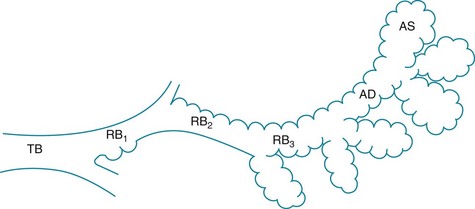
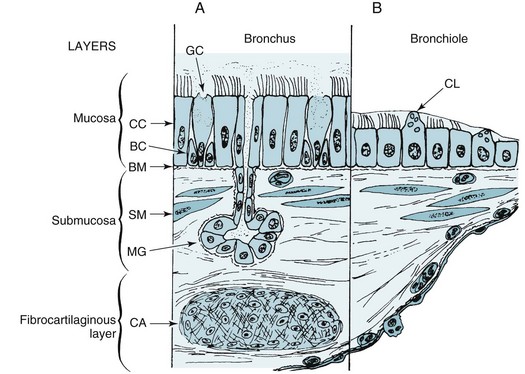
4 The trachea, bronchi, and bronchioles down to the level of the terminal bronchioles constitute the conducting airways. Their functions are to transport gas and protect the distal lung from inhaled contaminants. Beyond the terminal bronchioles are the respiratory bronchioles. They mark the beginning of the respiratory zone of the lung, where gas exchange takes place. Respiratory bronchioles are considered part of the gas-exchanging region of lung because alveoli are present along their walls. With successive generations of respiratory bronchioles, more alveoli appear along the walls up to the site of the alveolar ducts, which are entirely “alveolarized” (Fig. 4-1). The discussion in this chapter is limited to the conducting airways and those aspects of the more distal airways that affect air movement but not gas exchange. Alveolar structure is discussed further in Chapter 8. The airways are composed of several layers of tissue (Fig. 4-2). Adjacent to the airway lumen is the mucosa, beneath which is a basement membrane separating the epithelial cells of the mucosa from the submucosa. Within the submucosa are mucous glands (the contents of which are extruded through the mucosa), smooth muscle, and loose connective tissue with some nerves and lymphatic vessels. Surrounding the submucosa is a fibrocartilaginous layer that contains the cartilage rings that support several generations of airways. Finally, a layer of peribronchial tissue with fat, lymphatics, vessels, and nerves encircles the rest of the airway wall. Each of these layers is considered here, with a description of the component cells and the way the structure changes in the distal progression through the tracheobronchial tree. The surface layer (mucosa) consists predominantly of pseudostratified columnar epithelial cells. The mucosa appears to be several cells thick in the trachea and large bronchi, owing to the columnar shape and variable positions of the nuclei; however, each cell is resting on the basement membrane (see Fig. 4-2, A). The cilia that line the airway lumen are responsible for protecting the deeper airways by propelling tracheobronchial secretions (and inhaled particles) toward the pharynx. The cilia of airway epithelial cells have the characteristic ultrastructure seen in other ciliated cells: a central pair of microtubules and an outer ring of nine double microtubules (see Fig. 22-1). Small side arms called dynein arms, which contain the adenosine triphosphatase (ATPase) dynein, are found on the outer double microtubules. Proper configuration and function of dynein arms are necessary for normal ciliary functioning, and patients with cilia lacking the dynein side arms have impaired ciliary action and recurrent bronchopulmonary infections. The surface epithelium appears to have other important functions that may be altered in certain clinical conditions. By virtue of tight junctions between epithelial cells at the luminal surface, the epithelium prevents access of inhaled foreign material to deeper levels of the airway wall. Whether a disturbance in this barrier function is important in asthma—perhaps by allowing inhaled foreign material to penetrate the epithelial surface—is not known with certainty. Another important function involves active transport of ions, particularly chloride, to maintain a favorable ionic environment in the mucous layer lining the airway wall. In cystic fibrosis, an abnormality in chloride transport by surface epithelial cells plays a crucial role in the pathogenesis of the disease (see Chapter 7). The submucosal layer has two major components: bronchial mucous glands and bronchial smooth muscle. Mucus is a gel-like substance composed mostly of water (97%) and mucins. Other proteins including immunomodulators are also present, as well as electrolytes, lipids, and cellular debris. The mucous glands are located between bands of smooth muscle. The base of the glands is lined by mucous cells and serous cells and is connected to the airways by ducts lined by ciliated cells. The duct transports the secretions through the mucosa and discharges them into the airway lumen. As noted earlier, the primary mucin produced by mucous glands is MUC5B. In disease states such as chronic obstructive pulmonary disease and cystic fibrosis, where there is mucous gland hyperplasia, MUC5B becomes more prominent than MUC5AC in bronchial secretions. However, whether the functions of MUC5AC and MUC5B are different is not yet understood. Serous cells also line the mucous gland; these cells secrete proteoglycans and numerous antimicrobial substances involved in innate immunity (see Chapter 22). Airway smooth muscle is present from the trachea down to the level of the bronchioles and even the alveolar ducts. Disturbances in the quantity and function of the smooth muscle are important in disease, particularly in the case of bronchial asthma. We have thus far described the general structure of the airways, but structure varies considerably at different levels. Some of these differences are illustrated in Figure 4-2. In the progression distally through the tracheobronchial tree, the following changes are normally seen: 1. The epithelial layer of cells becomes progressively thinner until there is a single layer of cuboidal cells at the level of the terminal bronchioles. 2. Goblet cells decrease in number until they disappear about at the level of the terminal bronchiole. Domed-shaped Clara cells appear in the smaller airways, where they contribute to mucus production and other functions. 3. Mucous glands, which are present in the trachea and large bronchi, are most numerous in the medium-sized bronchi. They become progressively fewer in number more distally and are absent from the bronchioles.
Anatomic and Physiologic Aspects of Airways
Structure
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Anatomic and Physiologic Aspects of Airways