Abdominal Vasculature
I. ABDOMINAL AORTA
A.
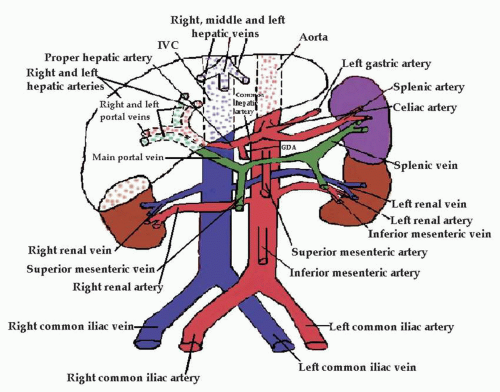
Anatomy (Fig. 2.1)
1. Abdominal aorta extends from the twelfth thoracic vertebra to the fourth lumbar vertebra.
2. Portions of the Abdominal Aorta (Fig. 2.2):
a. Proximal—superior to or at the level of the celiac axis, measures 2 to 3 cm
b. Middle—below the celiac axis, above the renal arteries, measures 1.6 to 2.5 cm
c. Distal—just above the bifurcation, measures 1.1 to 2.0 cm
d. Iliac arteries—measure 0.6 to 1.4 cm
3. Main branches off the aorta:
a. Celiac axis or celiac artery: first branch off the abdominal aorta, divides into the left gastric artery, splenic artery, and common hepatic artery. These feed the stomach, spleen, liver, pancreas, and duodenum.
b. The superior mesenteric artery is approximately 1 cm distal to the celiac axis. This artery feeds the small intestine, ascending colon, cecum, and part of the transverse colon.
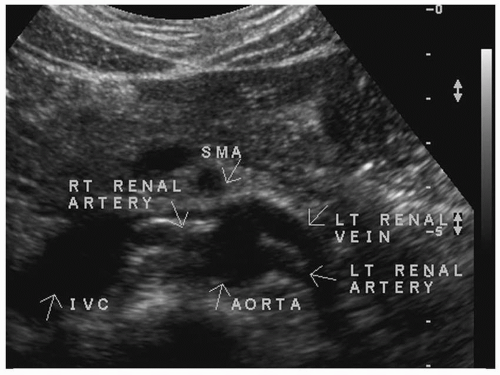
c. The renal arteries are the next branches. They supply the kidneys, ureters, and adrenal glands (Fig. 2.3).
d. The inferior mesenteric artery is approximately 3 to 4 cm above the aortic bifurcation. It supplies the descending, iliac, and sigmoid colon, as well as the left half of the transverse colon and part of the rectum.
e. The common iliac arteries are the terminal branches of the abdominal aorta. They divide into the internal iliac arteries and the external iliac arteries.
4. Other branches off the abdominal aorta but not commonly seen on ultrasound are:
a. The paired inferior diaphragmatic or inferior phrenic arteries.
b. The paired middle suprarenal arteries.
c. The paired gonadal arteries.
d. The paired first to fourth lumbar arteries.
e. The middle sacral artery.
5. Above the umbilicus, all paired arteries course posterior to their related vein. Below the umbilicus, all paired arteries course anterior to their related vein.
B. Pathology
1. Ectasia—when the abdominal aorta does not taper as it normally does, but is not dilated to the point of aneurysm.
2. Atherosclerosis or arteriosclerosis—thickening, hardening, and deposition of plaque in the intimal wall of arteries, which can cause stenosis.
a. This is associated with smoking, hypertension, sedentary lifestyle, diabetes mellitus, and increased levels of low-density lipoprotein (LDL) levels of cholesterol.
b. Because of its large size and high flow rate, the abdominal aorta is sensitive to plaque. Two common sites of plaque formation are the origin of the renal arteries and the bifurcation into the common iliac arteries. The most common site is the infrarenal portion of the aorta.
c. More men than women are affected with atherosclerosis, and the incidence increases with age.
d. Atherosclerosis may be associated with aneurysm and wall weakening.
3. Coarctation is the narrowing of the aorta. There are two clinical findings associated with this:
a. Hypertension resulting from decreased kidney perfusion.
b. Manifestation of lower extremity ischemia decreased lower extremity pulses.
4. Aneurysm—increase in arterial diameter (Fig. 2.4).
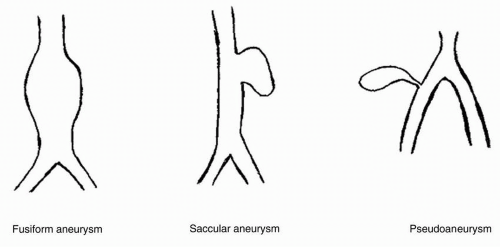
a. Types of aneurysms (Fig. 2.5):
(1) Fusiform—symmetric swelling, most common, usually found below the level of the renal arteries (90% of all aneurysms) and may extend into the common iliac arteries. These also may contain thrombus.
(2) Saccular—focal outpouching, least common, usually affects the left lateral portion of the distal abdominal aorta (where the least support is), causes marked alteration in the pattern of blood flow. These also may have thrombus or plaque.
(3) Dissecting—tear in intimal lining of the wall of the vessel. A false lumen is created between the
intima and the media. These may extend from the aortic valve to the abdominal aorta. They can be very dangerous. Blood flow may push the flap across the lumen and completely (or almost completely) obstruct flow. Two flow lumens with markedly different flow characteristics would be seen. These are most common in the thoracic aorta (Fig. 2.6).
intima and the media. These may extend from the aortic valve to the abdominal aorta. They can be very dangerous. Blood flow may push the flap across the lumen and completely (or almost completely) obstruct flow. Two flow lumens with markedly different flow characteristics would be seen. These are most common in the thoracic aorta (Fig. 2.6).
(4) Pseudoaneurysms or false aneurysms. Small pocket of moving blood connected to an artery through a small opening or neck and may be partly surrounded by thrombus. These form due to interventional radiology procedures (e.g., cardiac catheterization using the common femoral artery), trauma, surgery, or infection. They can be felt as a pulsatile mass. A turbulent flow pattern
would be visualized. Compression with a transducer may clot them off. An alternative therapy would be thrombin injection.
would be visualized. Compression with a transducer may clot them off. An alternative therapy would be thrombin injection.
b. Abdominal aortic aneurysm is considered if the diameter is greater than 3 cm or greater than 50% than the original diameter.
c. A true aneurysm contains all the layers of the artery (fusiform and saccular.) A false aneurysm or pseudoaneurysm leaks through a hole in the intima but is contained by the external layer or by the body.
d. There is an increased risk for abdominal aortic aneurysm in close relatives.
e. The incidence of the disease is highest among men, particularly those over 65 years of age.
f. The identification of an abdominal aortic aneurysm increases the risk for aneurysms in the common iliac arteries, common femoral arteries, and popliteal arteries.
g. Only 4% of abdominal aortic aneurysms actually affect flow into the renal arteries. Stenosis of the renal arteries and hydronephrosis are potential complications of abdominal aortic aneurysms.
h. Aneurysms over 6 cm in diameter are considered surgical emergencies, and 60% of all aneurysms over 7 cm will rupture within 1 year. Abdominal aortic aneurysms can have small tears and leak into the body cavity.
i. The main complication of abdominal aortic aneurysm is rupture; the main complication of peripheral aneurysm is distal embolization.
j. Atherosclerotic abdominal aortic aneurysms may become inflammatory, and the wall will become thickened and surrounded by fibrosis.
k. Marfan syndrome is associated with weakness of the arterial wall and may result in aneurysm of the first portion of the aorta leading up to the aortic valve. This may lead to dissection of this portion of the aorta.
l. To repair an aneurysm, the surgeon may put a graft in. The native aorta is usually wrapped around the graft. Fluid can accumulate between the graft and the vessel wall. Types of aortic grafts are as follows:
(1) Aortic end-to-end graft (wrapped in native aorta)
(2) Aortoiliac graft
(3) Aorto-bifemoral graft
C. History: Questions to Ask the Patient
1. Do you have abdominal pain? (May be deep and penetrating, mainly in the back). Aortic rupture causes severe pain.
2. Do you have a pulsing sensation in your abdomen? (Most of the time a thoracic aneurysm will not be considered. However, if this is a consideration or if on early views of the aorta one sees a suggestion of extension from the thoracic area, then ask the next question).
3. Do you have high back pain, a cough, wheezing, hoarseness, or difficulty swallowing?
D. Diagnostic Examination
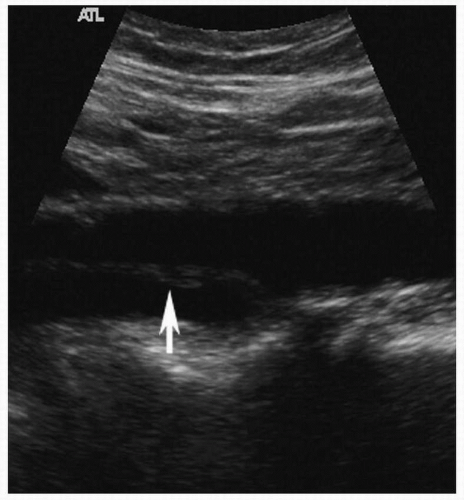
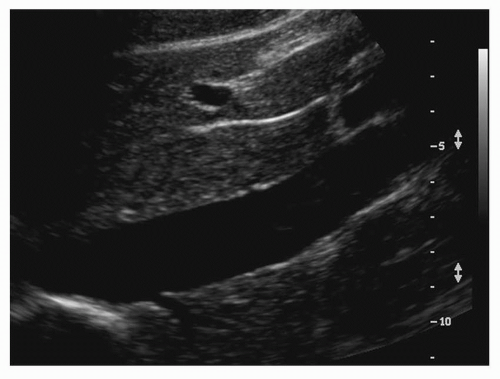
1. Begin with the patient in the supine position, although a decubitus position can be helpful to evaluate the bifurcation.
2. Using a 3.5- or 5-MHz curved-array transducer, place the transducer in a sagittal plane at the midline of the body, just inferior to the xiphoid process of the sternum. Slightly move or angle the transducer to the left and locate the proximal aorta. Slowly move inferiorly, using a rock-and-slide motion.
3. Repeat in the transverse plane.
4. Measure anteroposterior and transverse dimensions of the aorta, outside wall to outside wall.
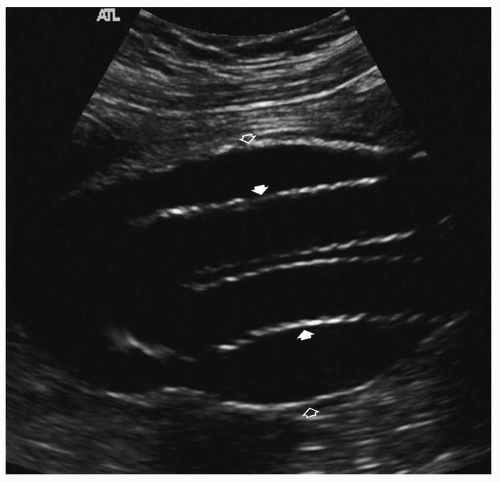 FIGURE 2.7. Sagittal view of a bifurcated endograft (closed arrows) within dilated aortic lumen (open arrows). (Image courtesy of Philips Medical Systems.) |
5. Take sagittal and transverse images of the following structures with and without calipers:
a. Proximal aorta (inferior to the diaphragm and superior to the celiac trunk).
b. Mid aorta (inferior to the celiac trunk and along the length of the superior mesenteric artery).
c. Distal aorta (inferior to the superior mesenteric artery and superior to the bifurcation).
d. Right and left common iliac arteries.
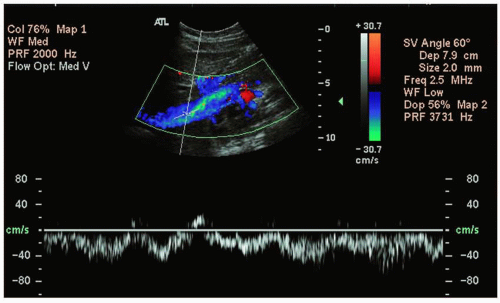
e. Color images and Doppler waveforms may be taken if necessary.
f. If evaluating an endovascular stent graft, take gray-scale images in both planes, and color images and Doppler waveforms through the native aorta, entire graft, and outflow iliac vessels. Assess the entire residual aneurysm sac as well. Evaluate potential sites for endoleaks, such as the attachment sites of the graft or branches related to the lumbar artery and inferior mesenteric artery (Fig. 2.7).
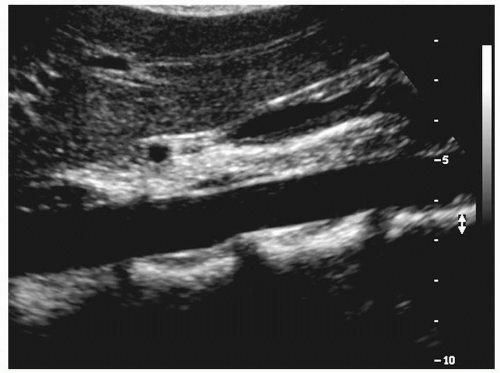
6. Distinguishing the aorta from the inferior vena cava (IVC) on ultrasound:
a. The aorta never touches the liver; the IVC does.
b. The aorta has thicker walls (thicker tunica media).
c. The aorta has cardiac pulsatility; the IVC changes with respiration.
d. The aorta tapers from superior to inferior; the IVC has a “hammock” shape.
e. The aorta and IVC have different Doppler signals.
f. The aorta has multiple anterior branches, while the only branches from the IVC are the hepatic veins.
g. The right renal artery is seen posterior to the IVC; no vessels course posterior to the aorta.
E. Diagnostic Analysis
Analysis of the abdominal aorta would include the following:
1. The maximum true anteroposterior, length, and transverse dimensions.
2. Documentation of the location of an aneurysm, and of whether the renal arteries or iliac arteries are involved.
3. Notation of wall thickening in terms of what type and how extensive it is.
4. Evaluation for dissection. This appears as a thin membrane “fluttering” in the lumen. Doppler shows different signals in each of the channels.
5. Examination of both kidneys for signs of hydronephrosis or renal artery stenosis.
6. Verification that normal triphasic or biphasic waveforms that are high resistance are seen with Doppler.
7. An endoleak associated with an endovascular stent graft has a distinctly different Doppler signal than from that of the endograft. There should be no flow leaking out around the graft, inside or outside of the residual aneurysm sac.
F. Other Diagnostic Tests
1. Aortic angiography
2. Magnetic resonance angiography (MRA)
3. Computed tomographic angiography (CTA).
II. INFERIOR VENA CAVA
A. Anatomy
(Fig. 2.8)
1. Originates from the paired common iliac veins at fifth lumbar vertebra.
2. Lies to the right of the aorta.
3. The size is generally less than 3.5 cm during full inspiration.
4. The main branches include the hepatic veins, renal veins, and the common iliac veins.
5. The right and left renal veins enter the IVC laterally, coursing anterior to the renal arteries. The left renal vein is longer, and courses anterior to the aorta and posterior to the superior mesenteric artery (SMA).
6. The right gonadal and fourth lumbar vein also enters the IVC. (The left gonadal vein enters the left renal vein.)
7. The tunica media of the IVC is very thin and elastic.
8. There are no valves in the IVC. There are also no valves in the external and common iliac veins, hepatic, renal, lumbar, gonadal, and soleal sinuses.
9. During inspiration, the intrathoracic pressure decreases and the intraabdominal pressure increases. Blood moves from the abdomen into the chest with decreased outflow from the peripheral veins, and flow in the legs should decrease or stop. Inflow is allowed from upper extremities. During expiration, vice versa. Outflow increases from the lower extremity veins.
10. Hydrostatic pressure is pressure due to gravity—when the patient is supine, hydrostatic pressure is negligible (0-15 mm Hg). When the patient is erect, hydrostatic pressure may be 102 mm Hg depending on his or her height.
B. Pathology
1. Enlargement of the IVC. A faulty tricuspid valve that allows blood to reflux through the right atrium into the IVC causes the size of the IVC to be large (>3.5 cm). Color flow shows reversal—blue then red then blue again pattern.
2. Thrombus in the IVC may lead to localized swelling and noncollapse of the IVC during exhalation.
3. Tumors may invade the IVC, especially from the right kidney through the right renal vein. These metastasize from lymphoma, hepatocellular carcinoma, renal cell carcinoma, and breast carcinoma. Primary tumors are rare. Leiomyosarcoma of the IVC wall is the most common type of mural tumor in the venous system.
4. Budd-Chiari syndrome—thrombus in hepatic veins prevents blood from draining from the liver to the IVC.
5. Congenital abnormalities may include the hepatic veins draining directly into the right atrium.
6. IVC rupture usually occurs after trauma or surgery.
7. Greenfield filter (or other filter) — placed in the IVC near the confluence of the renal veins or iliac veins. This keeps the thrombus from coursing through the IVC, heart, and pulmonary vessels. A surgical clip can also be placed in the IVC to decrease the risk for pulmonary embolism.
C. History: Questions to Ask the Patient.
Symptoms may be nonspecific. Primary vena cava tumors are rare, and symptoms are likely to be due to secondary involvement or compression of the IVC. There may be secondary renal related symptoms. Ask the following questions:
1. Do you have leg swelling or edema?
2. Do you have any known kidney disease?
D. Diagnostic Examination
1. Begin with the patient in the supine position, although a slight reverse Trendelenburg position can pool blood in the IVC. A decubitus position can also be helpful.
2. Using a 3.5- or 5-MHz curved-array transducer, place the transducer in the sagittal plane at the midline of the body, just inferior to the xiphoid process of the sternum. Slightly move or angle the transducer to the right and locate the IVC. [See “Distinguishing the Aorta from the IVC” (Section I.D.2.) for different sonographic characteristics between the two.] Slowly move inferiorly, using a rock-and-slide motion.
3. Repeat in the transverse plane.
4. Take sagittal and transverse images of the following structures:
a. Distal IVC to include the diaphragm and hepatic veins
b. Mid-IVC at the level of the head of the pancreas
c. Proximal IVC
d. Bifurcation of the right and left common iliac veins
E. Diagnostic Analysis
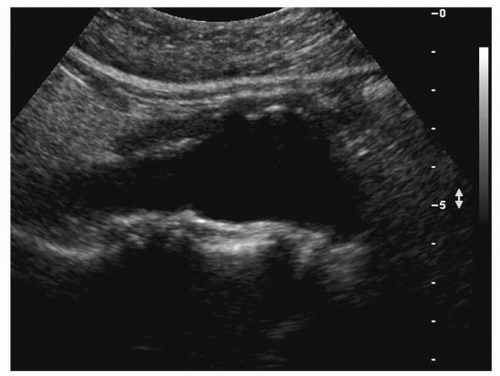
1. The IVC transmits both respiratory and cardiac pulsations, which becomes more noticeable the closer you are to the heart. The pattern of the Doppler tracing has been described as a “saw-tooth” tracing (Fig. 2.9).
2. With deep inspiration, the IVC dilates. With deep expiration, the IVC diameter decreases. By doing a Valsalva maneuver, the flow is temporarily suspended.
3. Evaluate the lumen for thrombus, tumor, or slowflowing blood. Slow-flowing blood appears more echogenic and moves in a swirling pattern. Slow-flowing blood is seen with fluid overload, right heart failure, and inferior to an obstruction.
F. Other Diagnostic Tests
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree