CASE 8 STEMI Intervention and Stent Thrombosis
Cardiac catheterization
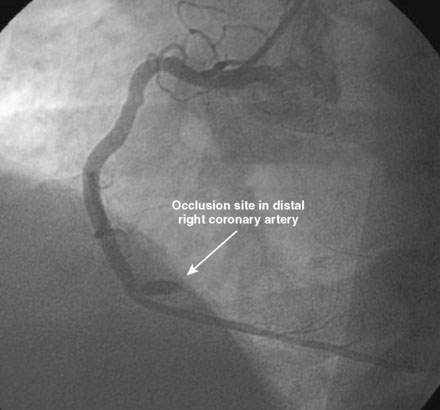
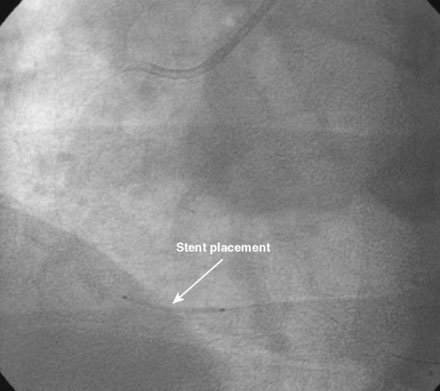
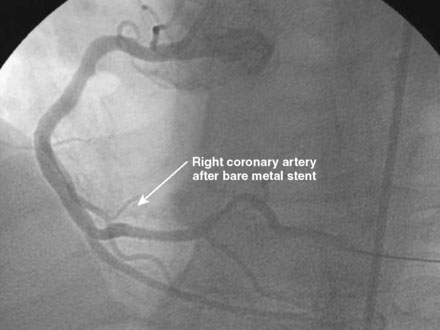
An ACT was measured and additional heparin administered to achieve an ACT between 250 and 300 seconds. Based on the ECG, the right coronary artery was the suspected infarct artery and was engaged first using a 6 French JR4 guiding catheter. Right coronary angiography revealed occlusion of the distal vessel, with retained contrast at the occlusion site (Figure 8-1 and Video 8-1). Eptifibatide was administered (two boluses, each of 180 mcg per kg, and an infusion of 2.0 mcg/kg per minute for 14 hours). The operator crossed the occlusion with a 0.014 inch floppy-tipped guidewire and TIMI-3 flow was restored after balloon dilatation with a 2.5 mm diameter by 15 mm long, compliant balloon. Following this, a 3.0 mm diameter by 23 mm long bare-metal stent was selected based on visual determination of the proximal and distal reference segments (Figure 8-2 and Video 8-2). A bare-metal stent was selected due to uncertainty about future medication compliance. The stent was positioned across the narrowed arterial segment and deployed at 14 atmospheres of pressure. The operator achieved a satisfactory angiographic result (Figure 8-3 and Video 8-3); intravascular ultrasound was not used.
Postprocedural course
Three months later, the patient again presented to the emergency department after suffering chest pains for 5 hours. The initial ECG demonstrated 3 to 4 mm ST elevations in leads 2, 3, and aVF with Q waves in those leads. The patient had not kept his previous medical follow-up appointments and admitted to stopping all of his medications after running out of prescriptions 3 weeks prior to the current presentation. Again, he was promptly treated in the emergency department with aspirin (325 mg), clopidogrel (600 mg), and unfractionated heparin (60 U/kg) and brought emergently to the cardiac catheterization laboratory. Right coronary angiography confirmed the suspected occlusion at the site of the previously-placed bare-metal stent (Figure 8-4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree