Anatomy and Physiology of the Heart
Description and location of the heart
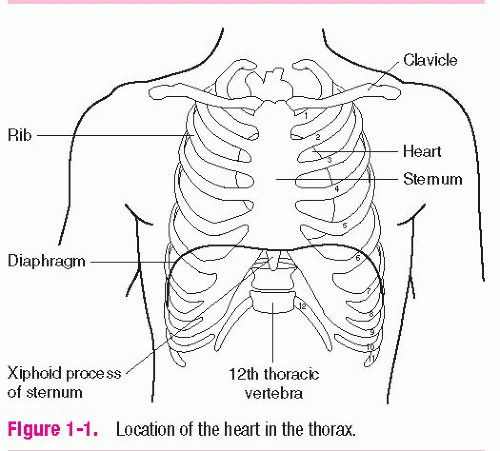
The heart is a hollow, four-chambered muscular organ that lies in the middle of the thoracic cavity between the lungs, behind the sternum, in front of the spinal column, and just above the diaphragm (Figure 1-1). The top of the heart (the base) is at approximately the level of the second intercostal space. The bottom of the heart (the apex) is formed by the tip of the left ventricle and is positioned just above the diaphragm to the left of the sternum at the fifth intercostal space, midclavicular line. There, the apex can be palpated during ventricular contraction. This physical examination landmark is referred to as the point of maximal impulse (PMI) and is an indicator of the heart’s position within the thorax.
The heart is tilted forward and to the left so that the right side of the heart lies toward the front. About two-thirds of the heart lies to the left of the body’s midline and one-third extends to the right. The average adult heart is approximately 5″ (12 cm) long, 3½″ (8 to 9 cm) wide, and 2½″ (6 cm thick) — a little larger than a normal-sized fist. The heart weighs between 7 and 15 oz (200 and 425 grams). Heart size and weight are influenced by age, weight, body build, frequency of exercise, and heart disease.
Function of the heart
The heart is the hardest working organ in the body. The heart functions primarily as a pump to circulate blood and supply the body with oxygen and nutrients. Each day the average heart beats over 100,000 times. During an average lifetime, the human heart will beat more than 3 billion times.
The heart is capable of adjusting its pump performance to meet the needs of the body. As needs increase, as with exercise, the heart responds by accelerating the heart rate to propel more blood to the body. As needs decrease, as with sleep, the heart responds by decreasing the heart rate, resulting in less blood flow to the body.
The heart consists of:
four chambers
two atria that receive incoming blood
two ventricles that pump blood out of the heart
four valves that control the flow of blood through the heart
an electrical conduction system that conducts electrical impulses to the heart, resulting in muscle contraction.
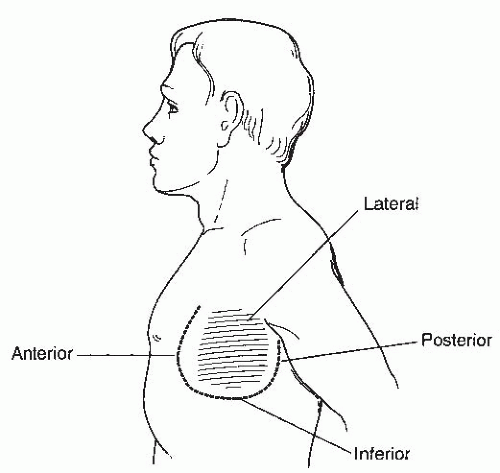
Heart surfaces
There are four main heart surfaces to consider when discussing the heart: anterior, posterior, inferior, and lateral (Figure 1-2). The heart surfaces are explained below:
anterior — the front
posterior — the back
inferior — the bottom
lateral — the side.
Structure of the heart wall
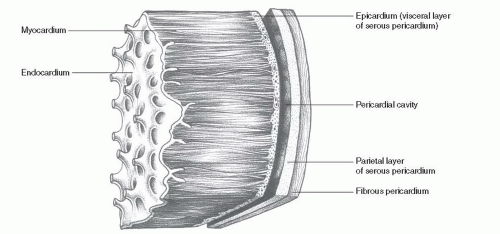
The heart wall is arranged in three layers (Figure 1-3):
the pericardium — the outermost layer
the myocardium — the middle muscular layer
the endocardium — the inner layer.
Enclosing and protecting the heart is the pericardium, which consists of an outer fibrous sac (the fibrous pericardium) and an inner two-layered, fluid-secreting membrane (the serous pericardium). The outer fibrous pericardium comes in direct contact with the covering of the lung (the pleura) and is attached to the center of the diaphragm inferiorly, to the sternum anteriorly, and to the esophagus, trachea, and main bronchi posteriorly. This position
anchors the heart to the chest and prevents it from shifting about in the thorax. The serous pericardium is a continuous membrane that forms two layers: the parietal layer lines the inner surface of the fibrous sac and the visceral layer (also called epicardium) lines the outer surface of the heart muscle. Between the two layers of the serous pericardium is the pericardial space, or cavity, which is usually filled with 10 to 30 mL of thin, clear fluid (the pericardial fluid) secreted by the serous layers. The primary function of the pericardial fluid is to provide lubrication, preventing friction as the heart beats. In certain conditions, large accumulations of fluid, blood, or exudates can enter the pericardial space and may interfere with ventricular filling and the heart’s ability to contract.
anchors the heart to the chest and prevents it from shifting about in the thorax. The serous pericardium is a continuous membrane that forms two layers: the parietal layer lines the inner surface of the fibrous sac and the visceral layer (also called epicardium) lines the outer surface of the heart muscle. Between the two layers of the serous pericardium is the pericardial space, or cavity, which is usually filled with 10 to 30 mL of thin, clear fluid (the pericardial fluid) secreted by the serous layers. The primary function of the pericardial fluid is to provide lubrication, preventing friction as the heart beats. In certain conditions, large accumulations of fluid, blood, or exudates can enter the pericardial space and may interfere with ventricular filling and the heart’s ability to contract.
The myocardium is the thick, middle, muscular layer that makes up the bulk of the heart wall. This layer is composed primarily of cardiac muscle cells and is responsible for the heart’s ability to contract. The thickness of the myocardium varies from one heart chamber to another. Chamber thickness is related to the amount of resistance the muscle must overcome to pump blood out of the chamber.
The endocardium is a thin layer of tissue that lines the inner surface of the heart muscle and the heart chambers. Extensions and folds of this tissue form the valves of the heart.
Circulatory system
The circulatory system is required to provide a continuous flow of blood to the body. The circulatory system is a closed system consisting of heart chambers and blood vessels.
The circulatory system consists of two separate circuits, the systemic circuit and the pulmonary circuit. The systemic circuit is a large circuit and includes the left side of the heart and blood vessels, which carry oxygenated blood to the body and deoxygenated blood back to the right heart. The pulmonary circuit is a small circuit and includes the right side of the heart and blood vessels, which carry deoxygenated blood to the lungs and oxygenated blood back to the left heart. The two circuits are designed so that blood flow is pumped from one circuit to the other.
Heart chambers
The interior of the heart consists of four hollow chambers (Figure 1-4). The two upper chambers, the right atrium and the left atrium, are divided by a wall called the interatrial septum. The two lower chambers, the right ventricle and the left ventricle, are divided by a thicker wall called the interventricular septum. The two septa divide the heart into two pumping systems — a right heart and a left heart.
The right heart pumps venous (deoxygenated) blood through the pulmonary arteries to the lungs (Figure 1-5). Oxygen and carbon dioxide exchange takes place in the alveoli and arterial (oxygenated) blood returns via the pulmonary veins to the left heart. The left heart then pumps arterial blood to the systemic circulation, where oxygen and carbon dioxide exchange takes place in the organs, tissues, and cells; then venous blood returns to the right heart. Blood flow within the body is designed so that arteries carry oxygen-rich blood away from the heart and veins carry oxygen-poor blood back to the heart. This role is reversed in pulmonary circulation: pulmonary arteries carry oxygen-poor blood into the lungs, and pulmonary veins bring oxygen-rich blood back to the left heart.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree