At a heart rate of 70 beats per minute, a human heart will contract approximately 100800 times a day, more than 36 million times a year and nearly 3 billion times during an 80-year lifespan.
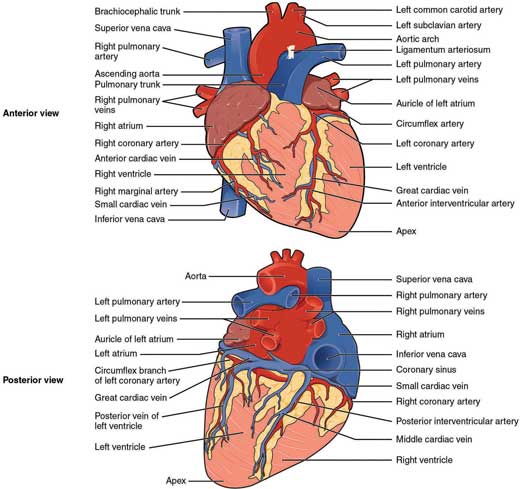
Figure 1.1 – The anatomy of the heart.
1.2 Chambers of the heart
Cardiac chambers In A Heartbeat
Right atrium |
|
Right ventricle |
|
Left atrium |
|
Left ventricle |
|
The heart has four chambers: two atria and two ventricles that function to return deoxygenated blood to the lungs and oxygenated blood to the rest of the circulation.

Figure 1.2 – The internal anatomy of the heart.
1.2.1 Right atrium
- Forms the entire right border
- Receives venous blood from the:
- superior vena cava superiorly, draining the azygos, subclavian and jugular veins
- inferior vena cava inferiorly, draining the lower body
- coronary sinus inferiorly, draining the heart
- anterior cardiac veins anteriorly, draining the anterior heart
- superior vena cava superiorly, draining the azygos, subclavian and jugular veins
- Anterior part of wall is smooth
- Posterior part of wall is rough with trabeculations known as musculi pectinati (pectinate muscles) derived from the true fetal atrium
- Crista terminalis is a muscular ridge that runs vertically downwards, separating the smooth and rough parts
- Right auricle/atrial appendage is a cone-shaped muscular pouch-like extension of the right atrium
- Fossa ovalis is a shallow oval depression in the interatrial septum
- an embryonic remnant of the fetal foramen ovale.
1.2.2 Right ventricle
- Forms most of the inferior border and anterior surface of the heart
- Connected to the right atrium by the tricuspid valve which has three cusps: anterior, posterior and septal
- Connected to the pulmonary trunk by the pulmonary valve comprising three semilunar cusps
- Each cusp is connected to its corresponding papillary muscle by chordae tendinae (heart strings)
- Trabeculae carneae are irregular ridges lining the wall
- Moderator band is a muscular bundle connecting the interventricular septum to the anterior wall
- conveys the right bundle branch to the ventricular muscle
- Infundibulum is the smooth-walled outflow tract directed upwards and right towards the pulmonary trunk.
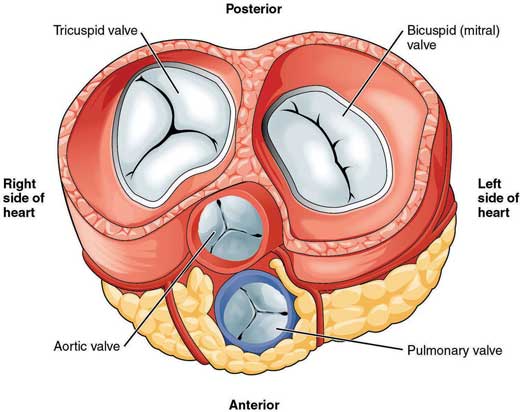
Figure 1.3 – Superior view of heart valves.
1.2.3 Left atrium
- Forms most of the base of the heart
- Smaller, but thicker walled than right atrium
- Receives oxygenated blood from the four pulmonary veins which open into the cavity on its posterior wall (two from each lung: superior and inferior)
- Left auricle/atrial appendage is an ear-shaped muscular pouch extending forwards and to the right
- this is a common site for thrombus formation
- Mainly smooth-walled except for ridges in the auricle due to underlying pectinate muscles.
1.2.4 Left ventricle
- Forms most of the left border and the apex of the heart
- Longer, more conical and thicker walled than the right atrium (three times thicker, between 6 and 10 mm in a normal heart)
- Wall is lined by thick trabeculae carneae
- Joined to left atrium by mitral valve
- Mitral valve has two cusps: anterior and posterior
- Chordae tendinae connects each cusp to its corresponding papillary muscle
- Communicates with aorta via the aortic valve:
- 3 semilunar cusps: anterior, right and left posterior
- anterior and left posterior aortic sinuses above the valve give rise to the right and left coronary arteries respectively.
- 3 semilunar cusps: anterior, right and left posterior
// PRO-TIP //
- ‘Pectinate’ means ‘like a comb’ in Latin
- The mitral valve gains its name from its resemblance to a bishop’s mitre
- A patent foramen ovale is found in 20% of adults and is usually asymptomatic
- Rupture of any papillary muscle, such as following a myocardial infarction, will cause the valve cusp to prolapse, resulting in severe regurgitation.
1.3 Coronary circulation
Coronary circulation In A Heartbeat
Right coronary artery |
|
Left coronary artery |
|
Coronary veins |
|
1.3.1 Coronary arteries
The heart has a high oxygen demand from continuous pumping of blood. This demand is met by the left and right coronary arteries.
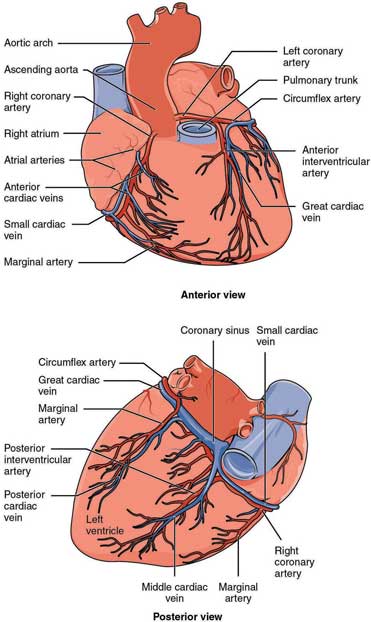
Figure 1.4 – The coronary vessels.
Right coronary artery
- Originates from the anterior aortic sinus
- Passes forwards between pulmonary trunk and right auricle
- Runs along the atrioventricular (AV) groove
- Continues to the inferior border of heart to anastamose with the circumflex branch of the left coronary artery
- Major branches:
- sinoatrial (SA) nodal artery runs posteriorly between the right auricle and aorta, supplying the SA node
- marginal artery along the inferior border of the heart
- posterior descending/posterior interventricular artery descends in the posterior interventricular groove to anastamose with the left anterior descending artery at the apex
- AV nodal artery arises from the characteristic loop where the posterior descending artery originates to supply the AV node.
- sinoatrial (SA) nodal artery runs posteriorly between the right auricle and aorta, supplying the SA node
Left coronary artery
- Originates from the left posterior aortic sinus
- Larger than the right coronary artery
- Left main stem varies in length (4–20 mm)
- known as the ‘widowmaker’ as occlusion leads to rapid death
- Initially passes behind then to the left of the pulmonary trunk
- Reaches the left part of the AV groove
- Runs laterally around the left border as the left circumflex artery to reach the posterior interventricular groove
- Major branches:
- left anterior descending (LAD)/anterior interventricular:
– descends in the anterior interventricular groove to anastamose with the posterior descending artery at the apex
- left circumflex (LCX):
– continues round the left side of the heart in the atrioventricular groove, giving off various ventricular and atrial branches
– anastamoses with the terminal branches of the right coronary artery.
- left anterior descending (LAD)/anterior interventricular:
// PRO-TIP //
Knowledge of the major and minor branches of the coronary arteries is essential for coronary angiogram interpretation. Figure 1.5 is a schematic of the arteries as visualised in a typical coronary angiogram.
RCA = right coronary | LAD = left anterior descending | |
RDP = posterior descending | D1 = first diagonal branch of LAD | |
RPL = right posterolateral branch | M1 = first marginal branch of LCX | |
LCX = left circumflex | MO1 = first marginal obtuse branch of LCX |
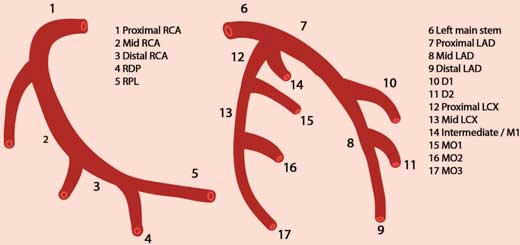
Figure 1.5 – Schematic of coronary arteries as visualised in a typical angiogram.
Anatomical variations
- 90% of the population are ‘right dominant’ – where the posterior descending/posterior interventricular artery branches from the right coronary artery. In the ‘left dominant’ 10%, the left coronary and circumflex arteries may be larger and branch off the posterior descending artery before anastomosing with an unusually smaller right coronary artery.
- The SA node is supplied by the right coronary in 60% and the left circumflex artery in nearly 40% of the population. Dual supply is present in 3%.
- The AV node is supplied by the right coronary artery in 90% of the population, with the remaining 10% by the left circumflex.
// PRO-TIP //
- The coronary arteries originate from the aortic sinuses – small openings superior to the cusps of the aortic valve. This makes coronary arteries the first branches of the aorta
- Coronary blood flow is about 250 ml/min at rest (5% of cardiac output) and rises to 1 L/min during exercise
- During systole (contraction), the aortic valves open and blood is ejected into the aorta. When the aortic valves close during diastole (when the heart is at rest), blood in the aorta flows into the aortic sinuses then into the coronary arteries to supply the heart
- Coronary flow takes place mainly during diastole. It is reduced during systole when the intramyocardial arteries are compressed by the contracting muscle
- Therefore, diastolic perfusion time is important for the coronary circulation. This is shortened by a rapid heart rate which may result in inadequate perfusion.
1.3.2 Coronary veins
Most of the heart’s venous drainage is fulfilled by the tributaries of the coronary sinus.
The coronary sinus runs in the posterior atrioventricular groove. It opens into the right atrium just to the left of the opening of the inferior vena cava. Its orifice is guarded by the Thebesian valve. Its tributaries are:
- the great cardiac vein in the anterior interventricular groove
- the middle cardiac vein in the inferior interventricular groove
- the small cardiac vein that accompanies the marginal artery along the inferior border of the heart
- the oblique vein which descends obliquely on the posterior side of the left atrium.
The remaining venous drainage is fulfilled by:
- the anterior cardiac veins (3 or 4 of them) draining a large proportion of the anterior surface of the heart directly into the right atrium
- small veins (venae cordis minimae) within each chamber wall draining directly into their respective chambers.
1.4 Conducting system of the heart
Conducting system In A Heartbeat
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


