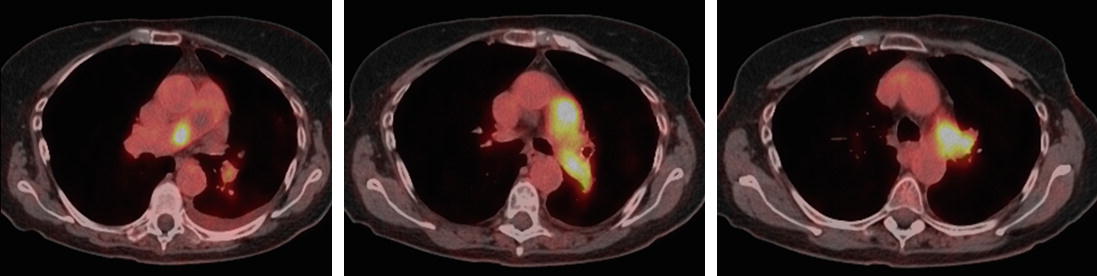
Selected images from computed tomography pulmonary angiography (see “Radiographic Interpretation” section for arrow explanations)
Past medical history included osteopenia, systemic hypertension, anxiety, gastro-esophageal reflux disease, and cataracts for which she had right eye surgery a few years prior. Her only other surgery was a total abdominal hysterectomy and oophorectomy more than 15 years before her current presentation. She had no known allergies, and no history of prior deep vein thrombosis, or pulmonary emboli. She also denied any prior estrogen use.
Social history disclosed no alcohol, tobacco, diet pill or illicit drug use. She worked as a flight attendant prior to retiring and was widowed. Her family history did not include any clotting disorder or any relatives with prior blood clots. She noted a rash with penicillin and some pruritus with enoxaparin and with clindamycin.
A few weeks after her discharge, she followed up as an outpatient with a pulmonologist due to continued shortness of breath and decreased exercise tolerance. Not only had she not returned to her baseline, but she occasionally experienced exertional chest tightness and palpitations that were alleviated with rest. On one occasion, after pushing herself to walk approximately 200 ft at a brisk pace, she felt dizzy and pre-syncopal. Her pulmonologist ordered an echocardiogram that showed a normal left ventricular size and systolic function, with mild diastolic dysfunction. Abnormal ventricular septal motion and position were noted, suggesting the presence or right ventricular pressure overload. The right ventricle was moderately enlarged and hypertrophied with reduced systolic function and the right ventricular systolic pressure was reported at 67 mmHg with a TAPSE measured at 1.32 cm. The left atrium was normal, the right atrium was moderately dilated and a trivial pericardial effusion was noted in addition to some moderate tricuspid regurgitation. The main pulmonary artery was enlarged and a large mass was seen within it.
Based on these findings and in the context of her more chronic and progressive symptoms with poor response to anticoagulation, chronic thromboembolic pulmonary hypertension was suspected and she was referred to a CTEPH center for pulmonary thromboendarterectomy (PTE) surgery evaluation.
During her evaluation for PTE surgery her vital signs were notable for elevated systemic blood pressure at 150/73, a temperature of 97 °F, a respiratory rate of 16, and a SpO2 of 98% on room air. Her height was 5′ 4″ and her weight was 60.5 kg. On exam, she had mild JVD and an accentuated P2 heart sound. Although her lungs were clear to auscultation bilaterally, a loud flow murmur was heard over her right lung zones during breath hold. Her only other finding were some lower extremity varicose veins.
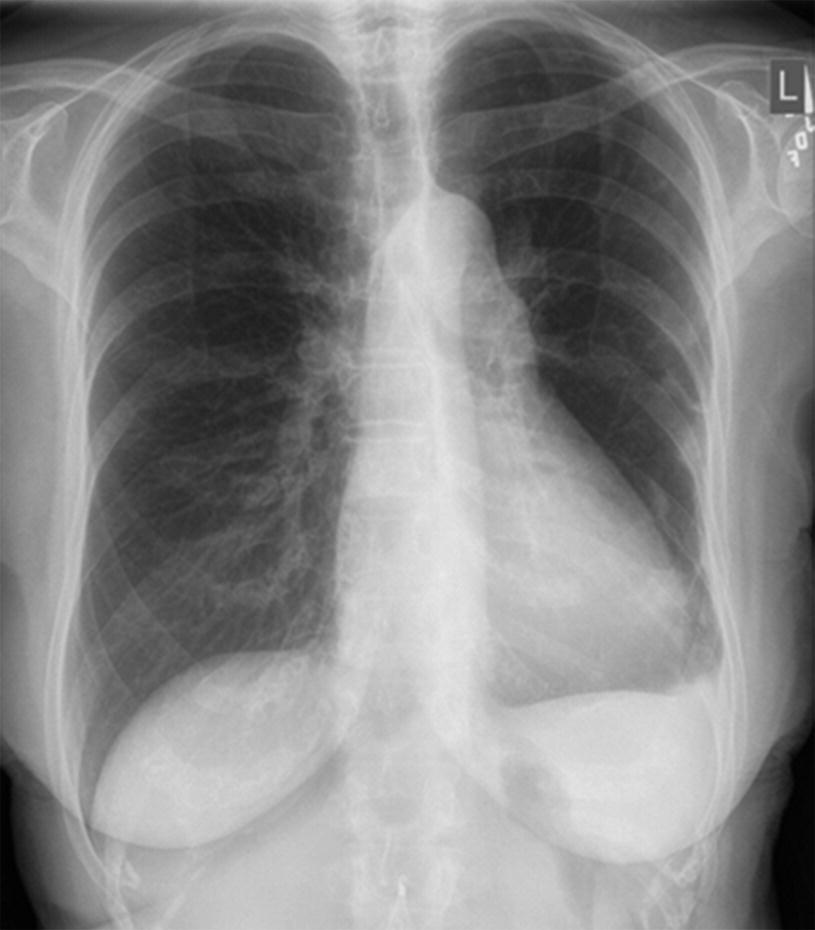
Chest radiograph
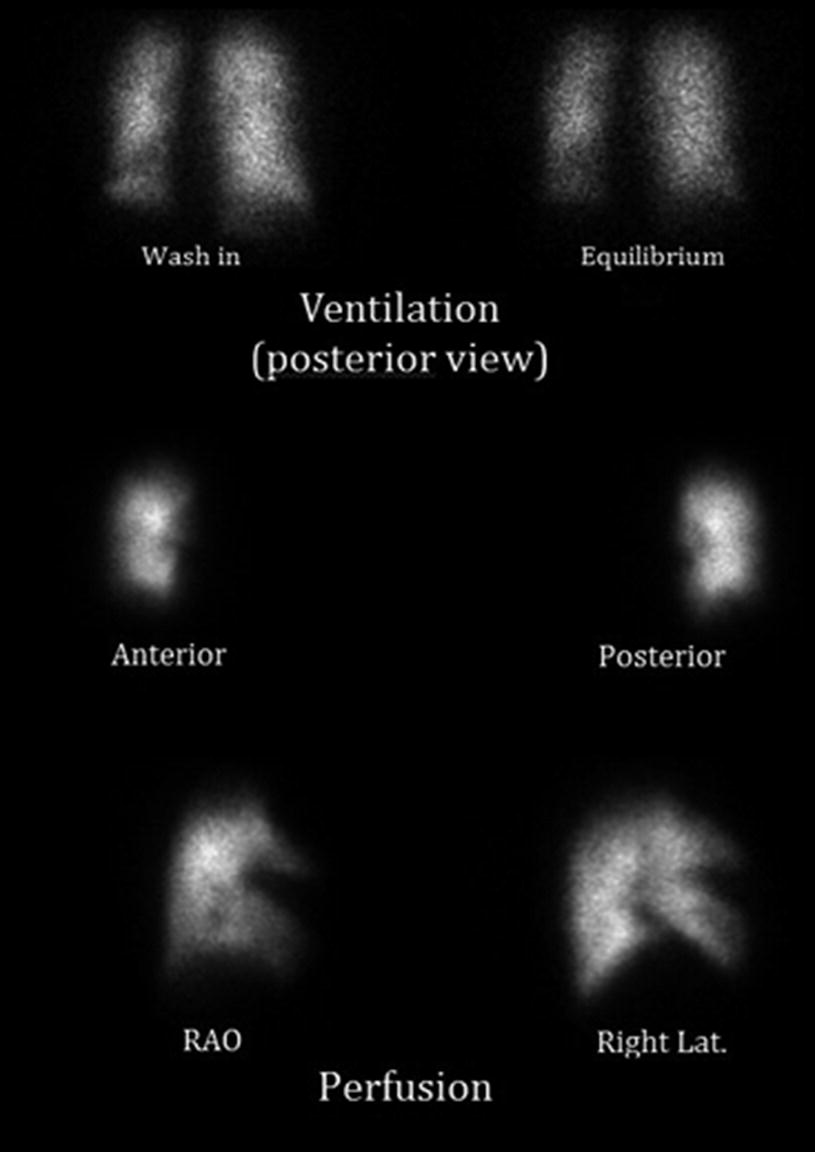
Ventilation perfusion scintigraphy (RAO: right anterior oblique, Lat: lateral)

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


