Chapter 27 Acute Respiratory Failure
Acute respiratory failure is the inability to maintain adequate gas exchange. It is defined by abnormalities of arterial oxygen (Pao2) and carbon dioxide (Paco2) tensions. Hypoxemia may occur with a normal or low Paco2 (type 1 respiratory failure) or with an elevated Paco2 (type 2 respiratory failure). Respiratory failure is commonly associated with respiratory distress, which manifests as tachypnea, dyspnea, and the use of the accessory muscles of breathing.
Respiratory failure is relatively common in cardiac surgery patients and has a wide variety of causes (Table 27-1). The need for prolonged ventilatory support (>72 hours) occurs in approximately 6% of patients undergoing coronary artery bypass graft surgery,1 and reintubation is required in approximately 3% of patients.2
Table 27-1 Common Causes of Postoperative Respiratory Failure Hypoxemia in Patients After Cardiac Surgery
| On Arrival in the ICU and During Mechanical Ventilation |
| Pulmonary edema |
| Atelectasis/lobar collapse |
| Endobronchial intubation |
| Pneumothorax |
| Hemothorax |
| Ventilator dysynchrony |
| Bronchospasm |
| Low SVO2 (low cardiac output,* anemia) |
| Immediately Following Extubation |
| Residual sedative or opioid drugs |
| Residual neuromuscular blockade |
| Atelectasis |
| Upper airway obstruction/edema |
| Late Deterioration in Respiratory Function |
| Cardiac tamponade (following removal of pacing wires) |
| Pneumothorax (following removal of chest drains) |
| Left ventricular dysfunction |
| Arrhythmias (particularly atrial fibrillation) |
| Atelectasis and lobar collapse |
| Sepsis (pneumonia, mediastinitis) |
| Pulmonary embolus |
| Pulmonary edema |
ICU, intensive care unit.
* Causes of low cardiac output in the early period after cardiac surgery include all conditions listed in Table 20-4 with the exception of low systemic vascular resistance.
This chapter is divided into three sections: (1) mechanisms of respiratory failure; (2) diagnosis and treatment of respiratory failure; (3) specific causes of respiratory failure. Only an overview of respiratory failure is provided here. The physiological mechanisms of respiratory failure are explored in greater detail in Chapter 1, and the ventilatory treatment is described in Chapters 28 and Chapter 29.
MECHANISMS OF RESPIRATORY FAILURE
Central Nervous System and Neuromuscular Dysfunction
Dysfunction of the CNS or neuromuscular system can lead to hypoventilation, loss of protective airway reflexes, and impaired swallowing. Hypoventilation causes hypercarbia and, if severe, hypoxemia. Impaired swallowing and loss of protective airway reflexes predispose a patient to pulmonary aspiration.
Exacerbating Factors
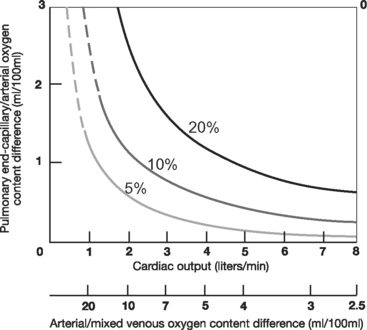
With normal lung function, the main determinant of Pao2 is alveolar oxygen tension (PAo2). However, with intrapulmonary shunting, systemic venous blood passes through the lungs without being oxygenated, and SVo2 becomes an important determinant of Pao2. Low SVo2 can arise from anemia, low cardiac output, and high metabolic rate. This is illustrated in Figure 27-1, which shows the relationship between cardiac output and arterial oxygenation at various levels of intrapulmonary shunting.
APPROACH TO PATIENTS WITH ACUTE RESPIRATORY DISTRESS
Diagnosis
Examination
If appropriate, a targeted neurologic assessment should be performed, focusing on level of consciousness (Glasgow coma scale), cough, gag reflex, and focal neurologic deficit (see Chapter 37).
Investigations
Blood Gas Analysis and Oximetry.
In addition to measurement of arterial oxygen saturation (Sao2), Pao2, and Paco2, useful information is obtained from (1) calculation of the alveolar-arterial (A-a) Po2 gradient, (2) measurement of Svo2, and (3) assessment of metabolic parameters (pH, bicarbonate, base excess, and lactate; see Chapters 1 and Chapter 31).
The A-a gradient is the difference between PAo2 and Pao2, where PAo2 is calculated from the alveolar air equation (see Equation 1-18). With healthy lungs breathing air, the A-a gradient is very low, less than 1 κPa (<7.5 mmHg). However, the A-a gradient is influenced by age and FIo2. At age 40, the upper limit of normal is about 3 κPa (23 mmHg), increasing to 5 κPa (38 mmHg) at age 80 (when breathing room air). To this must be added 0.75 to 1 κPa (6 to 7.6 mmHg) for every 10% increase in FIo2. Within these limitations, the A-a gradient can be used to differentiate hypoventilation (normal A-a gradient) from intrapulmonary shunting (elevated A-a gradient).
Chest Radiography.
The chest radiograph (see Chapter 6) is essential in the assessment of respiratory failure. If possible, the film should be obtained while the patient is erect because this position improves the diagnostic yield, particularly in terms of pleural collections and pneumothoraces. In a patient with respiratory failure, a normal chest radiograph is consistent with the diagnoses of hypoventilation, microatelectasis, low SVo2, and shunting across a PFO.
Hemodynamic Monitoring and Echocardiography.
Hemodynamic evaluation (see Chapter 8) is an integral part of the assessment of respiratory failure. A PAC allows for quantification of cardiac output, SVo2, and pulmonary artery wedge pressure (PAWP). PAWP helps to determine the cause of pulmonary edema (see subsequent material). Echocardiography (see Chapter 7) reliably identifies the cause of low cardiac output (see Chapter 20) and can be used to identify a PFO.
Treatment
Treatment of acute respiratory failure is both supportive and specific to the underlying condition. Specific treatments are discussed in specific causes of respiratory failure. Supportive treatments are listed subsequently. The treatment goals are outlined in Table 27-2.
Table 27-2 Therapeutic Aims for Managing Acute Respiratory Failure
| SaO2 ≥ 90% (approximately 7 kPa or 55 mmHg) |
| pH >7.25 |
| Respiratory rate <30 to 35/min* |
| Ability to speak in short sentences |
| Hemodynamic stability |
| Ability to protect airway† |
* Higher respiratory rates cannot usually be sustained indefinitely; exhaustion and respiratory arrest are likely to supervene.
† Respiratory failure severe enough to cause a fall in the level of consciousness such that the patient cannot obey commands mandates endotracheal intubation to protect against pulmonary aspiration.
Supplemental Oxygen
All patients who are hypoxemic (Pao2 <8 to 10 κPa or 60 to 75 mmHg) should receive supplemental oxygen by nasal cannula or face mask. This includes patients with COPD (see subsequent material). Oxygen is very effective in treating hypoxemia due to hypoventilation but is less effective when it is due to V/Q mismatch. Supplemental oxygen may mask severe hypoventilation, emphasizing the importance of monitoring respiratory rate, level of consciousness, and Paco2 (or end-tidal CO2) in addition to Spo2. Oxygen therapy is discussed further in Chapter 28.
Positive Pressure Ventilation
Positive pressure ventilation is used to improve gas exchange and reduce the work of breathing. It may be invasive (see Chapter 29) or noninvasive (see Chapter 28).
The need for ventilatory support depends on the severity of the respiratory failure, the rate of deterioration, the underlying disease process, and the need to protect the airway. When respiratory failure develops rapidly or occurs in the context of multiple organ dysfunction syndrome, early institution of invasive ventilation is indicated. However, if respiratory failure develops slowly and is not associated with severe metabolic derangement or other organ failure, urgent intubation may not be required, and other targeted therapy (e.g., antibiotics, physical therapy, diuretics) may be tried first. The signs of severe respiratory failure that, if not rapidly corrected, indicate the need for urgent intubation and ventilation are listed in Table 27-3.
Table 27-3 Features of Severe Respiratory Failure That Indicate the Need for Urgent Endotracheal Intubation
| Respiratory System |
| SaO2 ≤ 85% (approximately 6.5 kPa or 50 mmHg) with high-flow face-mask oxygen or an FIO2 ≥ 0.6 with noninvasive ventilation |
| Rising PaCo2* with respiratory acidemia (pH < 7.1) |
| Respiratory distress: respiratory rate >40/min, intercostal in-drawing, use of accessory muscles, the inability to speak more than one or two words between breaths |
| Cardiovascular System |
| Heart rate >120 beats/min |
| Falling blood pressure or cardiac output or escalating inotrope requirements |
| Increasing lactic acidosis |
| Central Nervous System |
| Confusion and agitation |