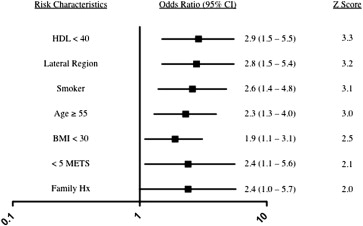
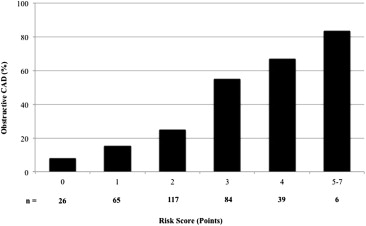
Women with angina pectoris and abnormal stress test findings commonly have no epicardial coronary artery disease (CAD) at catheterization. The aim of the present study was to develop a risk score to predict obstructive CAD in such patients. Data were analyzed from 337 consecutive women with angina pectoris and abnormal stress test findings who underwent cardiac catheterization at our center from 2003 to 2007. Forward selection multivariate logistic regression analysis was used to identify the independent predictors of CAD, defined by ≥50% diameter stenosis in ≥1 epicardial coronary artery. The independent predictors included age ≥55 years (odds ratio 2.3, 95% confidence interval 1.3 to 4.0), body mass index <30 kg/m 2 (odds ratio 1.9, 95% confidence interval 1.1 to 3.1), smoking (odds ratio 2.6, 95% confidence interval 1.4 to 4.8), low high-density lipoprotein cholesterol (odds ratio 2.9, 95% confidence interval 1.5 to 5.5), family history of premature CAD (odds ratio 2.4, 95% confidence interval 1.0 to 5.7), lateral abnormality on stress imaging (odds ratio 2.8, 95% confidence interval 1.5 to 5.5), and exercise capacity <5 metabolic equivalents (odds ratio 2.4, 95% confidence interval 1.1 to 5.6). Assigning each variable 1 point summed to constitute a risk score, a graded association between the score and prevalent CAD (p trend <0.001). The risk score demonstrated good discrimination with a cross-validated c-statistic of 0.745 (95% confidence interval 0.70 to 0.79), and an optimized cutpoint of a score of ≤2 included 62% of the subjects and had a negative predictive value of 80%. In conclusion, a simple clinical risk score of 7 characteristics can help differentiate those more or less likely to have CAD among women with angina pectoris and abnormal stress test findings. This tool, if validated, could help to guide testing strategies in women with angina pectoris.
At present, no simple techniques are available to help physicians identify women with angina pectoris who are more or less likely to have obstructive coronary artery disease (CAD) before referral for coronary angiography. Previous studies, largely performed >2 decades ago, that incorporated stress testing and clinical data to predict obstructive CAD were limited by including predominantly men and focusing just on exercise treadmill testing, rather than including stress imaging data. Therefore, we sought to determine the clinical factors associated with obstructive CAD in women with angina pectoris and abnormal stress test findings using data from consecutive women referred for coronary angiography in a large, urban teaching hospital during a 4-year period. We then devised a risk score that identifies women with a lower risk of obstructive CAD.
Methods
The present study was a retrospective cohort study analyzing the medical records of 337 consecutive women who had undergone coronary angiography for documented angina pectoris and abnormal stress test findings from 2003 to 2007 at Parkland Memorial Hospital, a large, urban, county teaching hospital. The institutional review board of the University of Texas Southwestern Medical Center at Dallas approved the study protocol. All women during the study period who underwent coronary angiography and who also had preceding abnormal stress test findings were identified (n = 445). The stress testing modalities consisted of either exercise or pharmacologic stress, with electrocardiographic, echocardiographic, or nuclear detection. Women were excluded from the present study if they had a known clinical history of CAD before angiography or if they had undergone cardiac catheterization for acute coronary syndrome or for an evaluation of cardiomyopathy, congestive heart failure, valvular heart disease, or congenital heart disease (n = 108), leaving a final sample size of 337 subjects.
Patient charts, electronic databases, and coronary angiograms were reviewed to abstract data on numerous clinical and laboratory variables (detailed in the next paragraphs). The electrocardiographic and stress testing components were also evaluated. Data were collected on the types of stress testing completed, exercise tolerance test characteristics (exercise capacity and symptoms developed during stress), and imaging stress test characteristics (regionality and reversibility).
Race/ethnicity was previously defined by healthcare provider documentation. The body mass index (BMI) was assessed during the preprocedural physical examination. Prevalent clinical diagnoses such as hypertension, diabetes mellitus, and lipid derangement were ascertained by a previous chart diagnosis or medication use (i.e., antihypertensive agents, glucose-lowering agents, statins). Additionally, patients with systolic blood pressure ≥140 mm Hg, fasting glucose >125 mg/dl or hemoglobin A1c >6.5%, or high-density lipoprotein (HDL) cholesterol <40 mg/dl were diagnosed as having hypertension, diabetes mellitus, or low HDL cholesterol, respectively. Smoking history was classified as current smoker, past smoker (cessation for ≥6 months), or never smoked. A family history of premature CAD was defined as those with first-degree relatives who had had CAD before 55 years old for male relatives or 65 years old for female relatives. Psychiatric history (depression, anxiety disorder, bipolar disorder) and chronic pain syndrome were determined from chart diagnoses or mental health/pain clinic visits. Postmenopausal state was identified by chart diagnoses or by previous oopherectomy. Substance abuse was ascertained by chart diagnosis or urine toxicology screening. The Framingham risk score (FRS) was derived from these covariates using the National Cholesterol Education Program version of the score.
A positive exercise tolerance test was defined as having >1 mm horizontal or down-sloping ST-segment depressions in ≥1 leads. Positive myocardial perfusion imaging study findings were defined by >1 segment of reversible perfusion defect. Positive stress echocardiographic findings was defined as new or worsening inducible wall motion abnormality at peak stress. Exercise capacity was evaluated only in those who underwent treadmill protocols and was categorized as those achieving ≥5 or <5 metabolic equivalents (METs). Obstructive CAD was defined as ≥50% stenosis in ≥1 epicardial coronary artery determined by coronary angiography.
Univariate analyses (Wilcoxon rank sum test for continuous variables and chi-square test for categorical variables) were used to evaluate differences in characteristics between those with and those without obstructive CAD. Using a threshold of p = 0.05, variables achieving crude statistical significance were entered into a forward stepwise multivariate logistic regression model to identify variables independently associated with obstructive CAD. Not all subjects had complete data sets because a proportion of patients did not undergo imaging stress tests to assess regions of ischemia (n = 147) and a proportion did not undergo exercise stress testing to assess for functional capacity (n = 308). These variables and other missing data were assigned the null category for the multivariate models, as a conservative approach that would bias toward the null. Covariates with p <0.05 remaining in the final regression model were assigned 1 point, with the points summed to derive an integer score. Continuous variables were dichotomized according to usual clinical cutpoints (30 kg/m 2 for BMI, 5 METs) or median values in the cohort (55 years for age) for the purposes of creating the score. The area under the receiver operating characteristics curve for the integer score was determined by calculating the c-statistic in logistic regression analyses with obstructive CAD as the dependent variable and the integer score as the independent variable. The 95% confidence limits of this c-statistic were generated by bootstrapping techniques using 100 replications of this model. The optimized threshold value of the score was determined by calculating the sensitivity, specificity, positive predictive value, and the negative predictive value for each level of the score. Analyses were performed using STATA, version 10.1 (StataCorp, College Station, Texas).
Results
Of the 337 women referred for invasive coronary angiography for angina pectoris and abnormal stress test findings, 65% (n = 219) had no obstructive CAD. The clinical characteristics of the study population are listed in Table 1 . A patient could have undergone 1 or multiple stress testing modalities, and a total of 444 tests were administered in these 337 women. Most patients underwent nuclear stress testing (44%), with fewer undergoing exercise treadmill testing (33%) or stress echocardiography (23%). Exercise was used as a stress modality for 31% of the patients. An imaging modality, compared to electrocardiograms, was used in 67%. The stress testing characteristics of the study population are listed in Table 2 .
| Characteristic | Obstructive (n = 118) | Nonobstructive (n = 219) | p Value |
|---|---|---|---|
| Age (yrs) | 59 ± 8.9 | 55 ± 9.2 | <.001 |
| Race | .27 | ||
| White | 27 (33%) | 33 (15%) | |
| Black | 55 (47%) | 107 (49%) | |
| Hispanic | 26 (22%) | 65 (30%) | |
| South Asian | 4 (3%) | 4 (2%) | |
| Other | 6 (5%) | 10 (5%) | |
| Body mass index (kg/m 2 ) | 31 ± 6.3 | 35 ± 8.5 | <.001 |
| Diabetes mellitus | 75 (64%) | 99 (45%) | .001 |
| Hypertension | 110 (93%) | 192 (88%) | .11 |
| Low high-density lipoprotein | 101 (86%) | 138 (63%) | <.001 |
| Smoker | 61 (52%) | 68 (31%) | <.001 |
| Premature family history | 15 (13%) | 13 (6%) | .03 |
| Menopausal | 21 (18%) | 41 (19%) | .83 |
| Depression | 28 (24%) | 52 (24%) | 1.00 |
| Anxiety | 7 (6%) | 24 (11%) | .13 |
| Bipolar | 2 (2%) | 9 (4%) | .23 |
| Chronic pain | 10 (8%) | 26 (12%) | .34 |
| Substance abuse | 10 (8%) | 9 (4%) | .10 |
| Characteristic | Obstructive (n = 118) | Nonobstructive (n = 219) | p Value |
|---|---|---|---|
| Positive tests | |||
| Exercise tolerance test | 37 (31%) | 74 (34%) | .65 |
| Nuclear | 70 (59%) | 108 (49%) | .08 |
| Echocardiography | 33 (28%) | 57 (26%) | .70 |
| Low exercise capacity | 16 (14%) | 12 (5%) | .01 |
| Reversibility | |||
| Inferior | 44 (37%) | 74 (34%) | .52 |
| Anterior | 47 (40%) | 69 (31%) | .13 |
| Lateral | 32 (27%) | 24 (11%) | <.001 |
| Apical | 41 (35%) | 46 (21%) | .01 |
| Other | 26 (22%) | 42 (19%) | .53 |
On multivariate analysis, older age (≥55 years), current smoking, nonobese BMI (<30 kg/m 2 ), low HDL cholesterol, premature family history of CAD, low exercise capacity (<5 METs), and lateral wall stress imaging abnormality results were independently associated with obstructive CAD ( Figure 1 ). No subject had all 7 of these factors, and only 6 (1.7%) had ≥5 ( Figure 2 ).