Chapter 45
Adult Congenital Heart Disease
1. Which patients with adult congenital heart disease require antibiotic prophylaxis?
 Unrepaired cyanotic heart disease
Unrepaired cyanotic heart disease
 Residual defects after repair with prosthetic material
Residual defects after repair with prosthetic material
 The first 6 months after repair with a device or prosthesis
The first 6 months after repair with a device or prosthesis
The new guidelines have also eliminated indications for prophylaxis for genitourinary (GU) or gastrointestinal (GI) procedures. (See also Chapter 33 on endocarditis and endocarditis prophylaxis).
2. What are the three main types of atrial septal defects (ASDs), and what are their associated anomalies?
The three main types of ASDs are secundum (70%), primum (20%), and sinus venosus (10%). The secundum ASD is a defect involving the floor of the fossa ovalis of the atrial septum. It usually presents as an isolated anomaly. The primum ASD is a defect at the base of the atrial septum adjacent to the atrioventricular valves. It is invariably part of an atrioventricular septal defect (endocardial cushion defect), and a cleft mitral valve is almost always present. The sinus venosus ASD is a defect of the posterior part of the septum, usually located in the superior part. In the majority of cases, a sinus venosus ASD is associated with anomalous connections or drainage of the right-sided pulmonary veins (Fig. 45-1).
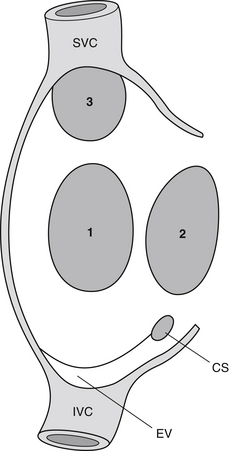
Figure 45-1 Atrial septal defects: 1, secundum; 2, primum; 3, sinus venosus. (Modified from Gatzoulis MA, Webb GD, Daubeney PEF, et al: Diagnosis and management of adult congenital heart disease, Edinburgh, 2003, Churchill Livingstone, p 163.) CS, Coronary sinus; EV, eustachian valve; SVC, superior vena cava; IVC, inferior vena cava.
3. When should an ASD be closed? Which ASDs cannot be closed by a percutaneous device?
4. List the four types of ventricular septal defects (VSDs).
Different classifications for VSDs have been used; one common approach divides VSDs into four types:
 Membranous or perimembranous VSDs involve the membranous ventricular septum, a small localized area of the normal ventricular septum that is fibrous. This is the most common type of VSD seen in the adult.
Membranous or perimembranous VSDs involve the membranous ventricular septum, a small localized area of the normal ventricular septum that is fibrous. This is the most common type of VSD seen in the adult.
 Muscular VSDs involve the trabecular portion of the septum.
Muscular VSDs involve the trabecular portion of the septum.
 Inlet VSDs involve the part of the ventricular septum that is adjacent to the tricuspid and mitral valves. Inlet VSDs are always associated with atrioventricular septal defects.
Inlet VSDs involve the part of the ventricular septum that is adjacent to the tricuspid and mitral valves. Inlet VSDs are always associated with atrioventricular septal defects.
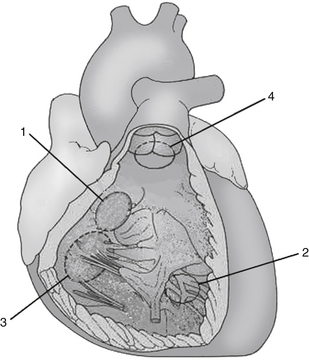
 Outlet VSDs (also known as supracristal VSD) involves the portion of the ventricular septum that is just below the aortic and pulmonary valve (Fig. 45-2).
Outlet VSDs (also known as supracristal VSD) involves the portion of the ventricular septum that is just below the aortic and pulmonary valve (Fig. 45-2).
5. What are the long-term complications of a small VSD in the adult patient?
6. What are the complications of a bicuspid aortic valve?
A bicuspid aortic valve is present in 0.5% to 1% of the population. The main complications are progressive aortic stenosis, aortic regurgitation, or a combination of both. Other complications include endocarditis and aortopathy. Although infrequent (<10%), aortic coarctation is also a well-described association and must be ruled out in these patients. Patients in whom the bicuspid valve demonstrates signs of valve degeneration on echocardiography are at an increased risk of cardiovascular events and need close regular follow-up.
7. How is hemodynamic severity of coarctation of the aorta assessed in the adult patient?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree