Traditionally, anaesthesia is viewed as being in four stages and the object is to obtain the third stage as quickly and smoothly as possible:
- Stage 1 – Disordered consciousness. This is now known as ‘induction’, and is the stage at which the patient passes from analgesia without amnesia to analgesia with amnesia, leading to unconsciousness.
- Stage 2 – Excitement. This is characterised by uncontrolled muscular movement, altered vital signs, pupil dilation, vomiting and possibly laryngeal spasm.
- Stage 3 – Surgical anaesthesia. This is achieved when the patient loses the ability to consciously respond to stimuli and reflexes serving muscle control become relaxed. It is at this stage a patient under a general anaesthetic will require support to maintain their airway via an appropriate airway adjunct.
- Stage 4 – Overdose. This stage is when a potential increased risk is present. If the anaesthetist does not titrate the level of anaesthetic to the surgical stimulation, this will cause an adverse impact upon the patient. Originally this was described as the ‘law of diminishing resistance’.
Staffing
Wherever anaesthesia is commenced, the anaesthetist must have exclusive and qualified assistance (AAGBI 2010, p. 10). This assistance typically takes the form of an anaesthetic practitioner, who can be either a registered nurse (RN) or an operating department practitioner (ODP). These assistants have two fundamental functions: to provide support to the anaesthetist and to support the patient, acting as advocate (Hughes and Mardell 2009). A third person should also be available to help support the patient and assist with any unforeseen occurrences.
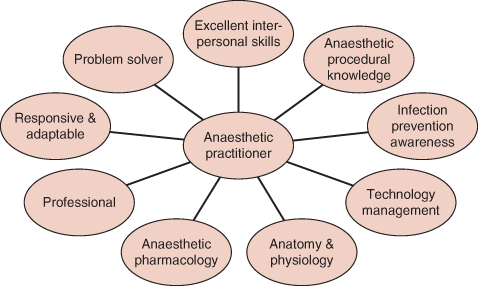
Figure 9.2 Qualities of an anaesthetic practitioner.
Training
Any anaesthetic practitioner must comply with the National Occupational Standards (NOS) (AAGBI 2010, p. 11). The RN is required to achieve additional professionally recognised and approved training before taking on the duties of an anaesthetic practitioner.
All relevant professional bodies acknowledge and positively encourage a programme of continuing professional development (CPD) for all anaesthesia practitioners. This will enable the practitioner to remain both vigilant and effective, thus maintaining a safe environment and delivery of the best quality care to the patient (Wicker and O’Neil 2006, p. 243). CPD forms the basis of employer reviews and professional registration compliance.
A clear function of the anaesthetic practitioner is to promote the wellbeing of the patient, to act as advocate and provide a professional approach to their duties. This is achieved by using sound, patient-centred, evidence-based practice and critical thinking, supported by a positive, reflective attitude. The application of a range of professional and personal skills is necessary to function as part of the anaesthetic multi-disciplinary team (MDT). Particular proficiencies must be evident in the form of preparation of the environment, maintaining health and safety, preparation of medical devices, undertaking vital signs monitoring, supporting the patient’s cardiovascular requirements and airway management (College of Operating Department Practice 2009).
The role of the anaesthesia assistant
The guiding principle for any practitioner working in anaesthetics is to ensure that the patient’s safety is maintained at all times (Younger 2000, p. 148). In order to achieve the best possible outcome for the patient, the knowledge base of the practitioner is continually advancing with core skills (Figure 9.1).
Many practitioners will evolve how they practice and will develop habits based upon their experiences; however this must be underpinned by best practice. Wicker and O’Neil (2006) argue that the basis of the anaesthetic practitioner’s role is to:
- prepare the environment
- prepare appropriate equipment
- ensure the safety checklist is completed
- support the patient as their needs dictate
- support the chosen method of anaesthesia
- work as part of a multi-disciplinary team (MDT)
- attach appropriate monitoring
- communicate any potential problems to relevant members of the MDT
- ensure documentation is accurate and complete.
When consultant anaesthetists are asked ‘What makes a good anaesthetic practitioner?’, a common response is ‘Someone who has what I need before I know I need it!’ While this is true, it only comes with exposure to a wide range of differing situations.
Figure 9.3 Immediate interdisciplinary team for surgical patients (from Hughes and Mardell 2009).
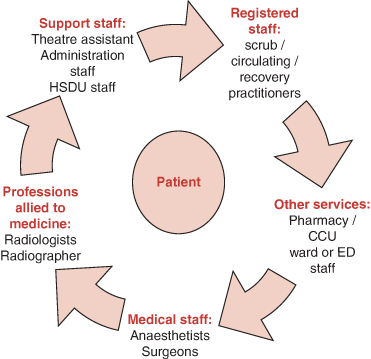
A critically important component in the operating department is communication. We must recognise our potential barriers, including gender, ethnicity, prejudices, professional rivalry, own limitations or organisational confusion to be able to overcome them. Gopee and Galloway (2009) suggest that clear and effective communication/information given to the patient preoperatively:
- improves the patient’s outcomes
- improves patient’s expectations
- requires less postoperative analgesia and
- reduces the patient’s length of stay in hospital.
The act of communication is a two-way meaningful process, not a rudimentary non- rhetorical remark or gesture (Russell 2005). To support the patient or member of the MDT an effective practitioner will adjust how, when and at what level there is a need to communicate (Figure 9.1). The NHS Institute for Innovation and Improvement (2009) advocates a framework referred to as ‘SBAR’ (situation, background, assessment, recommendation).
Environment
The size and layout of an anaesthetic room is guided by many factors, usually by recommended good practice through to statute intervention, such as the Association for Perioperative Practice (AfPP) (2011), Health and Safety Executive (HSE), Health and Safety at Work Act 1974 and NHS Estates (2005). The layout of the anaesthetic room should follow a logical sequence of when and where the practitioner needs to access items; for example, suction close to the anaesthetic machine, syringes close to needles, and so on. It should also be in close proximity to appropriately stocked stores.
The anaesthetic practitioner will develop his or her own way of working. Ideally, a routine should be established. Some may use the patient journey process – preparing monitoring first, then cannulae, airway equip, etc. Some may check their room in a clockwise manner. It does not matter which approach is used so long as it leads to nothing being forgotten or overlooked. Students and newly qualified practitioners should consider writing their ‘routine’ down so that they can refer to and adapt it.
Equipment
An essential aspect for any anaesthetic practitioner is the sound knowledge base regarding the equipment they will be expected to use. All medical devices are governed by the Medicines and Healthcare Regulatory Agency (MHRA), by the Medical Devices Regulations (MHRA 2002) plus subsequent amendments. Further regulation and guidance is taken from professional bodies, especially the AfPP (2011) and Association of Anaesthetists of Great Britain and Ireland (AAGBI 2004). The main tenets revolve around:
- not using unfamiliar equipment
- not using out of serviceable date
- following manufacturers instructions
- not using faulty equipment
- reporting faulty equipment as per the local protocol.
The primary guidance for checking anaesthetic equipment is issued by the AAGBI, which states that it is the responsibility of anaesthetists to be satisfied that checks have been carried out correctly. It is common practice for the anaesthetic practitioner to undertake initial checks. The AAGBI state that it is a mandatory activity to check anaesthetic equipment at the beginning of each session of use, and in the event of any changes to the current set-up (AAGBI 2004). These checks cover all aspects associated with the administration of anaesthesia, including the gas supply pipelines, the anaesthetic machine, filters, circuits, airway adjuncts, ventilators, suction, monitoring and ancillary equipment. A record of these checks should be kept with the anaesthetic machine (AAGBI 2004). A copy of the checklist produced by the AAGBI should be attached permanently to the anaesthetic machine.
The following advice is predominantly taken from the guidance issued by the AAGBI document entitled Checking Anaesthetic Equipment 3 (AAGBI 2004).
Anaesthetic machine
Most anaesthetic machines may be described simply as a box which draws in a medical gas (i.e. O2), the option to mix it with an anaesthetic agent and deliver a specific quantity of this gas/mixture to the patient via a circuit. Usually anaesthetic machines are connected directly to the mains electrical supply. Although other equipment can be connected into it, multi-socket extension leads must not be used with these devices. In essence, the anaesthetic machine is a collection of medical devices assembled in a convenient, transportable trolley.
In the event of machine failure an alternative method of effective oxygen supply is required. This can be via self-inflating bag or a circuit coupled with an oxygen cylinder. These items must be present in the anaesthetic room and checked appropriately.
Medical gas supplies
The anaesthetic practitioner should identify and note which gases are being supplied by pipeline and note that each pipeline is correctly inserted into the appropriate gas supply terminal. The use of size-specific connections should prevent cross-connection.
All machines have an oxygen failure alarm; testing this may involve disconnecting the oxygen pipeline on some machines. Repeated disconnection of gas hoses may lead to premature failure of the Schroeder socket and probe. As a result of this, a ‘tug’ test to confirm correct insertion of each pipeline into the appropriate socket is sufficient. If a gas master switch is present that should be used instead. In addition to these checks, the oxygen failure alarm must be checked on a weekly basis by disconnecting the oxygen hose while the oxygen rotameter/flowmeter is turned on. A written record must be kept. In addition to sounding an alarm which must sound for at least 7 seconds, oxygen failure warning devices are also linked to a gas shut-off device.
All gas pressure gauges for pipelines connected to the anaesthetic machine should indicate between 400 and 500 kPa.
Adequate supplies of any other gases intended for use must be available and connected as appropriate. All reserve cylinders should be securely seated and turned off after checking their contents.
Where fitted to an anaesthetic machine, the operation of rotameters/flowmeters must be checked, ensuring that each control valve operates smoothly and that the bobbin spins freely. If nitrous oxide is to be used, the anti-hypoxia device should be tested by first turning on the nitrous oxide flow and ensuring that at least 25% oxygen also flows. The oxygen flow should then be turned off and a check made that the nitrous oxide flow also stops.
Vaporisers
These units hold specific anaesthetic agents, such as Sevoflurane™ and Isoflurane™. They are used to either induce or maintain anaesthesia (Oakley and Van Limburgh 2005). The vaporiser(s) must be fitted correctly to the anaesthetic machine and secured to the back bar and the control knobs rotated. They should be kept upright at all times and not overfilled. Reference should be made to local policy with regard to the appropriate filling method, although COSHH regulations require that it should take place in a fume cupboard, unless fixed to the delivery unit, when filling should be carried out in isolation.
Humidifiers
Humidifiers are used to protect the patient’s respiratory tract and to counter the ‘drying out’ effect of anaesthetic gases. They also act as a barrier to potential microbiological bacteria. They are placed between the catheter mount and the breathing circuit.
Anaesthetic gas scavenging system
This system assists in the removal of anaesthetic gases. The anaesthetic practitioner must ensure that the system is switched on, connected to the machine and working correctly.
Circular absorption of carbon dioxide
Many modern anaesthetic machines have an absorption facility using modified soda lime crystals. This should be checked to ensure it is airtight and not exhausted. This process can produce caustic fluid, so glove-wearing is essential when changing the crystals and cleaning.
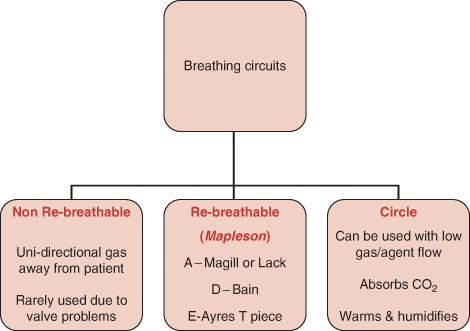
Figure 9.4 Breathing circuits.
Breathings systems
A breathing circuit is required to enable the delivery of anaesthetic mixtures from the anaesthetic machine to the patient via a facemask, laryngeal mask airway (LMA) or an endotracheal tube (ETT) (Oakley and Van Limburgh, 2005). There are three main types of circuit: non-rebreathable, rebreathable and circle (Figure 9.1). Rebreathable systems are subdivided into the ‘Mapleson classifications’, which are either open, semi-open or semi-closed. These are the most commonly used circuits in anaesthetics today (Hughes and Mardell 2009).
All circuits should be inspected manually for correct configuration and assembly before each use and changed as appropriate. The connections are secured by ‘push and twist’ motion. The practitioner should ensure that there are no leaks or obstructions in the reservoir bags or breathing system. A ‘dead cap’ should protect the patient end when not in use to prevent the intrusion of foreign bodies.
A new single-use bacterial/viral filter and angle piece/catheter mount must be used for each patient. It is important that these are checked for patency and flow, both visually and by ensuring gas flow through the whole assembly when connected to the breathing system.
Ventilators
On many anaesthetic machines, ventilators are inbuilt and undertake a self-check. However, if not, they need to be checked separately. The ventilator and tubing must be securely connected and the controls set for use ensuring that adequate pressure is generated during the inspiratory phase. The disconnection alarms should be checked for correct function.
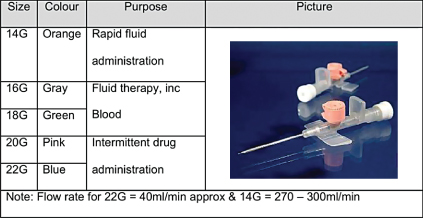
Figure 9.5 Cannulae comparison. Image of BD Venflon TM Pro Safety IV cannula reproduced with kind permission of BD UK Ltd.
Suction
Suction is required for rapid response to aspiration, regurgitation or vomiting by the patient during anaesthesia. The check should comprise confirmation function and connection security and also a test for the rapid development of an adequate negative pressure, done by occluding the tubing.
Cannulation
Intravenous access is a prerequisite for anaesthesia to be undertaken and is achieved by insertion of a cannula. Its placement in a blood vessel is for a variety of uses: administration of medicines, fluids or nutrition, invasive monitoring or haemodialysis (Wolverson 2008). In exceptional circumstances (e.g. babies or a needle-phobic patient), the patient can be induced without this access but it is established at the earliest opportunity.
In anaesthetics, the most common use is for the administration of anaesthetic medicines, usually via a peripheral vein.
Cannulae come in a range of sizes (Figure 9.1), the choice of which is dependent upon the size of vein and its use. The siting of peripheral cannulae can be into any viable vessel, though the most common are the back of the hand, forearm or antecubital fossa. A convention exists in the UK relating to the gauge size and specific colours. Once inserted, they must be secured with an appropriate transparent dressing. This is to enable the site to be observed for any potential signs of infection, reaction or haemorrhage. The size, location, time and date are recorded on patient documentation.
The use of invasive monitoring via an arterial cannula is only justified in certain circumstances when a severe change in blood pressure is expected. The uses of arterial lines include continuous/precise blood pressure monitoring or repeated arterial blood gases (ABG). An arterial line is usually sited in the radial artery, on the non-dominant hand side, though where peripheral access is difficult, the brachial or femoral arteries may be used on a short-term basis (Wolverson 2008). There are increased risks of bleeding, haematoma, ischaemia and infection when arterial lines are used, so great care is required when they are being inserted, secured, connected to and removed. The cannula is connected to a transducer, which converts the signal into a blood pressure reading. The transducer must be placed approximately level with the heart and ‘zeroed’ to atmospheric pressure (Hughes and Mardell 2009).
Central venous lines via the internal jugular, subclavian or femoral veins are used for monitoring central venous pressure (CVP), administration of medicines, infusions, nutrition, and long-term access or if there is poor peripheral access. They are typically inserted using the Seldinger technique (Wolverson 2008).
Monitoring equipment
Pre, peri and post anaesthesia the patient needs to be monitored effectively (AAGBI 2007). Direct clinical observations are a vital and effective form of monitoring and should be utilised as such (Thompson 2009) although advances in technological monitoring devices have increasingly become more sophisticated to help with this task. All apparatus must be functionality checked before use.
Monitoring devices must be attached before induction of anaesthesia and their use continued until the patient has recovered from the effects of anaesthesia (AAGBI 2007). Particular attention must be paid to ensuring that all devices used are clean, fit for purpose and free from obstruction.
Induction and maintenance of anaesthesia
The following are required for the induction and maintenance of anaesthesia:
- pulse oximetry – for measuring the circulating level of oxygen saturation, as well as heart rate (Oakley and Van Limburgh 2005)
- non-invasive blood pressure via a cuff attached externally to the patient.
- electrocardiograph
- fresh inspired and end-tidal gases and anaesthetic agents
- airway pressure – to avoid barotraumas and ensure adequate ventilation is taking place.
A nerve stimulator (whenever a neuromuscular blocking agent is used) and a way of measuring the patient’s temperature should also be available.
Patients who undergo an ‘operative procedure’ under either a regional technique or sedation must have a minimum of the following monitoring devices:
- pulse oximeter
- non-invasive blood pressure monitor
- electrocardiograph.
Thermoregulation
NICE defines hypothermia as a core temperature of below 35.0 °C and recommends that patients should be maintained as ‘comfortably warm’ (between 36.5 °C and 37.5 °C), pre and post operatively.
From an anaesthetic viewpoint, effective management of thermoregulation revolves around monitoring before and during the procedures. The patient’s temperature should be measured and documented before induction of anaesthesia and then every 30 minutes until the end of surgery.
It is noteworthy that hypothermia can be used to manage a patient during their operation (especially in neurological and cardiac surgery) after resuscitation or in the intensive care unit. This can be achieved via cooling catheters, cooling blankets, vests and leg wraps.
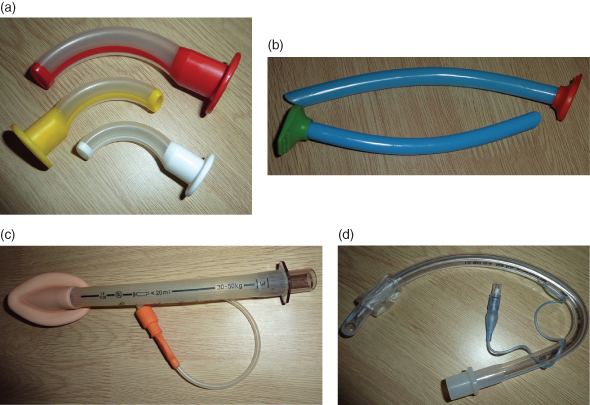
Airway adjuncts
There are five main categories associated with these devices (Figure 9.1):
- facemasks,
- oropharyngeal (OP airway)
- nasopharyngeal (NP airway),
- laryngeal mask airway (LMA)
- endotracheal (ET) tubes.
Figure 9.6 A range of different airways.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


