8.4 EVALUATION
8.4.1 History and Physical Examination
The history and physical examination should be detailed enough to establish the diagnosis of STEMI, but should also be concise in order to prevent unnecessary delay in reperfusion therapy (Table 8.1).
The chest discomfort associated with STEMI typically lasts more than 30 minutes, but may wax and wane if intermittent, spontaneous reperfusion occurs from endogenous fibrinolysis. It is typically substernal, but may originate in or radiate to the jaw, arm, neck, or epigastrum. A crushing pain, such as “an elephant sitting on my chest” is classic, but the discomfort may be more diffuse or milder, and confused with indigestion or heartburn. Associated symptoms may include nausea, vomiting, diaphoresis, fatigue, and dyspnea. Onset of symptoms is important: patients with pain which began >12–24 hours prior to hospital arrival that has subsequently subsided may no longer be candidates for emergent reperfusion therapy since the likelihood of substantial myocardial salvage is much less at that point.
Prior history of angina, myocardial infarction, percutaneous coronary intervention, coronary artery bypass surgery, or stress testing should be obtained. The patient should be questioned about risk factors such as hypertension, diabetes mellitus, hypercholesterolemia, family history of coronary disease, smoking, and cocaine use.
Severe tearing pain radiating to the back, especially in elderly or hypertensive patients, should raise the suspicion for aortic dissection. Other potential mimics of STEMI that should be considered include: acute pericarditis; coronary vasospasm; stress-induced cardiomyopathy (Takotsubo Syndrome); old infarction with left ventricular aneurism formation; and early repolarization.
Because therapy for STEMI includes antiplatelet, anticoagulant, and fibrinolytic agents, risk of bleeding should be evaluated. History of gastrointestinal bleeding, peptic ulcer disease, prior stroke, transient ischemic accident, intracranial hemorrhage, head trauma, or recent surgery should be obtained.
Table 8.1 Brief Initial Evaluation for Acute STEMI.
| History |
| Chest pain: time of onset, type, associated symptoms |
| History of MI, CVA, PCI, CABG |
| Risk factors for CAD |
| Bleeding risk |
| Contraindications to fibrinolysis |
| Physical exam |
| Airway, breathing, circulation Vital signs Evidence of CHF (JVD, rales, peripheral edema, cool extremities) Focal neurologic deficits |
| Electrocardiogram |
| ST elevation ≥ 0.1 mV in 2 contiguous leads Anterior (V1–V4) Lateral (V5–V6, I, aVL) Inferior (II, III, aVL) Right ventricular (V1, right-sided V4) True posterior (V7–V8, ST depression V1–V3) New or presumed new LBBB (obtain old ECG) Arrythmia |
| Laboratory analysis |
| Troponin, CK, CKMB CBC with platelets PT, PTT Electrolytes Creatinine Glucose Lipid panel B-hcg if women of child-bearing age Urine tox if suspect cocaine |
| Decide on strategy for reperfusion |
Physical examination should focus on patient stability (ABC: Airway, Breathing, Circulation), vital signs, jugular venous pressure elevation, murmers, rubs, gallops, rales, peripheral pulses, cool or edematous extremities, and focal neurologic defects.
8.4.2 Electrocardiogram
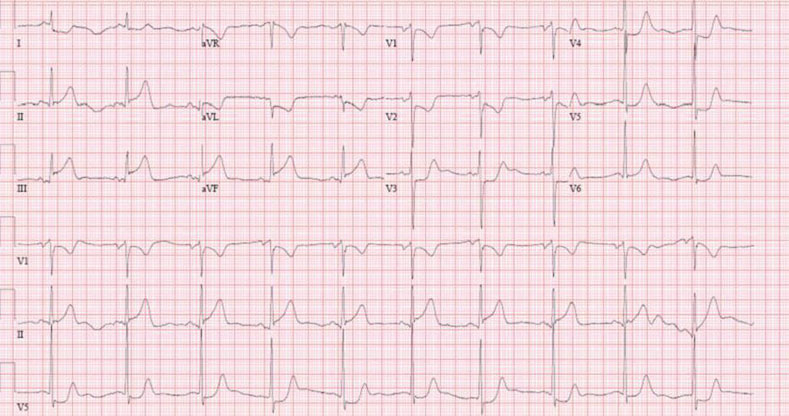
A 12-lead electrocardiogram (ECG) should be performed immediately in patients suspected of having an ACS because it helps determine the presence of STEMI and candidacy for reperfusion therapy. Patients with ST segment elevation of greater than 0.1 mV in at least two consecutive leads or a new or presumed new left bundle branch block (LBBB) are candidates for reperfusion therapy (Figure 8.1). It is important to note that within the first few minutes after symptom onset, the first ECG may not show ST segment elevation, but will show hyperacute (peaked) T waves. A repeat ECG is an invaluable tool in this setting. In patients with an inferior STEMI (Figure 8.2), a right sided ECG should be obtained to screen for right ventricular involvement, indicated by ST elevation in lead V4 on the right sided ECG. An ECG with deep ST depressions in V1–V4 accompanied by upright T waves and tall R waves in V1 and V2 may represent a true posterior infarction. In this situation, an echocardiogram or an ECG using posterior leads V7 and V8 may be helpful.
Figure 8.1 Electrocardiogram of acute anterolateral STEMI.
There are several other conditions which can cause ST elevation which must be distinguished from acute STEMI prior to implementation of reperfusion therapy (Table 8.2). Comparison to an old ECG is essential in this setting.
8.4.3 Laboratory Evaluation
Initial laboratory evaluation should include cardiac biomarkers (troponin, CK-MB, CK), CBC, PT, PTT, creatinine, electrolytes, glucose, and lipid panel. However, reperfusion therapy should not be delayed while awaiting the results of lab studies since it may take several hours for cardiac biomarkers to be elevated in the blood.
8.4.4 Other Diagnostic Studies
Chest radiography is indicated in all patients with STEMI, but should not delay reperfusion therapy. If, based on the clinical evaluation, aortic dissection becomes suspected a trans-esophageal echocardiogram or computed tomography (CT) scan should be obtained urgently prior to anticoagulation or reperfusion therapy. A surface echocardiogram may be useful in some settings if the diagnosis of STEMI is uncertain or to exclude mechanical complications (see Section 8.6 below).
Table 8.2 Differential Diagnosis of ST-Elevation on Clinical History and Electrocardiogram.
| Cause | Clues |
| Acute STEMI | Reciprocal changes, clinical history |
| Stress-induced cardiomyopathy (Takotsubo Syndrome) | Emotional stress, apical ballooning on echocardiogram or ventriculogram |
| Aortic dissection | Hypertension, tearing pain radiating to the back |
| Ventricular aneurism | Q-waves, absence of acute chest discomfort |
| Early repolarization | Most marked in V4, often with notched J point |
| Left ventricular hypertrophy | Concave |
| Left bundle branch block or ventricular paced rhythm | Discordant ST segment changes <5 mm from QRS direction |
| Acute pericarditis | Diffuse ST elevation and PR depression |
| Hyperkalemia | Tall, peaked T waves, loss of P wave amplitude, widened QRS |
| Pulmonary embolus | Sinus tachycardia, S1Q3T3, right bundle branch block |
| Brugada syndrome | rSR’ in V1 and V2 with down-sloping ST elevation |
8.5 TREATMENT
Treatment for STEMI can be divided into initial therapy, reperfusion therapy, antiplatelet and anticoagulant therapy, and post-reperfusion therapy (Table 8.3).
Table 8.3 Inpatient Management of STEIM.
| Initial management |
| O2, IV access, cardiac monitor |
| Aspirin 325 mg chewable PO or 300 mg PR |
| Morphine IV PRN |
| NTG SL PRN |
| Reperfusion therapy |
| PCI vs. lytics (see Figure 8.3) |
| Antiplatelet therapy |
| Aspirin |
| 325 mg chewable PO or 300 mg PR initially, then 81 mg PO daily indefinitely |
| Theinopyridine |
| Clopidogrel 300 mg PO initially, then 75 mg PO daily for 12 months Prasugrel 60 mg PO initially, then 10 mg PO daily for 12 months Caution if prior TIA or stroke, age >75 years, or weight <60 kg |