Alcohol and vagal activity may be important triggers for paroxysmal atrial fibrillation (PAF), but it remains unknown if these associations occur more often than would be expected by chance alone because of the lack of a comparator group in previous studies. We compared self-reported frequency of these triggers in patients with PAF to those with other supraventricular tachycardias (SVTs). Consecutive consenting patients presenting for electrophysiology procedures at a single university medical center underwent a structured interview regarding arrhythmia triggers. Two hundred twenty-three patients with a documented arrhythmia (133 with PAF and 90 with SVT) completed the survey. After multivariable adjustment, patients with PAF had a 4.42 greater odds (95% confidence interval [CI] 1.35 to 14.44) of reporting alcohol consumption (p = 0.014) and a 2.02 greater odds (95% CI 1.02 to 4.00) of reporting vagal activity (p = 0.044) as an arrhythmia trigger compared to patients with SVT. In patients with PAF, drinking primarily beer was associated with alcohol as a trigger (odds ratio [OR] 4.49, 95% CI 1.41 to 14.28, p = 0.011), whereas younger age (OR 0.68, 95% CI 0.49 to 0.95, p = 0.022) and a family history of AF (OR 5.73, 95% CI 1.21 to 27.23, p = 0.028) each were independently associated with having vagal activity provoke an episode. Patients with PAF and alcohol triggers were more likely to have vagal triggers (OR 10.32, 95% CI 1.05 to 101.42, p = 0.045). In conclusion, alcohol consumption and vagal activity elicit PAF significantly more often than SVT. Alcohol and vagal triggers often were found in the same patients with PAF, raising the possibility that alcohol may precipitate AF by vagal mechanisms.
Most studies describing the association between alcohol and atrial fibrillation (AF) have focused on alcohol as a risk factor for incident AF, with conflicting results. Less studied, but no less relevant, is the importance of alcohol as a trigger for AF in those who already have the disease. Although up to 34% of patients with paroxysmal AF (PAF) report that alcohol consumption precedes their episodes, all previous studies on this subject have been descriptive; a lack of a comparator group has precluded a quantitative study to determine if alcohol as a trigger for AF occurs more often than would be expected by chance alone. For example, because PAF may occur randomly and because alcohol intake is so common, it remains possible that alcohol appears to provoke AF episodes when in fact a causal association is not present. Similarly, activation of the parasympathetic nervous system has been implicated in the pathogenesis of PAF, but studies examining activities that increase vagal tone as triggers for AF in humans have been descriptive and not comparative. We sought to determine if alcohol consumption or vagal activation precipitated PAF episodes more often than would be expected by chance alone by comparing self-reported frequencies of these potential triggers in patients with paroxysmal supraventricular tachycardia (SVT) to those with PAF.
Methods
From September 2004 to March 2011, consecutive consenting patients presenting for procedures to the electrophysiology laboratory at the University of California, San Francisco were surveyed. We assigned a primary arrhythmia type to each subject based on documented arrhythmias from chart review, 12-lead electrocardiograms, and invasive electrophysiology procedures. We identified consenting patients with a primary diagnosis of PAF or SVT (n = 520). PAF was defined as ≥2 episodes of AF that terminated without intervention in <7 days. A primary diagnosis of SVT included the diagnoses atrioventricular nodal re-entrant tachycardia (AVNRT), atrioventricular re-entrant tachycardia (AVRT), atrial tachycardia (AT), and junctional tachycardia. We excluded patients with SVT and any history of AF or atrial flutter and patients with PAF and any current or previous SVT (remaining patients, n = 438). Analyses were limited to patients who completed survey questions regarding alcohol habits and other arrhythmia triggers (n = 223). “Lone AF” was defined as AF occurring in patients <60 years of age and without hypertension, diabetes, coronary artery disease, significant valve disease, or congestive heart failure. A family history of AF was defined as having any first- or second-degree relative with a diagnosis of AF determined by patient interview.
Patients were interviewed by research assistants using a structured questionnaire designed by the study authors. Surveyed areas were history of cardiovascular illness, detailed arrhythmia history, family history, and health-related behaviors. Patients reported alcohol consumption on a 6-point Likert scale ranging from “never” to “>2 drinks/day.” “Binge drinking” was defined as ever consuming >5 drinks in a 24-hour period. Type of alcoholic beverage consumed the most (wine, beer, or spirits) was ascertained. Patients reported whether their arrhythmia symptoms initiated or terminated with various activities or behaviors by answering on a 5-point Likert scale from “never” to “always” or “yes/no.” Vagal activation was considered a trigger if resting or eating provoked arrhythmia symptoms “often” or “always” or if symptoms terminated with exercise. Sympathetic activation was considered a trigger if patients answered yes to exertion, caffeine intake, or stress bringing about their symptoms.
Continuous variables are expressed as mean ± SD. Analyses were performed using Student’s t test or analysis of variance for continuous variables and chi-square test for categorical variables. Unadjusted and multivariable adjusted odds ratios (ORs) with 95% confidence intervals (CIs) were obtained using logistic regression for binary outcome variables. Ordered logistic regression was used to obtain ORs for frequency of alcohol as a trigger, which was grouped into 3 levels (never, rarely/sometimes, or often/always) to ensure that models satisfied the assumption of proportional odds. Missing data were excluded from regression analyses.
Covariates were included in multivariable models based on a priori beliefs regarding potential confounding (such as age, gender, and race) or if they were associated with the predictor and outcome with a p value <0.1. In all analyses related to alcohol consumption, multivariable models also included amount of alcohol consumed and the presence or absence of binge drinking. Data analysis was performed using STATA 12 (STATA Corp., College Station, Texas).
Results
Baseline characteristics are listed in Table 1 . In the SVT group, the primary diagnosis was AVNRT in 50 patients (56%), AVRT in 24 (27%), AVNRT and AVRT in 1 (1%), and AT in 14 (16%); 1 patient with SVT had no identifiable SVT mechanism after invasive electrophysiologic testing.
| Variable | PAF | SVT | p Value |
|---|---|---|---|
| (n = 133) | (n = 90) | ||
| Age (years) | 59 ± 12 | 47 ± 16 | <0.001 |
| Men | 94 (71%) | 32 (36%) | <0.001 |
| Race | 0.06 | ||
| White | 106 (80%) | 59 (66%) | |
| Black | 0 (0%) | 3 (3%) | |
| Asian | 15 (11%) | 14 (16%) | |
| Latino | 6 (5%) | 4 (4%) | |
| Other | 6 (5%) | 9 (10%) | |
| Previous myocardial infarct | 2 (2%) | 0 (0%) | 0.24 |
| Coronary artery disease ⁎ | 16 (12%) | 3 (3%) | 0.022 |
| Heart failure | 7 (5%) | 1 (1%) | 0.10 |
| Diabetes mellitus | 15 (11%) | 4 (4%) | 0.07 |
| Hypertension | 43 (32%) | 17 (19%) | 0.026 |
| Average alcohol consumption | 0.30 | ||
| Never (or none for >3 months) | 39 (31%) | 25 (30%) | |
| Rare (<1–2 drinks/month) | 14 (11%) | 15 (18%) | |
| Monthly (>1–2 drinks/month) | 14 (11%) | 12 (14%) | |
| Weekly (>1–2 drinks/week) | 29 (23%) | 19 (23%) | |
| Daily (1–2 drinks/day) | 26 (20%) | 8 (10%) | |
| >2 drinks/day | 5 (4%) | 4 (5%) |
⁎ Defined as present if there was any mention of coronary artery disease in the medical record.
One hundred ten patients (83%) with PAF and 68 (76%) with SVT answered questions regarding how frequently alcohol consumption provoked their episodes ( Table 2 ). Before multivariable adjustment, subjects with PAF were more likely to report alcohol as a trigger compared to those with SVT, but this association did not reach statistical significance ( Table 3 ). After multivariable adjustment, patients with PAF were significantly more likely to report that alcohol provoked their arrhythmia ( Table 3 ).
| Frequency | PAF | SVT |
|---|---|---|
| (n = 110) | (n = 68) | |
| Never | 86 (78%) | 59 (87%) |
| Rarely/sometimes | 16 (15%) | 8 (12%) |
| Often/always | 8 (7%) | 1 (1%) |
| Trigger | Unadjusted | Multivariable Adjustment | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Alcohol consumption | 1.90 | 0.83–4.36 | 0.13 | 4.42 ⁎ † | 1.35–14.44 | 0.014 |
| Vagal activation | 1.14 | 0.66–1.95 | 0.47 | 2.02 ⁎ | 1.02–4.00 | 0.044 |
| Sympathetic activation | 0.29 | 0.11–0.73 | 0.009 | 0.68 ⁎ ‡ | 0.21–2.18 | 0.52 |
⁎ Adjusted for age, gender, and race.
† Adjusted for binge drinking and average amount of alcohol consumption.
‡ Adjusted for presence of hypertension and congestive heart failure.
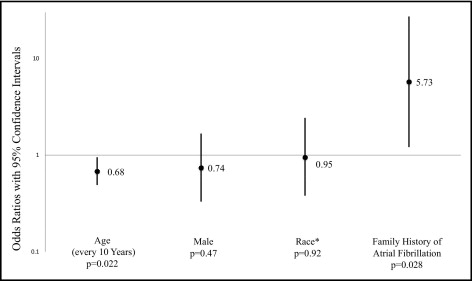
In a multivariate ordered logistic regression model including age, gender, race, and all covariates associated with alcohol as a trigger with a p value <0.1, only drinking primarily beer was independently associated with alcohol as a trigger in those with PAF ( Figure 1 ) .
Fifteen of the 28 patients who reported drinking primarily beer also reported drinking primarily wine or spirits. When those 15 were excluded, the analysis regarding drinking primarily beer as a predictor of alcohol triggering PAF was no longer statistically significant. However, when patients reporting >1 type of alcoholic beverage as their primary drink were grouped with those reporting drinking wine or spirits, no significant associations (unadjusted or adjusted) with alcohol as a trigger were observed.
One hundred thirty-two patients (99%) with PAF and 89 (99%) with SVT answered questions regarding activities that increased vagal tone. Overall, 111 (50%) reported that vagal activation precipitated their arrhythmia symptoms. Behaviors reported were resting/sleeping (n = 105, 95%), eating (n = 14, 13%), and symptoms that terminated with exercise (n = 17, 15%). After multivariable adjustment, patients with PAF were significantly more likely to report vagal activation as a trigger compared to those with SVT ( Table 3 ).
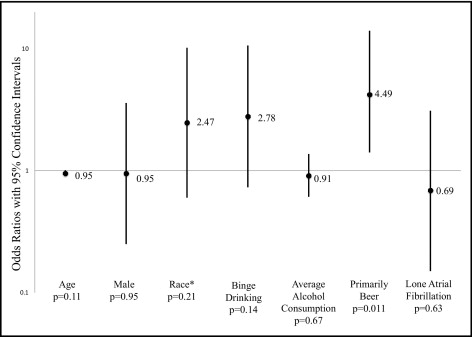
In a multivariate model designed to identify independent predictors of patients with PAF and vagal triggers, younger age and a family history of AF were significantly associated with having vagal triggers ( Figure 2 ) .