Fig. 8.1
Nonenhanced thin-section CT scan of a 26-year-old female who underwent bilateral lung transplantation 6 months before due to cystic fibrosis. She went to hospital due to recurrent fever, emesis with some nonproductive cough, and global deterioration. FEV1 was 2.3l (71%). CMV pp65 antigenemia was mild positive (260 IU/ml). Bronchopneumonic infiltration was evident on CT in the right lower lobe (B + C) as well as the causal stenosis of the right main stem bronchus (a). Multiplanar reformat and postprocessing helped to identify the stenosis and to quantify its severity and extent (b, c, d). Virtual bronchoscopy was calculated for demonstration purposes and matches well with real bronchoscopic view. Biopsy was taken to differentiate between graft rejection and infection (the latter was the reason). (a) Transversal CT scan, (b) coronal reformat, (c) paracoronal reformat (single oblique), (d) surface-shaded rendering, (e) virtual bronchoscopy
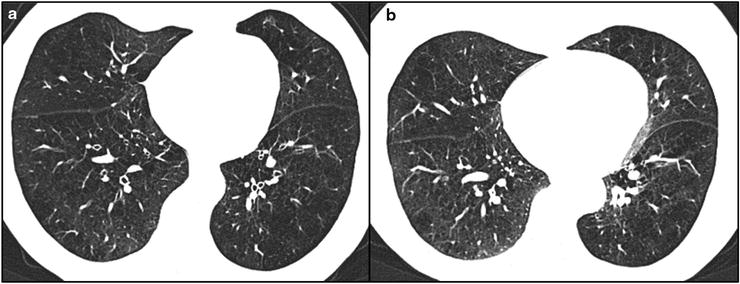
Fig. 8.2
The 57-year-old patient acquired 30 pack years and suffered from COPD IV°. She was planned for interventional emphysema therapy and therefore underwent paired inspiratory (a) and expiratory (b) thin-section CT scan. A special window-level setting (width 1,000 HU, level – 800 HU) demonstrated the inhomogeneous density of the lung parenchyma in both breath holds (a + b), especially in the expiratory one (b). There are subsegmental regions with adequate increase after expiration (right lower lobe), representing a relative increase of tissue per voxel. In contrast, other subsegmental areas did not change their density in expiration (left lower lobe), indicating air trapping as an indirect sign of obstructive small airway disease. Besides the indirect signs, also direct collapse of the segmental airways is visible in this image pair: All segmental bronchi are open at inspiratory CT (a), while almost all airways appear to be collapsed at the expiratory scan (b)
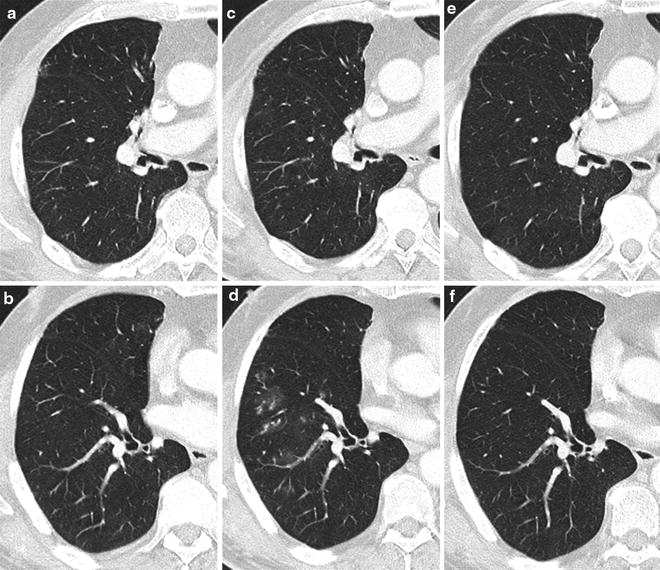
Fig. 8.3
(a + b) Prescan, (c + d) presentation, and (e + f) 6 months later, (a + c + e) at an lower lobe segmental ramification level. (b + d + f) Bronchus intermedius level. The 70-year-old patient was upper lobectomized right 4 years before due to stage I non-small-cell lung cancer and reported cough and bronchial infection since some weeks. The CT scan (c + d) demonstrated focal ill-defined nodules in the right lower lobe (c), which were newly developed as compared to the prescan (b). While analyzing the feeding bronchi, a bronchial kinking was evident in middle and right lower lobes. Together with the evident clinical symptoms, this was rated as bronchopneumonia, while pulmonary metastases were considered unlikely. The findings disappeared at the routine follow-up (e + f), indicating the infection to be treated successfully
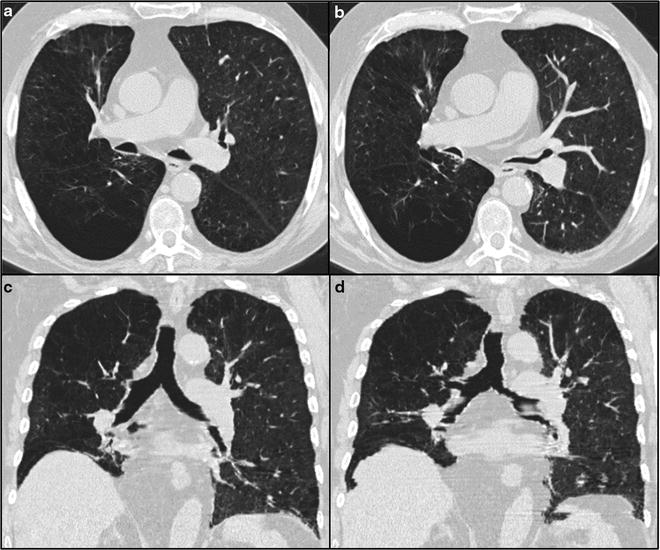
Fig. 8.4
The 81-year-old patient acquired 40 pack years and suffered from COPD III. He was planned for interventional emphysema therapy and therefore underwent paired inspiratory (a + c) and expiratory (b + d) thin-section CT scan. The comparison of the mainstem bronchi at inspiratory and expiratory CT indicates a relevant luminal change. The coronal reformat of the expiratory scan shows severe staring artifacts due to respiratory effect (d): Expiratory breath holding requires more compliance and pulmonary reserve as compared to inspiratory breath holding and is therefore frequently limited in patients suffering from severe lung disease. In this clinical scenario, fast CT scanning is relevant in particular since respiration artifacts occur in the expiratory scan (d). (a) Inspiratory breath hold, (b) expiratory breath hold, (c) coronal reformat of inspiratory breath hold, (d) coronal reformat of expiratory breath hold
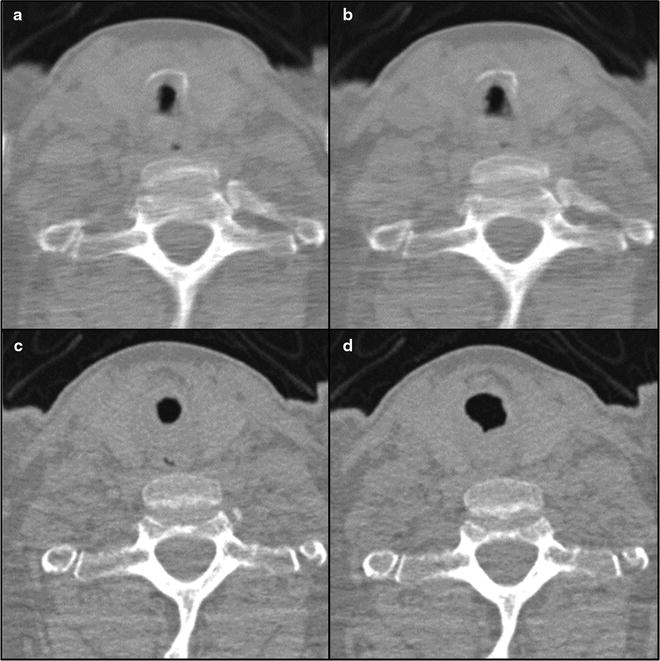
Fig. 8.5
(a) inspiratory breath hold, (b) expiratory breath hold, (c) maximal lumen in cine-CT, (d) expiratory breath hold. The 67-year-old patient was tracheotomized after substitution of mitral valve due to postoperative complications including seizure and pneumonia 2 months ago. Paired inspiratory and expiratory CT showed stenosis of the trachea at the level of tracheotomy (a + b). Cine-CT acquired during continuous respiration demonstrated additionally a relevant collapse at this level (c + d). Thus, an end-to-end resection of 3.5-cm trachea was performed
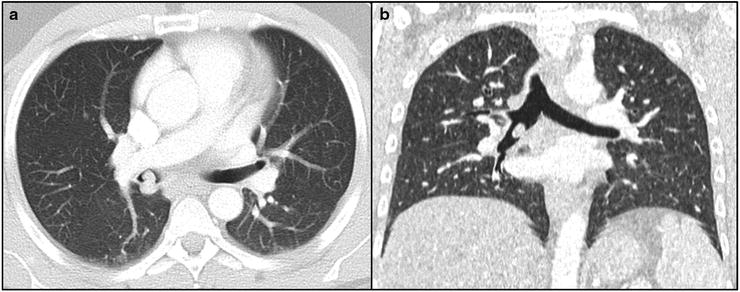
Fig. 8.6
(a) transversal CT, (b) coronal reformat. The 37-year-old male patient presented with hemoptysis. CT revealed polypoid mass in the bronchus intermedius (a + b), which was identified as typical carcinoid using bronchoscopy. Circular segmental resection of the bronchus intermedius was performed
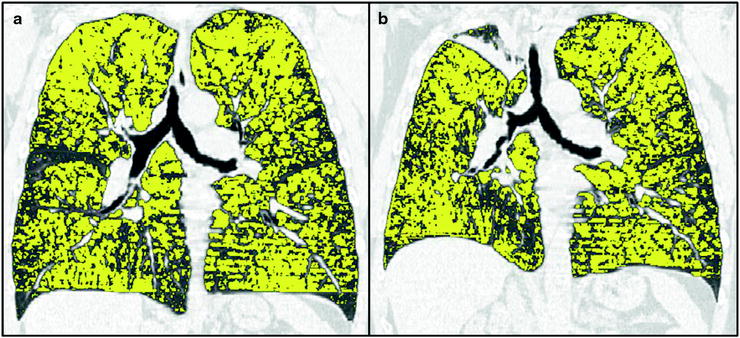
Fig. 8.7




The 61-year-old male patient acquired 60 pack years and presented COPD IV (FEV1 0.5 l, 6-min walk test 150 m). CT revealed severe diffuse bilateral centrilobular emphysema (emphysema index 48%, 15th percentile -983HU). After endobronchial placement of three valves in the right upper lobe, subtotal upper lobe atelectasis was observed and analysis improved to FEV1 0.8 l (25%), 6-min walk test 200 m, emphysema index 46%, and 15th percentile -981HU. (a) Prescan, (b) post valve implantation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


