Chapter 34 Airway Management in the Intensive Care Unit*
Noninvasive Ventilation
Patients with respiratory failure and preserved airway reflexes may benefit from NIV. The rationale for this application, most commonly seen in acute exacerbations of chronic obstructive pulmonary disease (COPD), is that NIV may reduce the work of breathing and help to correct hypercapnic or hypoxic respiratory failure. NIV is contraindicated, however, with cardiovascular or respiratory instability, compromised ability to handle secretions, aspiration risk, or inability to tolerate a tight-fitting face mask (see Chapter 33 on NIV).
Airway Assessment
Predictors of Difficult Intubation
Examination of the patient should determine the following: ability to protrude the mandible, range of neck movement, atlantooccipital flexion and extension, interincisor distance (less than 3 cm indicates a high likelihood of difficulty), and modified Mallampati test (Figure 34-1). Other predictors of difficult intubation include thyromental distance of less than 7 cm (Patil’s test) and obesity. Further investigations when indicated could include the view of the larynx obtained at nasal endoscopy, which may predict the view at laryngoscopy; chest radiographs, which may show tracheal deviation or mediastinal masses; and CT scans, which may be useful when abnormal anatomy is suspected—for example, in association with tracheal stenosis.
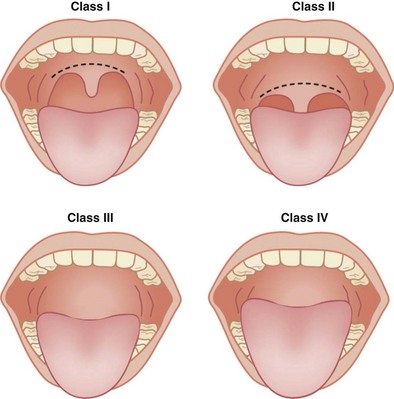
Figure 34-1 Mallampati test to classify view of the pharynx. For this test, the patient is asked to protrude the tongue fully while opening the mouth maximally, with the head in the neutral position. Class I: The pharyngeal pillars, soft palate, and uvula are visible. Class II: Only the soft palate and uvula are visible. Class III: Only the soft palate is seen. Class IV: Only the hard palate is seen. Mallampati class correlates with Cormack and Lehane grade for the view at laryngoscopy (see Figure 34-5). Increasing class suggests more difficult laryngoscopy.
Aspiration Risk
Aspiration of gastric contents can cause significant morbidity and mortality. Evidence suggests that reducing gastric volume and increasing pH of gastric contents will limit the risk of disorders associated with aspiration. Acid aspiration may lead to a chemical pneumonitis, but aspiration of food particles can result in physical obstruction of the bronchial tree with secondary bacterial pneumonia (Box 34-1 and Table 34-1).
Table 34-1 Drugs to Reduce Aspiration Risk
| Drug Class | Specific Agent | Mechanism of Action |
|---|---|---|
| Histamine H2 receptor antagonists | Ranitidine 50 mg IV | Increases pH and decreases gastric volume |
| Proton pump inhibitors | Omeprazole 40 mg IV | Irreversibly binds H+/K+-ATPase; increases pH and decreases gastric volume |
| Nonparticulate antacids | 0.3 M sodium citrate, 10 mL | Neutralizes gastric pH but increases volume Very effective at increasing gastric pH if given within 30 minutes |
| Prokinetics | Metoclopramide 10 mg | Reduces gastric volume |
Endotracheal Intubation with Muscle Relaxation
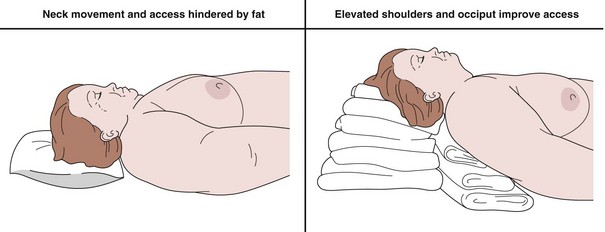
Positioning
Putting the patient in the optimal position is the first and most important step. Appropriate positioning allows good access to the airway and allows efficient preoxygenation. Other advantages include improvement of the laryngoscopic view and, with the head held slightly up, a reduced risk for aspiration of gastric contents. The “head-up” position also increases functional residual capacity by allowing better diaphragmatic excursion, thereby increasing oxygen reserves. The patient should be positioned with the neck flexed on a pillow, but with the head extended, so long as cervical spine injury is not suspected. Positioning is of particular importance in the obese patient (Figure 34-2).