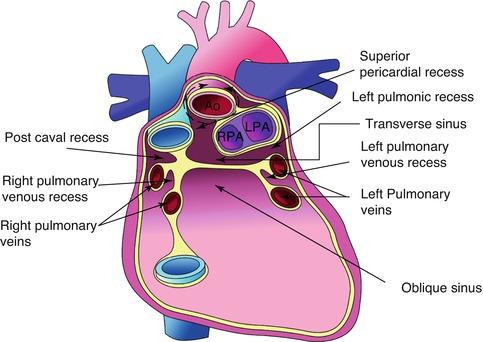
Fig. 1.3
Anatomic locations of the pericardial recesses and sinuses. Ao aorta, LPA, RPA left and right pulmonary arteries respectively, SVC, IVC superior and inferior venae cavae respectively (Courtesy of Adult Congenital Heart group, Boston Children’s Hospital and Brigham and Women’s Hospital, Harvard Medical School, Boston, MA)
Pericardial Fat
Fat deposits are found around the heart as epicardial fat (Fig. 1.1) covered by the visceral pericardial layer and as fat deposits on the outer surface of the fibrous pericardium. The epicardial fat predominantly overlies the atrioventricular and interventricular grooves and the right ventricle and contains the coronary arteries and veins, lymphatics, and nervous tissue. The epicardial fat serves as both a mechanical and immune barrier for the heart, a regulator of vascular flow by vasocrine mechanisms and as a local source of fatty acids during periods of high myocardial demand. Epicardial fat is associated with cardiovascular disease [8] which may be mediated by its paracrine effects, locally secreting cytokines which can accelerate the atherosclerotic process by means of endothelial dysfunction, smooth muscle proliferation, and oxidative stress [9].
Lymphatic Drainage
The pericardium has an extensive network of lymphatics providing active turnover of protein and various other substances from within the pericardial space. This turnover is mediated by lymphatics in both the epicardium and parietal pericardium. The lymphatic vessels of the anterior pericardium either travel upwards along the phrenic nerves terminating in the anterior right and left mediastinal nodes or travel downwards terminating at the diaphragm or prepericardial lymph nodes. The lymphatics of the lateral pericardium drain into the anterior mediastinal, tracheobronchial, lateropericardial, prepericardial and paraesophageal lymph nodes. The lymphatics of the posterior pericardium drain into the paraesophageal and tracheobronchial lymph nodes. Lymphatics of the inferior or diaphragmatic part of the pericardium drain into the right lateropericardial, right prepericardial, paraesophageal, and tracheobronchial lymph nodes [10] (Fig. 1.4).
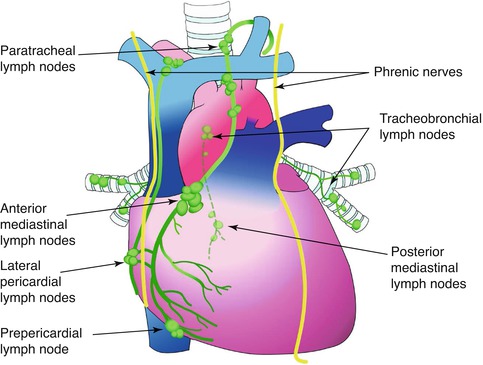
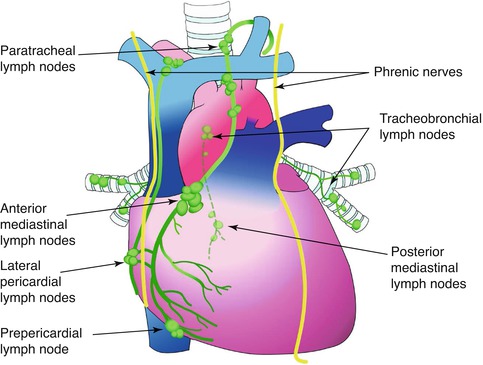
Fig. 1.4
Lymphatic drainage of the pericardium (Courtesy of Adult Congenital Heart group, Boston Children’s Hospital and Brigham and Women’s Hospital, Harvard Medical School, Boston, MA)
Vascular Supply
The pericardium receives its blood supply from branches of the internal thoracic (mammary) and musculophrenic arteries and the descending thoracic aorta [11]. The pericardial veins vary in number and drain into the left innominate, azygous, and internal thoracic veins. The lymphatic system is also thought to play an important role in venous drainage of the myocardium.
Innervation
Parasympathetic nerve fibers branching from the vagus, left recurrent laryngeal, and esophageal plexus innervate the pericardium. Sympathetic innervation is supplied from the first dorsal ganglion, stellate ganglion, and the aortic, cardiac, and diaphragmatic plexuses [11]. Additionally, the pericardium secretes prostaglandins with which increased levels have been shown to modulate sympathetic nerve effects and potentially suppress the development of arrhythmias in various situations [12].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


