12
Agricultural environments and the food industry
As a trade, food processing is tremendously diverse. Ranging from agriculture and fishing, to slaughtering and raw processing of foods to refined processing and cooking, the numerous and varied jobs offer countless types of potentially hazardous exposures. Exposure to airborne particles of organic material is the cause of a diversity of clinical conditions in all of the jobs within the group. Comprehensive reviews on the specific diseases related to farming are found in Linaker and Smedley [1] and in Schenker et al. [2]. Excellent reviews also exist in relation to bakery and seafood workers and to several of the other jobs within these trades. The history of disease related to crop, soil and animal contact is the oldest in the history of man’s occupational exposures. Descriptions of respiratory problems arising from such contact can be found in several ancient texts, many of which describe symptoms of readily recognizable conditions such as pneumonitis or chronic bronchitis, whereas asthma and rhinitis – the two respiratory conditions most widely associated with farming today – are less easily recognized. We do not know whether or not allergic reactions were less common in man’s long history of farming than they are today. Certainly this question has attracted much recent attention in relation to the ‘hygiene hypothesis’.
12.2 Agriculture and agribusiness
In Table 12.1 are listed the most common respiratory hazards in farming. Typical job types include:
Table 12.1 Possible respiratory hazards in agriculture
| Pollen and other seasonal allergens Organic dust from grain and other crops of microbial origin (molds, spores, bacteria, endotoxin and other toxins) Mites Animal (dander, urine, faeces) Inorganic dust (mainly silicates and other minerals from soil) Gases and fumes from slurry/manure and fertilizers – carbon dioxide, ammonia, hydrogen sulfide, methane from silage – nitrogen dioxide and carbon dioxide engine exhaust fumes welding fumes Chemicals pesticides (insecticides, herbicides, fungicides) disinfectants and cleaning agents paints Infectious agents (zoonoses) |
- field preparation and harvesting, mostly with machinery that creates dust, especially in dry weather;
- maintenance of machines and buildings, resulting in exposure to diesel exhaust and different chemicals and dust;
- application of and potential exposure to pesticides and other toxins;
- handling of a great variety of crops with exposure to dust from these and from plant debris;
- storage of crops and feedstuffs with potential exposure to molds and mites;
- handling of animals with direct contact and exposure to their allergens in addition to infectious agents from them;
- work in animal houses with exposure to complex mixes of bioaerosols and gases from feed, animals and manure;
- storage and handling of manure and fertilizers with exposure to these in the form of aerosols or gases;
- cleaning of animal houses with pressurized water, which liberates extremely high concentrations of humid aerosolized material of mostly organic origin.
Farmers as well as farm workers and farm dwellers are thus exposed to different kinds of dust throughout life. Depending on the type of farming, the region, climate and season, this exposure may be dominated by dry soil components (e.g. among crop farmers in dry climates during soil preparation and harvesting), by dusts from the crops themselves (e.g. from handling grain) or by the more humid bioaerosols containing dead and live microorganisms that are present in high concentrations in most animal houses. Farms are becoming ever larger and more specialized in most parts of the world. Most modern farmers specialize in producing only one or a few types of products rather than a range of different animals and crops on their farms. These changes in farming result in longer work periods with more uniform exposures (e.g. inside swine houses) and can result in much higher doses of airway irritants or allergens. On the other hand, larger operations will allow for more of the work to be performed by machines unsupervised by the farmer, potentially reducing the exposures. As single farming operations grow with more workers employed, groups of employees who are not traditionally considered farmers become exposed to the hazards of farming. Some of these workers have little knowledge about these hazards and may decline the use of respiratory protection if such protection is offered to them at all.
Migrant farm workers, numerous in southern USA but common in farming almost anywhere in the world, are particularly vulnerable to the hazards of farming. They may be particularly prone to acute reactions such as reactive airways dysfunction syndrome (RADS), organic dust toxic syndrome (ODTS), hypersensitivity pneumonitis (HP), and to poisoning from inhalation or skin contact with pesticides. Nor does the seasonality of their work protect them from developing chronic diseases such as asthma or chronic bronchitis. City-dwellers, another group not commonly thought of as exposed to farming, make up an important workforce in the production of fruit, vegetables, and flowers, e.g. in greenhouses, because many of these operations are located close to towns.
Farmers and farm workers commonly report respiratory symptoms such as wheeze, dyspnoea and cough. These symptoms are relatively nonspecific and can be caused by several occupational respiratory disorders, chronic as well as transient. However, persistent symptoms are not rare. Symptom prevalences from a study of 4.793 European farmers revealed prevalences of 3.3% for asthma, 14.9% for wheeze, 12.4% for chronic phlegm, 14.4% for nasal symptoms and 12.4% for toxic pneumonitis (ODTS). In California, prevalences of chronic symptoms or diseases in a farming population have been reported for persistent wheeze at 8.6%, for chronic bronchitis at 3.8%, for chronic cough at 4.2% and for asthma at 7.8%.
In any type of farming, exposure to allergens is very common – see Table 12.3 for common examples. A farmer presenting with rhinorrhea, nasal congestion, nasal itching and sneeze, often accompanied by symptoms of conjunctivitis, is likely to have irritative or allergic rhinitis. As most farmers work outdoors in close contact with plants from spring to autumn, they are highly exposed to pollen with the potential of causing sensitization. Seasonality may be less pronounced in an allergic farmer than in other patients because farmers expose themselves perennially to feedstuff and animals, and because irritative reactions to diverse types of dust may maintain the nasal symptoms for prolonged periods. Indeed, irritative mechanisms probably explain the majority of upper airway and eye symptoms among farmers since such symptoms are very common (some studies suggest that more than 50% of farmers suffer from them), while allergic sensitization seems to be rarer than in the general population. Greenhouse workers, less affected by seasonal variations in exposure, are often in contact with plants with a large allergenic potential. In addition to dermatitis, conditions such as allergic rhinitis and asthma are common and are likely to cause many to change their occupation. In recent years different species of bacteria and small insects have been introduced in large numbers into greenhouses as alternative methods of combating plant disease. Sensitization to some of these species has been observed, but apparently only little illness has emerged from their use.
Table 12.3 Some of the most common causes of allergic asthma in agriculture and food processing
| Animal-derived allergens cow dander (cow allergen Bos d 2) egg proteins (ovalbumin, conalbumin, lysozyme, ovomucoid) bird antigens (bird serum albumins Gal d 5) laboratory animal allergens (rat, mouse, guinea pig, rabbit, etc.) seafood and fish allergens (snow crab, Alaska king crab, lobster, shrimp, salmon, trout, etc.) Plant-derived allergens grain dust and cereal flours (wheat, rye, soya, barley, etc.) coffee beans and tea dust foods such as potato, onion, carrot, asparagus and several less common ones castor beans seeds (e.g. from onion, sunflower, sesame) garlic dust and other spices and herbs flowers (Lathyrus, Gypsophila, Freesia, Hyacinthus, and other common decorative flower species) vegetable gums (arabic gum, tragacanth and others and seed gums such as carob gum and guar gum) Parasites Anisakis simplex (in fish) Insects Mites (predatory mites in greenhouses and storage mites in grains) Molds and other microorganisms S. cerevisiae (yeast) Aspergillus (in bakers) Enzymes α-amylase (additive to baking flour) papain (in production of meat, juices, beer, etc.) pepsin (in production of liquors, cheese, cereals, etc.) pectinase (in fruit juice production) B-gluconase (additive to animal feed) |
Much agricultural dust is so coarse that its penetration beyond the larynx is limited and symptoms arising from exposure may be restricted to the upper airways – including cough to ‘clear the throat’. Examples include allergic rhinitis caused by olive pollen in olive orchard workers, allergic rhinoconjunctivitis in greenhouse workers caused by exposure to predatory mites used as pest control agents and storage mites in farmers, allergic sensitization to horses accompanied by rhinitis and/or conjunctivitis in grooms and cow dander allergy and rhinitis in dairy farmers. The latter may illustrate the diversity of exposure even within the same type of farming as in Finland daily brushing of cows is common and they are kept indoor most of the year, causing respiratory allergies in a large proportion of dairy farmers. These allergies are not nearly as common in other countries with different farming traditions and climates.
Farmer’s lung is a form of hypersensitivity pneumonitis, a respiratory disease caused by an exaggerated immune response to inhaled antigens; it was probably the first described occupational lung disease and typically occurs in dairy farmers exposed to dust that originates from poorly stored hay, straw, grain or similar plant material. Table 12.2 lists several of the most common types of exposures related with this disease. When any foliage is stored with a relatively high water content, i.e. above 15% humidity, heating occurs. This heating is initiated by an initial proliferation of lactobacteria, creating an ideal milieu for the growth of thermoactinomyces including Saccharopolyspora rectivirgula (SR) (formerly known as Micropolyspora faeni). When a farmer feeds this material to his animals in the following winter, when the barn’s ventilation is minimal, he or she is exposed to large quantities of dust containing dried antigens derived from this microorganism. This bioaerosol is generated not only by the direct handling of the material but also by shaking when the animals eat their feed. It is quite possible that a co-factor is needed to induce farmer’s lung disease. This co-factor could be endotoxin – abundantly present on farms – or a concomitant respiratory viral infection. Farmers’ lung can be acute with transient fever, chills and dyspnoea occurring 3-8 hours after exposure, or more indolent with progressive shortness of breath. Acute bouts usually heal completely while the more insidious form can lead to irreversible lung destruction in the form of fibrosis. The diagnosis is supported by the history of typical exposure and symptoms, restrictive lung function measurements, infiltrates on chest X-rays and high-resolution computed tomography (HRCT), and specific serum antibodies to the offending antigen. If the diagnosis is uncertain, a bronchoalveolar lavage should be obtained; a high number and percentage of lymphocytes in the bronchoalveolar lavage (BAL) fluid would clearly support the diagnosis while the absence of a lymphocytosis would rule out active HP. Although the confirmation of the diagnosis requires technology and expertise not readily available to the family physician, the first-line physician should through careful questioning and physical examination (bilateral inspiratory crackles) be able to suspect the diagnosis. The diagnosis is strongly supported by documented recurrence 3-8 hours after re-exposure to the farmer’s work environment.
Table 12.2 Some of the most common causes of hypersensitivity pneumonitis in agriculture and food processing (depending on climate) and the disease named thereafter
| Cause | Disease name |
| Moldy hay | Farmer’s lung disease |
| Moldy pressed sugarcane | Bagassosis |
| Moldy compost and mushrooms | Mushroom picker’s disease |
| Moldy cork | Suberosis |
| Contaminated barley | Malt worker’s disease |
| Contaminated maple logs | Maple bark disease |
| Contaminated redwood dust | Sequoisis |
| Contaminated wood pulp | Wood pulp worker’s disease |
| Cheese or cheese casings | Cheese washer’s disease |
| Greenhouse soil | Greenhouse lung |
| Mold on tobacco | Tobacco worker’s disease |
| Mold on grapes | Wine grower’s lung |
| Mold on peat moss | Peat moss lung |
| Pigeon droppings | Pigeon breeder’s disease |
| Chicken feathers | Chicken breeder’s disease |
| Oyster or mollusk shells | Shell lung |
Farmer’s lung is a relatively rare disease. The current estimated prevalence in appropriately moist agricultural regions is less than one case per 1000 dairy farmers per year. A doctor working in a rural setting, even in such areas where the disease is prevalent, might see one or two cases in his or her lifetime. As for any ‘orphan disease’, the fewer cases a doctor sees, the less likely it is that he or she will think of the diagnosis. It is important therefore for any family physician to keep the diagnosis of HP (or farmer’s lung if the patient is a farmer) in mind. HP should be ruled out in any case presenting with recurrent febrile episodes or an interstitial lung disease. Even if asked about exposures, many farmers may not be aware of exposure to partly degraded hay or other animal feed because it is such a common situation on many farms and the antigens may have formed months before the farmer handled the material.
A 65-year-old nonsmoking dairy farmer was brought to the hospital in respiratory distress. He had a high fever, inspiratory crackles and bilateral lung infiltrates. No detailed history was possible as the patient was intubated and mechanically ventilated with supplemental oxygen. He was given broad spectrum intravenous antibiotics. His condition rapidly improved and he was weaned off the respirator within 2 days and released from the hospital within 5 days of admission to continue oral antibiotics. Final diagnosis was bilateral pneumonia (no pathogens had been identified). The patient returned to the hospital a week later complaining of shortness of breath and chills. At this time a complete history revealed that he was a dairy farmer who had recently been using poorly conserved hay as bedding for his cows. The hay was so poor that he had used a chain saw to cut the bales into sections. The diagnosis of farmer’s lung was confirmed by serology, CT scan and BAL. His recovery was complete and, by changing his work environment, he was able to continue farming without recurrence.
Care must be taken to differentiate farmer’s lung from an infectious process or inhalation fever such as ODTS. ODTS also occurs in dairy farmers but in this case the exposure to moldy bioaerosols is massive, e.g. when decapping a haylage silo. The response is limited to the airways but extends to the alveoli. It is caused by toxic material in the dust. ODTS is also called toxic pneumonitits and has previously been called mycotoxicosis. The latter name was changed when it became evident that the toxic material which causes it is most likely also derived from bacteria (e.g. endotoxins). This self-limiting syndrome is not an immune-mediated disease. As for farmer’s lung, the diagnosis of ODTS can usually be made simply by careful questioning and by remembering this possibility. There are no standardized diagnostic criteria; the diagnosis is only made by history and follow-up and by ruling out other diagnoses such as an infectious process and farmer’s lung. The dyspnoea, fever, cough and malaise appearing a few hours after exposure resemble HP but symptoms resolve spontaneously within 1-2 days. It is likely that more than one agent can give rise to the syndrome and that some of the mixes of agents present, e.g. in animal houses and stables, are more potent than single agents.
A 42-year-old corn producer came to the hospital emergency room complaining of severe cough and chills since the evening before. His cough was unrelenting but he produced very little, blood-tinged sputum. Awaiting his turn to see the physician the receiving nurse obtained his vital signs. He had a fever of 39 C, his pulse was regular at a frequency of 140 beats/minute and his blood pressure was 140/94. A chest radiograph and spirometry were obtained, both of which were normal. Upon questioning the patient reported that he had been cleaning one of his corn silos the day before. He had spent 2 hours cleaning moldy grains of corn that remained on the edges of the otherwise empty silo. The doctor suspected an acute infectious bronchitis and was about to prescribe an antibiotic when the patient reported prior similar, although less severe, episodes after cleaning his silos in the past. With this additional information the doctor prescribed a cough suppression agent and aspirin. The patient was told he probably had ODTS and asked to return if the symptoms had not cleared within 24 hours. His recovery was uneventful, confirming that the diagnosis had probably been correct.
12.5 Symptoms not related to allergen exposure
A common disease entity among farmers is the ‘asthma-like syndrome’ with reported prevalences in some European farming populations of 20-50%. The syndrome resembles asthma as it can present with chest tightness, wheeze and dyspnea. Allergic reactions are absent. In contrast to the common worsening of asthma during a work week, the symptoms of asthma-like disease tend to improve as the working week progresses. Some allergic asthma may, occasionally, show the same pattern or in contrast may be worse on Saturdays after an entire week at work. In farming, such temporal patterns are usually very difficult to establish because work is rarely performed only on weekdays. Any episodic or persisting respiratory symptoms without systematic involvement are therefore evocative of asthma or asthma-like disease. Grain dust, ammonia and endotoxins have all been implicated in asthma-like disease – all of these exposures being common in animal houses. Endotoxins, ubiquitously present everywhere on farms and stemming from bacterial growth on feed, plant debris, in animal houses and elsewhere, have been associated not only with ODTS but also with worsening of asthma. Endotoxins are also commonly suspected of being at least partly responsible for asthma-like syndromes.
In a current or former farm worker or farmer presenting with a history of persistent or recurring productive cough and dyspnoea, chronic bronchitis is not unlikely even in a nonsmoker. In nonsmoking farmers and workers in animal confinement buildings, chronic obstructive pulmonary disease (COPD) has been found in 17%, with 3% having severe disease. COPD appears to be more common in older farmers than in comparable nonfarming populations. Several agents within the farming environment can reach and cause inflammation of the conductive airways: they include organic and inorganic dust, gases and fumes. Alone none of these has been convincingly demonstrated as a sufficient cause of COPD, but endotoxin in animal confinement buildings has repeatedly been associated with accelerated loss of lung function and with COPD. An increased risk of chronic bronchitis has also been found among farmers who have experienced ODTS. In dry climates an association of chronic bronchitis with dust exposure has been put forward. Furthermore, exposures to welding fumes, exhaust and smoke from fires are not uncommon among farm workers and may add to the risk of chronic bronchitis. Thus, whether the presenting symptoms are wheeze, dyspnoea, cough, chest tightness, or are less specific, any farmer reporting historic episodes of respiratory problems may well have some degree of COPD.
A farmer presenting with pulmonary fibrosis should be questioned about excessive exposure to dust from sand or soil or to the herbicide paraquat. Such inhalatory exposures are not uncommon during field work, but also occur when processing sugar beets, potatoes and grain or when burning straw etc., and can lead to fibrosis – an important diagnosis to consider in the dyspneic farmer.
Irritants like ammonia or other gases, cleaning agents, or other chemicals are regularly handled on farms. Accidental high exposure to many such irritants can cause RADS. RADS is not easily missed due to the new onset of asthma-like symptoms very shortly after unusual episodes of exposures. It is debated how long RADS can persist. Distinguishing between whether persisting symptoms represent an underlying asthma or if one should accept an entity called persisting RADS may be purely academic since both diseases may be caused by exposures at farms (and other workplaces with chemical irritants) and require anti-asthmatic treatment. At lower concentrations, gases from decomposing organic material can become concentrated in silos and cause respiratory irritation. Usually a self-limiting condition, such an inflammatory reaction of the airways to high concentrations of noxious gases can turn into life-threatening lung oedema or cause a long-lasting RADS. Suffocation or near death is not uncommon in such silos or in manure pits or other enclosed or low-level spaces that may fill with hydrogen sulfide.
Zoonoses are considered a rare cause of respiratory morbidity in farmers. Psittacosis, which is seen among poultry farmers due to their contact with infected birds, usually presents with nonproductive cough and other symptoms of a respiratory tract infection. Fever and other systemic symptoms will also be present. Bovine tuberculosis is well controlled in Europe and North America and infection of farmers has become rare. In some developing countries primary tuberculosis due to contact with cattle infected with Mycobacterium bovis remains a serious health problem. Fever may also be a symptom of Coxiella burnetii infection (Q fever) or other rare infectious diseases. Little is known about the prevalence of mild flu or cold-like viral infections transmitted from swine or other livestock. Such zoonoses may have become more prevalent because of higher density of animals in confinement buildings and because farm workers spend longer working hours inside these buildings. Farm workers, farmers and their relatives may if they present with airway infections or otitis, have been infected with multiresistant Staphylococcus aureus (MRSA), possibly transmitted from pigs. Such cases have been documented in recent years and are probably due to the frequent use of antibiotics not only for animal treatment but also as growth enhancers in most countries.
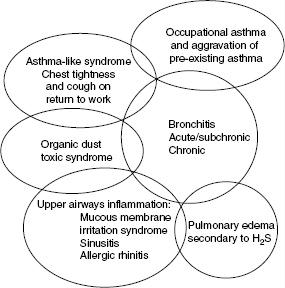
Acute symptoms of bronchoconstriction can be caused by organophosphates and carbamates used as pesticides in farming. A chemical pneumonitis can result from exposure to the very commonly used herbicide glycophosphate. Chronic pulmonary disease is rarely caused by pesticide exposure alone, but pulmonary fibrosis may be the result of exposure to the herbicide paraquat. The overlapping respiratory conditions associated with farming are illustrated in Figure 12.1.
Figure 12.1 The spectrum of respiratory disease in swine confinement workers. Adapted with permission from von Essen and Dosman
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


