More than 1/4 of patients who undergo invasive coronary angiography are found to have no visible or nonobstructive (<50% stenosis) coronary artery disease (CAD). With the rapid evolution of noninvasive imaging for CAD diagnosis, avoiding invasive coronary angiography in patients unlikely to require coronary revascularization is desirable. We undertook to develop a clinical prediction tool to identify patients with a low likelihood of obstructive (≥50% stenosis) CAD. The derivation cohort included 24,637 patients with a diagnosis of “stable angina” or “acute coronary syndrome” referred for first cardiac catheterization in the province of British Columbia, Canada. The model was validated using an external dataset from the province of Alberta and comprised 18,606 patients. Seven variables (female gender, age <50 years, atypical Canadian Cardiovascular Society angina class, absence of ST-segment change on electrocardiogram, lifelong nonsmoking, and absence of diabetes and hyperlipidemia) were associated with the angiographic finding of “no or nonobstructive CAD.” The c-statistics for the derivation model were 0.76 and 0.74 using the validation dataset. In conclusion, this simple clinical prediction tool, applied to patients for whom determination of coronary anatomy was clinically indicated, identifies patients who have a low likelihood of obstructive CAD. The patient population identified by this tool may represent a population best suited to a noninvasive diagnostic strategy.
Invasive coronary angiography (ICA) remains the clinical “gold standard” for defining coronary anatomy. Despite broad application, ICA has limitations and exposes patients to a low, but not insignificant, risk of a major complication (<1%). Minor complications are more common with local vascular adverse events occurring in up to 9% of cases. Recent data from the American College of Cardiology National Cardiovascular Data Registry have shown that 39.2% of subjects referred for elective ICA have coronary arteries with <20% luminal narrowing and 62.4% have normal or “nonobstructive” coronary artery disease (CAD). Improved strategies for risk stratification have been called for to increase the diagnostic yield of ICA. Once objective information on coronary anatomy is deemed clinically necessary, identification of patients unlikely to have obstructive CAD (and thus not require revascularization) is of value. Our goal was to develop a clinical prediction tool to identify patients with a low likelihood of having obstructive CAD on invasive coronary angiogram.
Methods
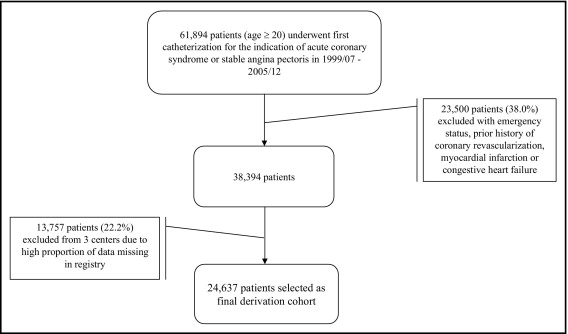
All adult patients (≥20 years of age) who underwent an index ICA for the indication of possible or presumptive stable angina pectoris or acute coronary syndrome, including unstable angina, non–ST-elevation myocardial infarction, and ST-elevation myocardial infarction, in the province of British Columbia, Canada, from July 1, 1999 to December 31, 2005 were eligible for the derivation cohort. The cohort was identified from the Cardiac Services British Columbia Registry, which prospectively captures demographic, procedural, and clinical information on all invasive coronary angiographic procedures performed in the province. Determination of extent of CAD was made at the conclusion of each case by the angiographer. Procedures were performed at the 6 centers in the province with diagnostic invasive coronary angiographic capabilities. In 3 centers, electrocardiographic data were not reliably entered into the Cardiac Services British Columbia Registry database, and data from these 3 centers was therefore excluded. Patients with previous heart failure, myocardial infarction, percutaneous coronary intervention, coronary artery bypass grafting, and current “emergency status” (patients judged to require immediate ICA) were excluded. The intent was to examine a symptomatic adult population without known CAD in whom invasive angiography had been requested by the referring physician to define CAD status. Patients requiring immediate ICA (emergency status), including acute ST-elevation myocardial infarction and the minority with presumed non–ST-elevation myocardial infarction or unstable angina with ongoing ischemic pain or hemodynamic instability, were judged to be inappropriate for initial noninvasive diagnostic strategies and were excluded. After exclusion, the total number of patients in the derivation cohort was 24,637 ( Figure 1 ). These patients were used to build the predictive model.
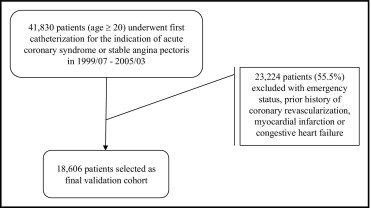
The model was validated through a second study cohort (“validation cohort”). The validation cohort included all patients who underwent an index ICA for the indication of possible or presumptive stable angina or acute coronary syndrome in the province of Alberta, Canada, from July 1, 1999 to March 31, 2005. The validation cohort was identified from the Alberta Provincial Project for Outcomes Assessment in Coronary Heart Disease database, which prospectively captures information on all cardiac catheterization procedures performed in the province of Alberta. Identical exclusion criteria as applied to the derivation cohort were applied to the validation cohort, and after exclusion, 18,606 patients comprised the validation cohort ( Figure 2 ).
The Cardiac Services British Columbia Registry and Alberta Provincial Project for Outcomes Assessment in Coronary Heart Disease databases categorize extent of CAD based on visual assessment. Angiographers code lesion severity in increments of 10% to 100% (total) occlusion. Angiographically normal infers a complete absence of angiographically evident disease and is coded as “angiographically normal.” For this analysis, nonobstructive CAD was defined as “disease present but luminal narrowing <50%.” Obstructive CAD was defined as “disease ≥50% in ≥1 epicardial coronary artery.” The intent of this work was to identify a patient subset with a low likelihood of obstructive CAD and thus those with angiographically normal and nonobstructive CAD were combined and represented by the term “absence of obstructive CAD.” Due to the limitation of visually distinguishing between truly normal and nonobstructive CAD on invasive coronary angiogram and the commonality of neither group requiring revascularization, it was judged appropriate to combine these groups.
Index catheterization was defined as the first invasive coronary angiographic procedure for the patient. Electrocardiography performed at the time of ICA in patients with stable angina and the most markedly abnormal electrocardiogram recorded for patients with acute coronary syndrome defined electrocardiographic status. Electrocardiographic status was graded into 1 of 5 categories (from least to most abnormal)—no ST-segment change, ambiguous ST-segment change, T-wave inversion, ST-segment depression, and ST-segment elevation. Angina pectoris was defined according to the Canadian Cardiovascular Society (CCS) classification system. Diabetes mellitus, hyperlipidemia, hypertension, and smoking were self-reported. For simplicity of model score calculation and based on clinical input to represent young, middle, and older age, age was categorized as <50, 50 to 64, and ≥65 years. Body mass index was categorized as <30 and ≥30 kg/m 2 .
A logistic regression model built on the 24,637 patients in the derivation cohort identified the independent predictors of absence of obstructive CAD. We started with clinically relevant variables including gender, age group, electrocardiographic status, CCS angina class, body mass index, CAD risk factors (hypertension, hyperlipidemia, diabetes, and smoking), and self-reported co-morbidities (including cerebrovascular disease, peripheral vascular disease, chronic obstructive pulmonary disease, renal disease, and liver disease). Variables in the final model were selected based on statistical significance and clinical importance. Only clinically plausible interaction terms were explored.
A score for a given predictor in the final model was developed by rounding the corresponding model coefficient to the nearest 0.5 increment. The total score for a given patient is the sum of the scores for each predictor. A clinical prediction tool was derived with a total score cutoff for identifying patients with a low likelihood of obstructive CAD. To evaluate the predictive ability of the tool, sensitivity, specificity, positive predictive value, and area under the receiver operating characteristic curve were calculated. All statistical analyses were performed using SAS 9 (SAS Institute, Cary, North Carolina) and R version 2.10.1 (Free Software Foundation, Boston, Massachusetts). A significance level of 0.05 was used for all statistical analyses.
Results
Women accounted for approximately 1/3 of all patients. Absence of obstructive CAD was noted 2 to 3 times more frequently in women compared to men, with up to 51% of women being reported to have no obstructive CAD at ICA. Baseline characteristics are listed in Table 1 and invasive coronary angiographic findings in Table 2 .
| Characteristic | Derivation Cohort | Validation Cohort |
|---|---|---|
| (n = 24,637) | (n = 18,606) | |
| Women | 34.4% | 34.6% |
| Age (years), mean ± SD | 63.3 ± 11.5 | 61.4 ± 11.5 |
| Diabetes mellitus | 21.9% | 20.0% |
| Hyperlipidemia | 56.8% | 70.5% |
| Hypertension | 55.2% | 61.1% |
| Chronic obstructive pulmonary disease | 8.7% | 12.0% |
| Renal disease | 1.5% | 1.7% |
| Peripheral vascular disease | 6.9% | 6.2% |
| Ever smoked | 60.1% | 60.1% |
| Cerebrovascular disease | 6.0% | 5.5% |
| Liver disease | 6.5% | 6.0% |
| Canadian Cardiovascular Society angina class | ||
| Atypical | 3.0% | 3.6% |
| 0–I | 10.8% | 6.4% |
| II–IV | 86.2% | 89.9% |
| Body mass index ≥30 kg/m 2 | 29.2% | 37.0% |
| Stable angina pectoris | 41.7% | 51.9% |
| Acute coronary syndrome | 58.3% | 48.1% |
| Electrocardiogram | ||
| No ST-segment change | 59.8% | 70.0% |
| Ambiguous ST-segment changes | 10.1% | 4.1% |
| T-wave inversion | 10.0% | 6.7% |
| ST-segment depression | 7.0% | 10.0% |
| ST-segment elevation | 13.1% | 9.3% |
| Extent of Diseased Vessels | Derivation Cohort | Validation Cohort | ||||
|---|---|---|---|---|---|---|
| Women | Men | Overall | Women | Men | Overall | |
| Absence of obstructive coronary artery disease (no stenosis ≥50%) | 43.5% | 17.4% | 26.4% | 51.2% | 25.9% | 34.6% |
| 1-Vessel disease (stenosis ≥50%) | 22.1 % | 25.9% | 24.6% | 19.2% | 22.8% | 21.5% |
| 2-Vessel disease (stenosis ≥50%) | 15.5% | 23.3% | 20. % | 14.0% | 20.5% | 18.2% |
| 3-Vessel disease (stenosis ≥50%) | 13.9% | 24.4% | 20.8% | 12.0% | 22.9% | 19.2% |
| Left main stem stenosis (≥50%) | 5.0% | 9.0% | 7.6% | 3.7% | 7.9% | 6.5% |
In univariate analysis, all baseline characteristics examined were significantly associated with absence of obstructive CAD ( Table 3 ). In the multiple logistic regression model, gender, age group, CCS angina class, electrocardiographic status, diabetes, chronic obstructive pulmonary disease, smoking, peripheral vascular disease, hyperlipidemia, hypertension, liver disease, body mass index status, and interactions between gender and age group and between gender and diabetes were significant independent predictors of absence of obstructive CAD. Factors selected for inclusion in the final prediction tool, based on statistical significance and clinical importance, included gender, age group, electrocardiographic status, CCS angina class, diabetes, hyperlipidemia, smoking status, and interactions of gender and age group and of gender and diabetes. Estimates and p values for the final predictors are presented in Table 4 . The Hosmer-Lemeshow test suggested the prediction model provided a good fit to the derivation data (p = 0.3).
| Characteristic | Absence of Obstructive CAD | |
|---|---|---|
| Yes | No | |
| (n = 6,500) | (n = 18,137) | |
| Women | 56.7% | 26.4% |
| Age (years), mean ± SD | 60.1 ± 11.7 | 64.4 ± 11.2 |
| Diabetes mellitus | 15.6% | 24.1% |
| Hyperlipidemia | 49.3% | 59.5% |
| Hypertension | 51.1% | 56.7% |
| Chronic obstructive pulmonary disease | 10.9% | 8.0% |
| Renal disease | 1.0% | 1.7% |
| Peripheral vascular disease | 5.0% | 7.6% |
| Ever smoked | 53.6% | 64.5% |
| Cerebrovascular disease | 4.9% | 6.4% |
| Liver disease | 8.0% | 6.0% |
| Canadian Cardiovascular Society angina class | ||
| Atypical | 7.5% | 1.4% |
| 0–I | 15.3% | 9.2% |
| II–IV | 77.2% | 89.4% |
| Body mass index ≥30 kg/m 2 | 32.9% | 27.8% |
| Stable angina pectoris | 50.5% | 38.5% |
| Acute coronary syndrome | 49.5% | 61.5% |
| Electrocardiogram | ||
| No ST-segment change | 74.0% | 54.6% |
| Ambiguous ST-segment changes | 10.2% | 10.1% |
| T-wave inversion | 7.9% | 10.7% |
| ST-segment depression | 3.5% | 8.3% |
| ST-segment elevation | 4.4% | 16.3% |
| Factors | Model Results | Score | |||
|---|---|---|---|---|---|
| Estimates | p Value | Women | Men | ||
| Gender | |||||
| Women | 1.07 | <0.0001 | |||
| Men | — | ||||
| Age group | |||||
| <50 | 1.35 | <0.0001 | 2 | 1.5 | |
| 50–64 | 0.49 | <0.0001 | 1.5 | 0.5 | |
| ≥65 | — | 1 | 0 | ||
| Diabetes mellitus | |||||
| No | 0.37 | <0.0001 | 1 | 0.5 | |
| Yes | — | 0 | 0 | ||
| Electrocardiogram | |||||
| No ST-segment change | 1.66 | <0.0001 | 1.5 | ||
| Ambiguous ST segment | 1.4 | <0.0001 | 1.5 | ||
| Deep T-wave depression | 0.92 | <0.0001 | 1 | ||
| ST-segment depression | 0.51 | <0.0001 | 0.5 | ||
| ST-segment elevation | — | 0 | |||
| Canadian Cardiovascular Society angina class | |||||
| Atypical | 1.43 | <0.0001 | 1.5 | ||
| 0–I | 0.41 | <0.0001 | 0.5 | ||
| II–IV | — | 0 | |||
| Hyperlipidemia | |||||
| No | 0.46 | <0.0001 | 0.5 | ||
| Yes | — | 0 | |||
| Smoking | |||||
| Never | 0.19 | <0.0001 | 0.5 | ||
| Ever | — | 0 | |||
| Gender × no diabetes | 0.4 | <0.0001 | |||
| Gender × age <50 years | −0.23 | 0.0032 | |||
| Gender × age 50–64 years | 0.23 | 0.0462 | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


