A. Observe the patient without intervention
B. Perform cardiopulmonary exercise testing to determine need for intervention
C. Recommend surgical ASD closure only
D. Recommend surgical ASD closure with pulmonary venous baffle
E. Recommend device closure of the ASD
27. A 52-year-old woman falls while snow skiing and injures her wrist. On seeking medical care, a systolic murmur is identified, and she is referred for cardiac evaluation. She is normotensive. Her physical examination demonstrates a holosystolic murmur heard best at the left sternal border. An ECG is normal. A transthoracic echocardiogram demonstrates a muscular ventricular septal defect in the mid-septum with a peak systolic velocity of 5 m/s. There is no chamber enlargement. The right ventricular systolic pressure is estimated to be normal by tricuspid regurgitant velocity. Which of the following is the best initial management of this lesion?
A. No intervention
B. Surgical closure of the ventricular septal defect
C. Cardiac catheterization to quantify ventricular level shunting
D. Restriction of vigorous physical activity with no immediate intervention
E. Device closure of the ventricular septal defect
28. A 28-year-old man is found to have cardiomegaly on chest x-ray. An echocardiogram demonstrates flow acceleration at the level of the pulmonary valve (peak velocity 2.1 m/s) and moderate dilation of the right-sided chambers. Which of the following is the best next step?
A. Additional echocardiographic imaging to demonstrate patent ductus arteriosus
B. Additional echocardiographic imaging to demonstrate ASD
C. Cardiac catheterization with pulmonary balloon valvuloplasty
D. Serial annual evaluation to assess for ventricular dysfunction
E. Cardiopulmonary exercise testing
29. An 18-year-old woman had neonatal arterial switch operation for dextro-transposition of the great arteries (d-TGA). She presents to a cardiology clinic after 4 years without medical care. She has slowly developed exertional dyspnea and now can only climb one flight of stairs without resting. Her physical examination reveals normal jugular venous pressure and pulsation. A grade 3/6 ejection systolic murmur is audible at the upper left sternal border with no diastolic murmur. Which of the following is the most likely explanation of the symptoms?
A. Supravalvar pulmonary stenosis
B. Atrial fibrillation
C. Coronary ostial stenosis
D. Aorto-pulmonary window
E. Subacute bacterial endocarditis
30. A 40-year-old woman with a membranous ventricular septal defect underwent prosthetic patch repair as a child. Subsequently, at age 18 years, she was successfully treated for Streptococcal viridans endocarditis involving her mitral valve. Regarding future endocarditis prevention at the time of dental work, which of the following includes the most appropriate counseling?
A. S. viridans is an unusual pathogen for endocarditis
B. Prophylactic antibiotics are not indicated since there is no residual shunt
C. Prophylactic antibiotics are indicated due to history of bacterial endocarditis
D. Prophylactic antibiotics are indicated daily due to her history of VSD repair
E. No prophylactic antibiotics are indicated
31. A 43-year-old man with d-TGA underwent a Mustard procedure in early childhood. His pulse oximetry reveals an oxygen saturation of 96% at rest. His family history includes colon cancer in his father at the age of 40, and the patient is scheduled for elective colonoscopy. Regarding endocarditis prevention at the time of colonoscopy, which of the following includes the most appropriate counseling?
A. Routine antibiotic prophylaxis should be administered
B. Broad spectrum antibiotic prophylaxis with anaerobic coverage should be administered
C. No antibiotic prophylaxis is indicated
D. Full colonoscopy should be delayed due to endocarditis risk
E. Limited sigmoidoscopy should be performed
32. A 25-year-old man with Ebstein anomaly had a witnessed, transient loss of consciousness while walking down his apartment stairs immediately after eating dinner. He had brief upper extremity twitching as he regained consciousness. Evaluation in the emergency room reveals normal blood pressure and perfusion. The patient had no prodrome. His ECG demonstrates sinus rhythm, right atrial enlargement with prominent peaked P waves, first-degree atrioventricular block, and right bundle branch block. Which of the following is the most likely explanation for this patient’s symptoms?
A. Neurocardiogenic (vasovagal) syncope
B. Seizure disorder
C. Ventricular tachycardia
D. Atrioventricular re-entrant (accessory pathway) tachycardia
E. Complete heart block
33. A 32-year-old woman with tricuspid atresia underwent lateral tunnel Fontan palliation as a teenager. She has been followed since that intervention with minimal functional limitation. In the past 2 weeks, she has noted increasing abdominal girth and decreasing exercise tolerance. On examination, she is bradycardic and her liver edge is palpable 4 cm below the costal margin. Her ECG demonstrates junctional rhythm at 42 bpm. Which of the following is the most appropriate intervention needed?
A. Increased diuresis
B. Atrial pacemaker
C. Fontan revision surgery
D. Cardiopulmonary rehabilitation
E. Digoxin therapy
34. A 50-year-old man is undergoing right-sided diagnostic heart catheterization in the setting of biventricular systolic dysfunction. He acutely develops third-degree atrioventricular block and subsequent hypotension. A pacing catheter is placed emergently. An echocardiogram is performed in the catheterization suite and chordal attachments are noted from the left-sided atrioventricular valve to the interventricular septum. Which of the following is the underlying congenital lesion that explains these events?
A. Partial atrioventricular septal defect (AVSD)
B. Congenital pulmonary stenosis
C. Congenitally corrected transposition
D. Double-chamber right ventricle (DCRV)
E. Parachute mitral valve
35. A 41-year-old man is new to your practice after living in remote Africa for the past 5 years. He was born with pulmonary atresia with an intact ventricular septum, and palliation was performed in early childhood with placement of a central shunt. He has routinely had therapeutic 300 mL phlebotomy. He denies symptoms including headaches, visual changes, or other neurologic symptoms before or after phlebotomy. He is euvolemic on examination. His initial laboratory results include hemoglobin 21 g/dL and hematocrit 70%. Which of the following is the next best step?
A. Administer 500 mL isotonic crystalloid intravenously
B. Initiate therapeutic heparinization
C. Initiate iron chelation
D. Therapeutic phlebotomy with crystalloid volume replacement
E. Order serum iron studies
36. A 38-year-old woman with tetralogy of Fallot had a right ventricle to pulmonary artery homograft connection. She requires pulmonary valve replacement. She is an active smoker and has a family history of premature coronary artery disease. Fasting cholesterol panel is normal. Prior to surgical intervention that is scheduled in 1 week, which of the following is most urgent?
A. Tobacco cessation
B. Routine preoperative laboratory evaluation only
C. Coronary angiography
D. Prophylactic statin therapy
E. Surveillance blood cultures
37. An 18-year-old man is referred to you after his primary provider hears an early systolic click at the apex. Echocardiogram confirms a bicuspid aortic valve with normal function. There is no family history of heart disease. He has two healthy siblings, and he is accompanied by his parents. Your recommendations for the patient’s first-degree relatives should include which of the following?
A. Physical examination of first-degree relatives to assess for aortic valve click
B. Echocardiographic screening of all first-degree relatives
C. Cardiac MRI of any first-degree relatives with abnormal physical examination findings
D. Cardiac MRI of the patient to determine need for family screening
E. No evaluation of first-degree family members is needed
38. A 20-year-old woman returns for routine follow-up after repair of coarctation of the aorta in early childhood. Physical examination demonstrates normal femoral pulses and no brachiofemoral delay. Her right upper extremity and lower extremity blood pressures are equivalent. She has had serial echocardiograms demonstrating no re-coarctation of the aorta. At this time, ongoing evaluation should include which of the following?
A. Coronary angiography
B. Neurocognitive testing
C. MRI/MRA of the head and CT or MRI of the thoracic aorta
D. TEE
E. 24-hour Holter monitor
39. A 35-year-old patient with trisomy 21 and repaired partial AVSD is admitted for new onset atrial fibrillation with rapid ventricular conduction. The ventricular rate decreases appropriately with medical therapy and perfusion is normal. On physical examination, there is a prominent apical impulse, and a grade III/VI harsh systolic ejection murmur is heard at the upper sternal border. Echo reveals a mean left ventricular outflow tract (LVOT) gradient of 55 mm Hg at rest. Which of the following is the best choice for therapeutic intervention?
A. Chronic β-blockade therapy
B. Chronic amiodarone therapy
C. Chronic ACE inhibition
D. Aortic balloon valvuloplasty
E. Surgical outflow tract repair
40. A 35-year-old patient with trisomy 21 and repaired partial AVSD is admitted for new onset atrial fibrillation with rapid ventricular conduction. The ventricular rate decreases appropriately with medical therapy and perfusion is normal. On physical examination, there is a prominent apical impulse, and a grade III/VI harsh systolic ejection murmur is heard at the upper sternal border. Echo reveals a mean left ventricular outflow tract (LVOT) gradient of 55 mm Hg at rest. Which of the following is the best choice for therapeutic intervention?
A. Improved right ventricular pressure with adequate ventilation
B. Left ventricle to right atrial shunting
C. Doppler contamination with right ventricular outflow signal
D. Transient pulmonary vasospasm
E. No discrepancy is present
41. A 26-year-old man is prompted by his wife to return for cardiac care. His medical record describes a grade II/VI high-pitched holosystolic murmur consistent with known small membranous ventricular septal defect. On current examination, a right ventricular heave is present, and a prominent thrill is palpable at the left upper sternal margin. Which of the following is the most likely diagnosis?
A. Supravalvular pulmonary stenosis
B. DCRV
C. Increase in left ventricular pressure
D. Decrease in ventricular septal defect size
E. Increase in ventricular septal defect size
42. A 52-year-old tow truck driver had repair of tetralogy of Fallot at 4 years of age. He presents to the emergency department due to syncope while loading a car onto his truck. He had no prodromal symptoms. He had only the one surgery in childhood. He had last sought cardiac care in 1970. His ECG show sinus rhythm at 80 bpm, the PR interval is 100 ms. There is right bundle branch block and the QRS duration is 199 ms. An electrophysiology study is most appropriate to evaluate for which of the following?
A. Inducible ventricular arrhythmia
B. Inducible atrial arrhythmia
C. Sinus node dysfunction
D. Atrioventricular node dysfunction
E. Accessory pathway characteristics
43. A 40-year-old man with d-TGA underwent Mustard procedure in infancy. On examination, his heart rate is 40 bpm and regular. Resting oxygen saturation is 92%. Jugular venous pressure is elevated 10 cm above the angle of the sternum. ECG confirms junctional rhythm. Exercise testing elicits sinus rhythm with a peak heart rate of 65 bpm and with poor exercise capacity. Prior to transvenous pacemaker placement, evaluation should include which of the following?
A. Thrombophilia laboratory assessment
B. Computed tomography coronary angiography
C. Electrophysiology study to evaluate for inducible ventricular tachycardia
D. Cardiac catheterization to evaluate for SVC obstruction and baffle leak
E. Cardiac catheterization to evaluate for proximal coronary obstruction
44. A 25-year-old woman with d-TGA underwent arterial switch operation in infancy. Twice while shoveling snow, she developed a dull ache between her scapulae. Symptoms abated with rest. She walks up to 3 miles per day without symptoms. In addition to routine echocardiography, you would recommend which of the following?
A. Coronary angiography
B. Transesophageal echocardiogram
C. Fasting lipid panel
D. Cardiac MRI with gadolinium
E. No additional evaluation
45. A 35-year-old man with congenitally corrected L-TGA and no previous surgery was found to have periods of complete heart block. Therefore, a dual chamber transvenous pacemaker was placed. The echo immediately after the intervention demonstrated stable findings including mildly reduced systolic function of the systemic ventricle and minimal systemic atrioventricular valve regurgitation. Six months later, the patient returns with new onset of paroxysmal nocturnal dyspnea and decreased exercise tolerance. Pacemaker interrogation is unremarkable. Repeat echo demonstrates moderate systemic ventricular systolic dysfunction and moderate mitral valve regurgitation. Which of the following is the most likely explanation for these changes?
A. Myocardial ischemia
B. Pacemaker induced dysfunction
C. Paradoxical supraventricular tachycardia
D. Obstructive sleep apnea
E. Subacute bacterial endocarditis
46. A 32-year-old man with lateral tunnel Fontan palliation of tricuspid atresia presents to an emergency department with sinus tachycardia and tachypnea after a presyncopal event. There was concern for pulmonary embolism and after placing a right upper extremity IV, a ventilation perfusion scan (VQ scan) demonstrated no perfusion of the left lung with normal perfusion of the right lung. Prior to initiation of treatment for pulmonary embolus occluding the left pulmonary artery, what would you recommend that the treating team perform next?
A. Repeat the study with a lower extremity IV
B. Perform a transesophageal echocardiogram
C. Place a central venous line
D. Perform invasive pulmonary angiography
E. Draw blood for thrombophilia assays
47. A 48-year-old man undergoes computed tomography angiogram in the setting of exertional chest discomfort. His right coronary artery arises from the left coronary cusp of the aorta with a proximal intramural course, subsequently passing between the pulmonary artery and the aorta that are normally positioned. Which of the following is the best intervention?
A. Saphenous vein graft to the distal left main coronary artery
B. Internal mammary artery anastomosis to the distal left main coronary artery
C. Unroofing of intraarterial left main coronary artery
D. Coronary button translocation to the left coronary cusp
E. No intervention is indicated
48. A 30-year-old man with congenital heart disease repaired in infancy undergoes right-and left-sided cardiac catheterization with this anterior-posterior image of catheter position (Figure 12.2.). The course of the cardiac catheter (not the wire) is best described as which of the following?
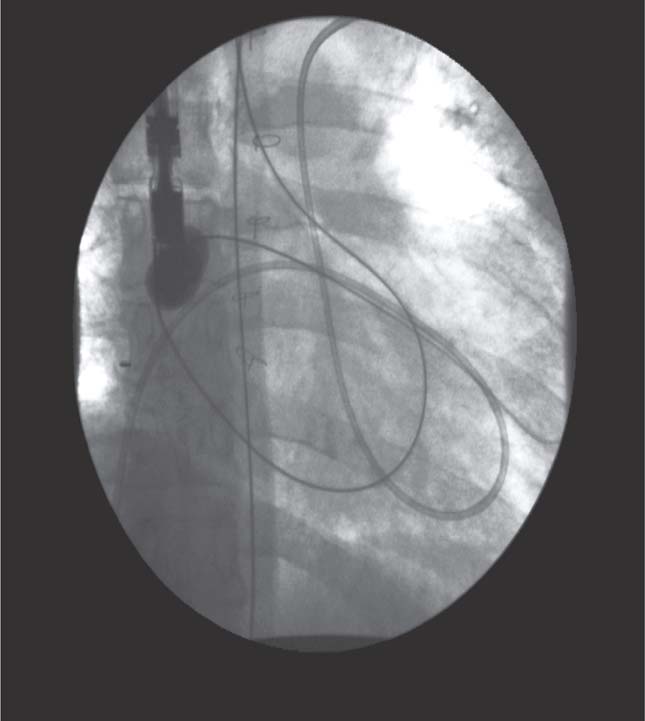
A. IVC, systemic venous baffle, mitral valve, morphologic left ventricle, aorta
B. IVC, systemic venous baffle, tricuspid valve, morphologic right ventricle, pulmonary artery
C. IVC, systemic venous baffle, mitral valve, morphologic left ventricle, pulmonary artery
D. IVC, systemic venous baffle, tricuspid valve, morphologic left ventricle, pulmonary artery
E. IVC, pulmonary venous baffle, tricuspid valve, morphologic right ventricle, pulmonary artery
Answers
1 ANSWER: C. The cardiac disease in pregnancy (CARPREG) investigators demonstrated in a prospective multicenter study that maternal cardiac risk could be predicted with the use of a risk index.1 Cardiac events were defined as pulmonary edema, arrhythmia, stroke, or cardiac death. The four predictors of primary cardiac events were (1) prior cardiac event, (2) baseline NYHA class >II or cyanosis, (3) left heart obstruction (mitral valve area <2 cm2, aortic valve area <1.5 cm2, or peak LVOT gradient >30 mm Hg by echocardiography), and (4) reduced systemic ventricular systolic function (ejection fraction <40%). The risk of maternal cardiac complication with zero predictors was 5%, with 1 predictor was 27%, and with greater than one predictor the risk was 75%. The risk score was further refined by the Boston Adult Congenital Heart Disease Group in a study that demonstrated that including decreased subpulmonary ventricular function and/or severe pulmonary regurgitation as a predictor in the risk index improved the accuracy of the risk assessment.2 Of the answers listed, the patient described in C has the highest predicted risk with a prior cardiac event (history of atrial fibrillation) and severe pulmonary valve regurgitation. Her poor peak VO2 may be a further indication of poor outcome, even if she has no complaints clinically. The patient in answer A has no predictors. The patient in answer D has 1 predictor. The patient in answer B could be considered to have 1 predictor—poor subpulmonary ventricular function.
2 ANSWER: C. ACE inhibitors can cause fetal renal dysfunction in the third trimester, but have also been demonstrated to be a teratogen. Therefore, ACE inhibitors should be avoided throughout pregnancy. ARBs should be considered to have the same risk profile and should be avoided. Hydralazine and nitrates are safe in pregnancy and together provide similar physiologic response to ACE inhibition.
3 ANSWER: D. Women with Eisenmenger syndrome are at exceptionally high risk of complication and death during pregnancy and the peripartum period. Pregnancy should be avoided in these patients.3 The patient described in answer A has one predictor of cardiac complication (predicted to have a complication risk of 25%) but has a low risk of death. Patients with Marfan syndrome can have dissection during pregnancy, but pregnancy is not absolutely contraindicated unless the aorta is larger than 40 mm. The patient described in answer C has a risk of cardiac complication, but no absolute contraindication.
4 ANSWER: D. Patients with mechanical valve prostheses pose significant difficulties for anticoagulation management. Warfarin probably provides the optimum anticoagulation, but it is a teratogen and should be avoided if possible during the first trimester of pregnancy. Also, warfarin crosses the placenta, and a fetus of a mother anticoagulated with warfarin should not be delivered vaginally secondary to the risk of fetal intracranial bleeding. However, studies have shown that if therapeutic anticoagulation can be achieved with a daily dose of <5 mg daily, the risk of warfarin embryopathy is quite low. A currently accepted management strategy is to provide alternative anticoagulation during at least the first trimester.4 Low molecular weight heparin is an attractive alternative to warfarin as it does not cross the placenta. However, weight-based dosing alone is not effective anticoagulation during pregnancy secondary to altered volume of distribution and drug metabolism. If low molecular weight heparins are used, anti-Xa levels must be followed closely (at least weekly) to ensure adequate anticoagulation.
5 ANSWER: E. Depo-Provera injection provides the best option for this patient, though there is some risk of hematoma at the injection site. Essure tubal implants are an irreversible form of contraception. Mirena IUD is reversible and safe to implant, but is not the best option in patients who are not monogamous as the incidence of pelvic inflammatory disease may be increased. Barrier contraception such as a diaphragm does not have the same efficacy as Depo-Provera, but the patient should be encouraged to use condoms with a new partner to prevent sexually transmitted disease. Estrogen containing oral contraception would not be a good choice in a patient at risk for thrombus.
6 ANSWER: B. This patient likely has Loeys–Dietz syndrome, a mutation of TGF-β receptor that results in arterial fragility. ARBs have been shown to reduce TGF-β signaling and reduce the risk of arterial complications in animal models. ARBs are the drug of choice in this situation. While patients with Loeys–Dietz can have aortic complication at this degree of dilatation, it is acceptable to follow closely with routine imaging at this aortic dimension.5
7 ANSWER: C. This patient had appropriate secondary erythrocytosis related to his cyanosis. This increase in hemoglobin is necessary to provide appropriate oxygen delivery and is not associated with stroke or other small vessel occlusion unless the patient is microcytic, as microcytotic red cells are less deformable as the traverse small capillary beds.6 This patient likely feels unwell because he has poor oxygen delivery. He should be treated with iron therapy for 1 month with a goal of normalizing the MCV and ferritin.
8 ANSWER: E. This patient has symptomatic aortic stenosis. Bedrest may be advisable, but 4 weeks is too long of a follow-up interval. Balloon valvotomy is not a good choice since the valve is calcified. Delivery of the fetus now is not optimal since this degree of prematurity would provide a high risk of neonatal complication and death. Percutaneous valve implantation is currently not an option in this situation and would likely carry some risk to mother and fetus. Surgical replacement of the aortic valve can be done with low risk to mother and relatively low risk to the fetus7 and is the best option in this scenario.
9 ANSWER: D. This patient is at higher risk of coronary artery disease given his history of coarctation. His LDL cholesterol goal should be 70mg/dL or less. Diet can be helpful, but the patient will benefit from a statin drug to lower LDL. Niaspan, fish oil, and gemfibrozil do not have significant LDL lowering effects.
10 ANSWER: D. This patient does need treatment for hypertension. While a recurrent coarctation can cause residual hypertension, there is no evidence from the echocardiogram that the patient has any significant residual obstruction; hence, stent implantation is unlikely to provide much benefit. This patient likely has hypertension related to stiff arterial vasculature and a relatively late coarctation repair. All the drugs listed can treat hypertension, but Metoprolol and Diltiazem would not be favored given the low resting heart rate. Daily Lasix will probably not be effective and controlling the hypertension and would not be a first-line choice. Losartan has the most advantages with a low side effect profile, no heart rate changes, and possible protection against aortic dilatation (for which this patient is at risk).
11 ANSWER: A. Patent foramen ovale is present in 25% to 30% of the adult population. Currently there are no data that treatment with medication or closure to prevent paradoxical emboli is indicated in an asymptomatic patient. Patent foramen ovale should not cause right ventricular volume overload; hence, MRI would not provide clinically useful information.
12 ANSWER: E. The patient has symptoms of platypnea-orthodeoxia syndrome, related to positional right-to-left shunting across a patent foramen ovale. Elderly patients with patent foramen ovale are more prone to right-to-left shunting as the cardiac geometry changes with age.8 A normal supine saturation would make this diagnosis more likely and then echocardiographic imaging could confirm. Treatment would be closure of the patent foramen ovale. Pulmonary function test with methacholine challenge would be helpful for diagnosing asthma, but asthma would not explain the patient’s decline in saturation. V/Q scan would be helpful to determine whether there had been pulmonary emboli, but the patient would potentially have right heart changes on echocardiography if emboli were so extensive to cause this degree of desaturation. Diastolic dysfunction or coronary artery disease can lead to dyspnea on exertion, but this degree of desaturation would be unlikely.
13 ANSWER: C. ASDs can cause right heart enlargement secondary to left-to-right shunting, but at this age and with the history of hypertension, it is possible that the left-to-right shunt volume is increased secondary to left ventricular diastolic dysfunction. If the left ventricular filling pressures are extremely high, the patient may become more dyspneic with closure of the ASD since the left atrial pressure will increase after ASD closure. Therefore, the best initial step in this patient’s evaluation is to perform left and right heart catheterization to determine filling pressures. If the pressures are elevated, an attempt at balloon occlusion of the ASD can be performed to ensure that left atrial pressures do not become excessively increased with ASD closure.
14 ANSWER: D. This patient has one risk factor—left heart obstruction (mitral valve area <2 cm2, aortic valve area <1.5 cm2, or peak LVOT gradient >30 mm Hg by echocardiography—on the CARPREG risk model.1 One risk factor predicts a risk of cardiac complication during pregnancy of 25%.
15 ANSWER: E. This patient is best served by transthoracic echocardiogram to evaluate the function of the left ventricle and the bicuspid aortic valve, MRI scan of the aorta to evaluate for thoracic aorta dilation and complications at the coarctation repair site, as well as MRA scan of the brain to evaluate for intracranial aneurysms since patients with a history of coarctation have an increased risk of intracranial aneurysm.3 The other choices listed could evaluate the heart and the thoracic aorta, but would not evaluate the intracranial vasculature.
16 ANSWER: A. Blood pressure medications can cause fatigue as a side effect, but this patient is complaining of hypersomnolence. Patients with Marfan syndrome should be screened for obstructive sleep apnea as they are at high risk for this condition, which can result in daytime hypersomnolence, hypertension, and aortic dilatation. Overnight oximetry is a simple, but effective, screening tool to evaluate possible obstructive sleep apnea.
17 ANSWER: A. Sertraline has a low risk of cardiac complications. Citalopram and Amitriptyline can cause prolonged QT that could be a problem in a patient with tetralogy of Fallot. Venlafaxine and Bupropion both inhibit the neuronal uptake of norepinephrine and can cause hypertension and tachycardia.
18 ANSWER: A. Dabigatran is an oral direct thrombin inhibitor. Unlike warfarin, Dabigatran therapy does not need to be monitored to ensure achievement of therapeutic anticoagulation. It is currently approved for use in patients with atrial fibrillation, but not for use with mechanical valves. There are no data currently regarding the use of this agent during pregnancy. Dabigatran is not useful for bridging anticoagulation as it is recommended that Dabigatran should be discontinued 1 to 2 days prior to surgery (with abnormal creatine clearance, this recommendation increases to 3 to 5 days). Dabigatran should not be used in patients with significant bleeding issues as there is no direct reversal agent available.
19 ANSWER: C. Concomitant use of amlodipine and simvastatin increases the risk of myopathy and rhabdomyolysis. If it is necessary to use both drugs, it is recommended that the dose of simvastatin do not exceed 20 mg/day.
20 ANSWER: B. Atenolol has an FDA pregnancy classification of class D—There is positive evidence of human fetal risk, but the benefits from use in pregnant women may be acceptable despite the risk (e.g., if the drug is needed in a life-threatening situation or for a serious disease for which safer drugs cannot be used or are ineffective)—because a study in hypertensive women taking atenolol demonstrated lower birthweight infants. The other drugs are labeled class C—Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal or other) and there are no controlled studies in women or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the fetus.
21 ANSWER: D. Endometrial ablation is a safe minimally invasive procedure that can reduce menstrual bleeding significantly (especially in women >35 years of age) and can be performed without interruption of anticoagulation. Endometrial ablation should not be performed in someone interested in becoming pregnant later. Hysterectomy can provide the same relief of symptoms, but for this patient to have hysterectomy, she would have to interrupt her warfarin anticoagulation and undergo a surgical procedure. Oral estrogen containing contraception can be a good choice to treat menometrorrhagia in some patients, but is not favorable in this patient secondary to the increased risk of thrombosis. Depo-Provera can improve menometrorrhagia, but is not as effective as endometrial ablation. Essure tubal ligation is good in preventing pregnancy, but does not treat menometrorrhagia.
22 ANSWER: E. Flecainide is a class IC antiarrhythmic agent. It can cause pro-arrhythmia and QRS prolongation, so is best initiated in hospital with continuous monitoring for five doses with a daily EKG to check the QRS duration.
23 ANSWER: A. Amiodarone can cause liver, pulmonary, and thyroid toxicity. Therefore, TSH, liver function tests, and pulmonary function tests should be monitored routinely. Liver function tests ideally should be reviewed twice yearly and thyroid function tests every 3 to 6 months.
24 ANSWER: A. One of the most common side effects of Bosentan is lower extremity edema. This side effect is not significant in the other drugs listed. β-blockers are not considered pulmonary vasodilators.
25 ANSWER: E. It is very important that the drug be taken at the same time daily for optimum effectiveness. It does not take 60 days for the pill to become effective. Rash can occur, but not sun sensitivity. Amenorrhea can occur, but is not the norm. Antibiotics may reduce the effectiveness of contraception, but patients who need SBE prophylaxis should continue using antibiotics when appropriate and be counseled to use alternative contraception for that cycle.
26 ANSWER: D. The physical examination and ECG are consistent with the echocardiographic image demonstrating a sinus venosus ASD with partial anomalous pulmonary venous return with the right superior pulmonary vein draining to the superior vena cava—right atrial junction. Given the cardiac chamber dilation with respiratory and exercise symptoms, it is appropriate to proceed with surgical intervention. ASD closure alone will allow persistent left-to-right shunting through the right superior pulmonary vein. To eliminate this shunt and volume load of the right heart, ASD closure and surgical pulmonary venous redirection to the left atrium are indicated. Device closure is reserved for secundum defects only.
27 ANSWER: A. Small ventricular septal defects may be detected at any age, particularly in patients who have avoided medical care. Management of this newly discovered lesion is based on the hemodynamic effects of the lesion. Evidence that the ventricular level shunt is small and of no hemodynamic consequence includes the absence of left atrial and ventricular chamber enlargement, normal right ventricular systolic pressure, and a very high flow velocity across the ventricular septal defect, although the latter may be the least trustworthy of these findings. No intervention or additional evaluation is required. The patient should be reassured about the benign nature of this lesion. There is no need for SBE prophylaxis.
28 ANSWER: B. The flow acceleration demonstrated by echocardiogram is mildly elevated. However, mild pulmonary stenosis should not result in right atrial and right ventricular chamber enlargement. Additional evaluation is needed to explain the chamber dilation. A patent ductus arteriosus and normal pulmonary vascular resistance result in increased pulmonary venous return and enlarged left-sided chambers. A hemodynamically significant ASD would result in left-to-right shunting with right atrial and right ventricular dilation.
29 ANSWER: A. Arterial switch operation for d-TGA has been the preferred surgical procedure since the early 1980s. The most common late postoperative complication for the arterial switch operation is supravalvar pulmonary stenosis. This may be amenable to stent implantation with care taken to avoid the pulmonary valve. Balloon valvuloplasty without stenting has a low success rate. Stenosis of the aorta is less common. Coronary ostial stenosis is a known complication but is not consistent with the physical examination. Atrial arrhythmias late after arterial switch operation are rare.
30 ANSWER: C. The 2007 ACC/AHA guidelines continue to recommend prophylactic antibiotics prior to dental work for anyone with a prior history of bacterial endocarditis. For nonvalvular prosthetic patch material, antibiotic prophylaxis is recommended for only the first 6 months following surgery. There is no indication for daily antibiotics. S. viridans remains a common pathogen for infective endocarditis.
31 ANSWER: C. Antibiotic prophylaxis is not indicated for patients undergoing nondental interventions (colonoscopy or upper endoscopy) in the absence of active systemic infection. Comprehensive care of patients with congenital heart disease includes preventative screening procedures at recommended ages.
32 ANSWER: C. While there is a clear association between Ebstein anomaly and atrioventricular reentrant accessory pathway tachycardia, patients with Ebstein anomaly are also at risk for life-threatening ventricular arrhythmias. This is particularly true for patients with deterioration in hemodynamic status. Atrioventricular re-entrant accessory pathway tachycardia is less likely to cause a sudden loss of consciousness. The absence of prodromal symptoms also makes a ventricular tachycardia more likely. Myoclonus is common in any loss of consciousness. This patient requires additional arrhythmia monitoring and evaluation of hemodynamic status and cardiac function.
33 ANSWER: B. The symptoms and physical examination findings are consistent with elevated IVC and central venous pressures in this Fontan patient’s circulation. While these symptoms could be consistent with obstruction in the Fontan connection, the ECG demonstrates junctional bradycardia. This is a common and often delayed finding in multiple forms of congenital heart disease after Mustard, Senning, and Fontan procedures. The onset of junctional rhythm may cause significant hemodynamic impact. This is a class I indication for atrial or dual chamber pacemaker placement.
34 ANSWER: C. In congenitally corrected TGA, the conduction system is abnormal in location and structure, making it vulnerable to physical trauma during catheterization in addition to spontaneous heart block associated with increasing age. The diagnosis of this congenital cardiac abnormality may be delayed into adulthood in individuals with adequate systemic ventricular function and no obvious murmur from a VSD or pulmonary/subpulmonary stenosis.
35 ANSWER: E. Routine phlebotomy for erythrocytosis in cyanotic patients is not recommended in the absence of symptoms and often leads to iron deficiency anemia with resulting microcytosis. Microcytosis independently increases viscosity, perpetuating a cycle of phlebotomy and worsening microcytosis leading to symptoms. For euvolemic patients with hemoglobin >20 g/dL and hematocrit >65% with symptoms of hyperviscosity, therapeutic phlebotomy with equal volume crystalloid replacement is indicated.
36 ANSWER: C. The 2006 ACC/AHA guidelines for the management of patients with valvular heart disease recommend cardiac catheterization with coronary angiography for symptomatic men 35 years or older, women 35 years or older with coronary artery disease risk factors, and all postmenopausal women. Tobacco cessation 1 week prior to surgery may increase respiratory secretions in the perioperative period. There is no indication for statin therapy at this time. From the 2006 ACC/AHA Guideline statement (JACC. 2006;48:659): In general, because angina is a poor marker of CAD in patients with AS, coronary angiography is recommended in symptomatic patients before AVR in men older than 35 years; premenopausal women older than 35 years with coronary risk factors, as well as asymptomatic men older than 45 years; women older than 55 years; or those with 2 or more coronary risk factors.
37 ANSWER: B. Both bicuspid aortic valve anatomy and isolated ascending aortic dilation have been identified in first degree family members of patients with bicuspid aortic valve. The abnormalities resulting in bicuspid aortic valves have clear association with abnormal aortic dilation and are not a process isolated to the aortic valve alone. For patients with bicuspid aortic valve, all first-degree relatives should be screened with transthoracic echocardiograms. Cardiac MRI is not recommended as first-line screening. Screening is recommended regardless of physical examination findings since ascending aortic dilation may be present in the setting of a normal physical examination.
38 ANSWER: C. Patients with repaired coarctation of the aorta have associated risk for cerebral aneurysms and for pseudoaneurysm formation at the site of prior surgical repair. While there is no evidence of aortic recoarctation by physical examination or by echocardiographic evaluation of the aortic lumen and blood flow, this does not exclude pseudoaneurysm formation. CT or MRI imaging of the thoracic aorta should be performed. Cardiac catheterization is not required. Head MRI with MR angiography may be utilized for cerebral aneurysm screening. Neurocognitive testing may be appropriate for an individualized patient.
39 ANSWER: E. Late postoperative complications following AVSD repair include LVOT obstruction, heart block, and left atrioventricular valve regurgitation. New onset of atrial arrhythmias should prompt a thorough anatomic and hemodynamic evaluation for postoperative complications resulting in atrial fibrillation. Treating the arrhythmia with medical therapy without additional evaluation is insufficient. Isolated LVOT obstruction with a mean gradient >50 mm Hg or a maximum instantaneous gradient >70 mm Hg is an indication for surgical intervention. Afterload reduction with ACE inhibition is relatively contraindicated in the presence of fixed LVOT obstruction and may result in hypotension and coronary hypoperfusion.
40 ANSWER: B. Left ventricle to right atrial shunting in the setting of normal right sided pressures results in a high-velocity left-to-right shunt. This Doppler signal may contaminate the tricuspid regurgitation signal. Initiation of pulmonary vasodilator therapy without additional investigation would be inappropriate. Patients with trisomy 21 are at increased risk of obstructive sleep apnea and pulmonary hypertension.
41 ANSWER: B. Isolated membranous ventricular septal defect is associated with the development of DCRV that may occur in adulthood. DCRV is defined by a proximal, upstream portion of the right ventricle that is at high pressure, separated by abnormal muscular hypertrophy from a more distal low pressure portion. The pulmonary arterial pressure is distal to the obstruction and should be normal. The development of DCRV is often heralded by an increase in murmur intensity, onset of a thrill, and findings of right ventricular pressure loading including an increased right ventricular impulse and RVH by ECG. Surgical resection of the muscle bundle is needed.
42 ANSWER: A. Risk factors for sudden death after repair of tetralogy of Fallot are QRS duration >180 ms, poor right ventricular hemodynamics, older age at repair, and prolonged palliative shunts. Invasive electrophysiology study is appropriate to provide additional risk stratification, but some would argue for internal defibrillator placement regardless of the outcome. Atrial arrhythmia and atrioventricular node dysfunction are both known complications following surgical repair, but are not the primary indication for additional electrophysiology study at this time.
43 ANSWER: D. Mustard and Senning atrial switch procedures are associated with sinus node dysfunction and atrial arrhythmias. Other complications are baffle leaks and baffle obstruction. Placement of transvenous, intracardiac pacemaker leads may worsen baffle stenosis, and paradoxical embolus may occur across a baffle leak. Incorrect positioning of ventricular leads across the baffles is also observed. Pacemaker placement in this patient should be performed at a center with experience in adult congenital cardiac care. There is no history given for thrombophilia. While sudden death does occur in patients with repaired d-TGA, there is no history of atrial or ventricular tachycardia in this patient even with exercise.
44 ANSWER: A. The arterial switch operation for d-TGA requires reimplantation of coronary artery buttons. There is risk of both early and late coronary obstruction. There is evidence that the risk may be greater with single coronary artery anatomy. Symptoms of coronary ischemia may present in atypical fashion. The history of exertional chest pain that resolved with rest warrants evaluation. Coronary angiography is the gold standard for coronary assessment, although computed tomography angiography may be appropriate.
45 ANSWER: B. Progressive systemic ventricular dysfunction may occur following initiation of ventricular pacing. The ventricular lead crosses the mitral valve (in L-TGA) and may cause mitral regurgitation. Following pacemaker placement, surveillance of the patient should be increased to detect these changes. Biventricular pacing may reverse these effects in some patients. Supraventricular tachycardia should be detected by pacemaker interrogation.
46 ANSWER: A. Patients with Fontan palliation are at increased risk for systemic venous thromboembolic events. Pulmonary embolism may present with variable symptoms, and this presentation is consistent with a pulmonary embolism but is not specific for this diagnosis. Streaming of blood flow in the Fontan circulation may result in superior vena cava blood flowing preferentially to one lung with inferior vena cava flow to the other lung. Contrast or isotope may need to be injected into upper and lower extremities to accurately demonstrate bilateral pulmonary perfusion. Invasive pulmonary angiography remains the gold standard, but may not be required in this scenario.
47 ANSWER: C. Anomalous coronary arteries are detected as incidental findings in the current era of advanced imaging. The intramural course of the anomalous artery in a long segment through the wall of the aorta is a risk factor for cardiac ischemia and death. The preferred intervention is an unroofing of this segment, opening the internal portion of the aortic wall to the aortic lumen. Bypass grafting a vessel that is not stenotic at baseline will typically result in a failed graft. Coronary button translocation is not required if unroofing is successful.
48 ANSWER: C. The anatomy demonstrated is d-TGA after a Mustard procedure. The wire and small balloon catheter can be traced retrograde from the aorta to the right-sided, morphologic right ventricle, tricuspid valve, and pulmonary venous baffle with a balloon inflated in the pulmonary venous baffle. The wire extends beyond the heart border in a left-sided pulmonary vein. The larger catheter can be followed antegrade through the inferior vena cava, systemic venous baffle, mitral valve, morphologic left ventricle, and proximal pulmonary artery. The pulmonary artery runs parallel to the aorta.
REFERENCES
1. Siu SC, Sermer M, Colman JM, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001;104(5):515–521.
2. Khairy P, Ouyang D, Fernandes SM, et al. Pregnancy outcomes in women with congenital heart disease. Circulation. 2006;113(4):
517–524.
3. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: a reports of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2008;118(23):e714–e833.
4. Bonow RO, Carabello BA, Chatterjee K, et al. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2008;118(15):e523–e661.
5. Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/
AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. Circulation. 2010;121:e266–e369.
6. Ammash N, Warnes CA. Cerebrovascular events in adult patients with cyanotic congenital heart disease. J Am Coll Cardiol. 1996;
28(3):768–772.
7. John AS, Gurley F, Schaff HV, et al. Cardiopulmonary bypass during pregnancy. Ann Thorac Surg. 2011;91(4):1191–
1196.
8. Sanikommu V, Lasorda D, Poornima I. Anatomical factors triggering platypnea-orthodeoxia in adults. Clin Cardiol. 2009;32(11):
e55–e57.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


