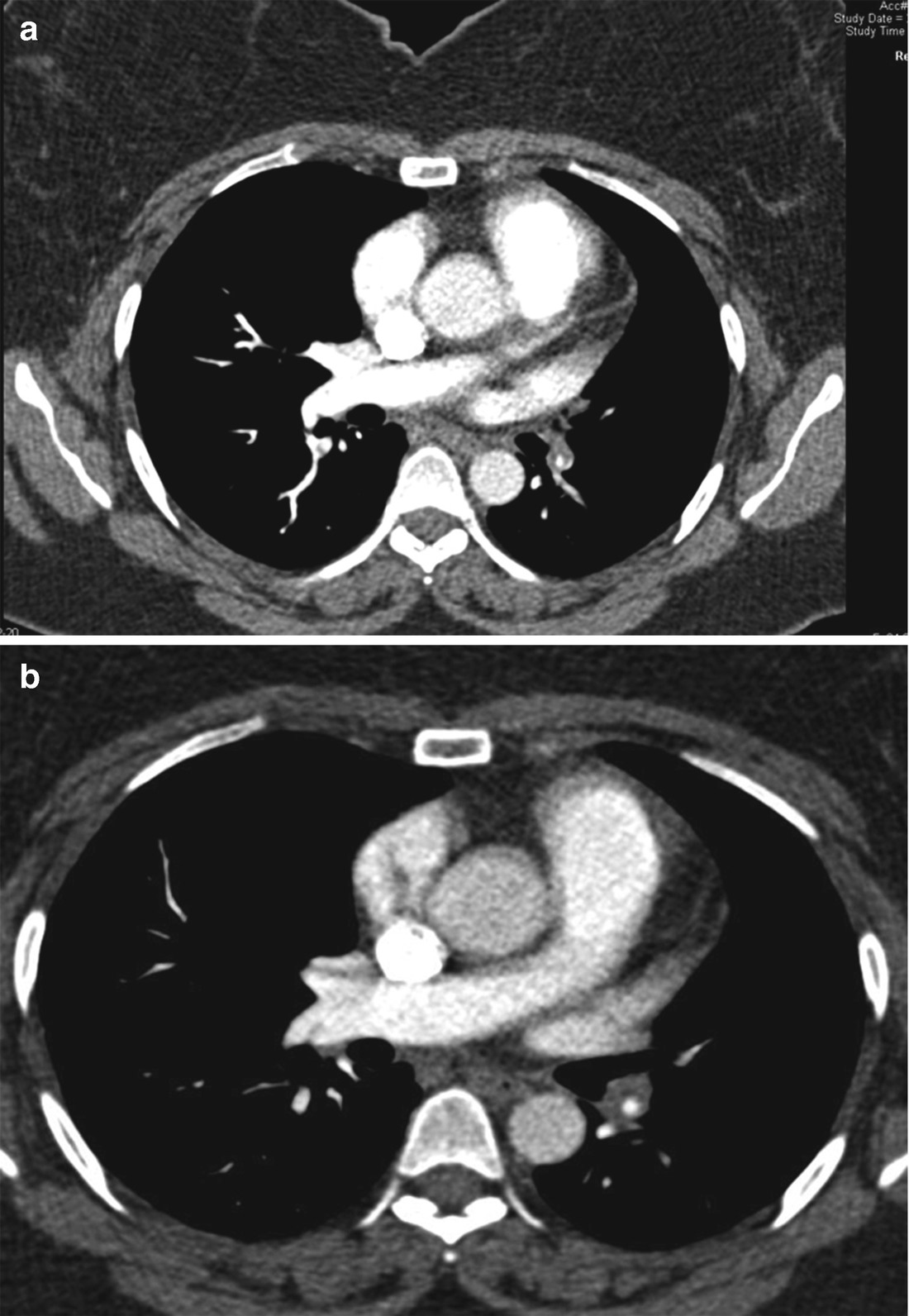
Selected images from computed tomography pulmonary angiography at time of diagnosis of pulmonary embolism
At the time of her acute pulmonary embolism, the echocardiogram revealed LVEF 50%, RV hypokinesis, RV pressure overload with PASP 40–45 mmHg. She did not require thrombolytic therapy. Troponins were negative. Lower extremity duplex dopplers were negative for acute deep vein thrombosis. She was placed on anticoagulation with enoxaparin and bridged to rivaroxaban. The PE was thought to be provoked from a long car trip. She complained of shortness of breath carrying her children and groceries. She had difficulty climbing stairs, though denied chest pain, lower extremity edema and presyncope.
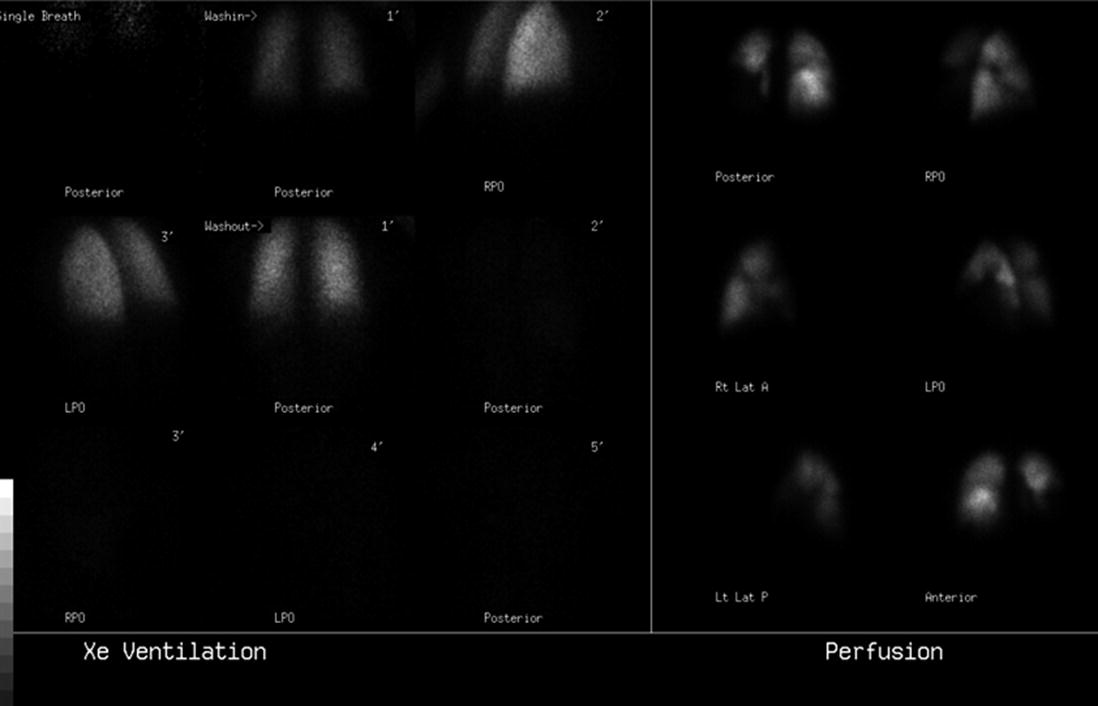
Ventilation perfusion scintigraphy 2 months post-acute pulmonary embolism
Her echocardiogram showed normal LV and RV size and systolic function, TAPSE 1.8 cm. PASP 35 mmHg, saline contrast study mildly positive for right to left shunt most consistent with a patent foramen ovale (PFO). Six minute walk test revealed a distance of 1050 ft and no desaturations with concluding Borg Score of 2. Pulmonary function testing was significant for reduced DLCO 44% predicted. Given that the acute pulmonary embolism was only 2 months prior and the echocardiogram did not show features of pulmonary hypertension or right heart enlargement, the perfusion defects seen on V/Q scan were felt to be due to her acute PE. Therefore, the decision was made to continue anticoagulation and repeat imaging 6 months after her acute pulmonary embolism.
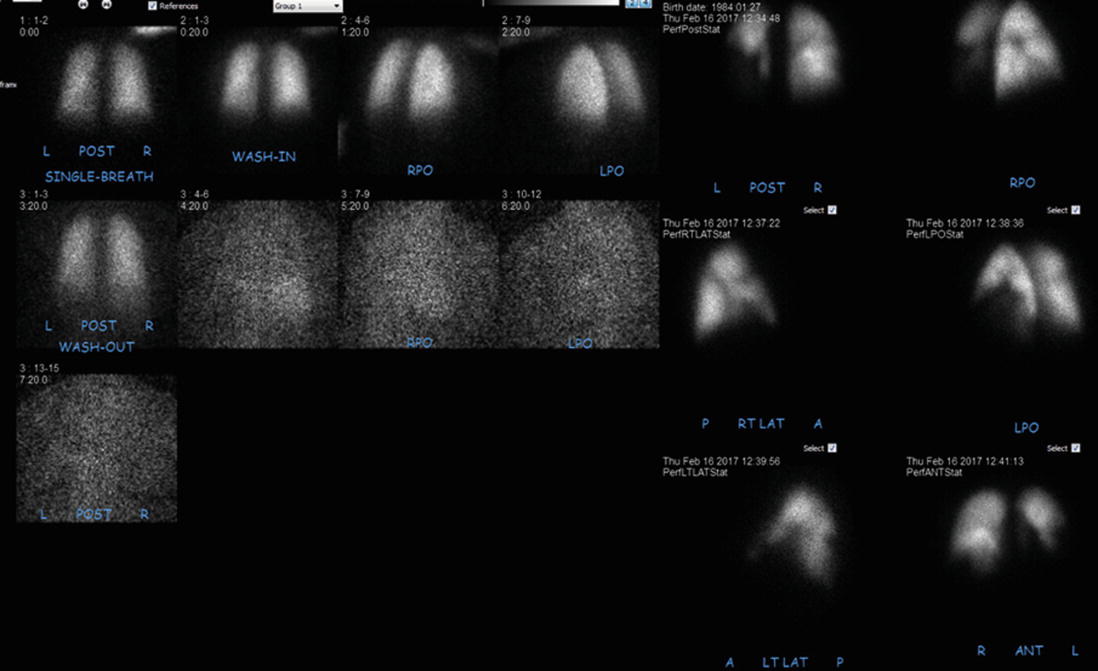
Ventilation perfusion scintigraphy 6 months post-acute pulmonary embolism
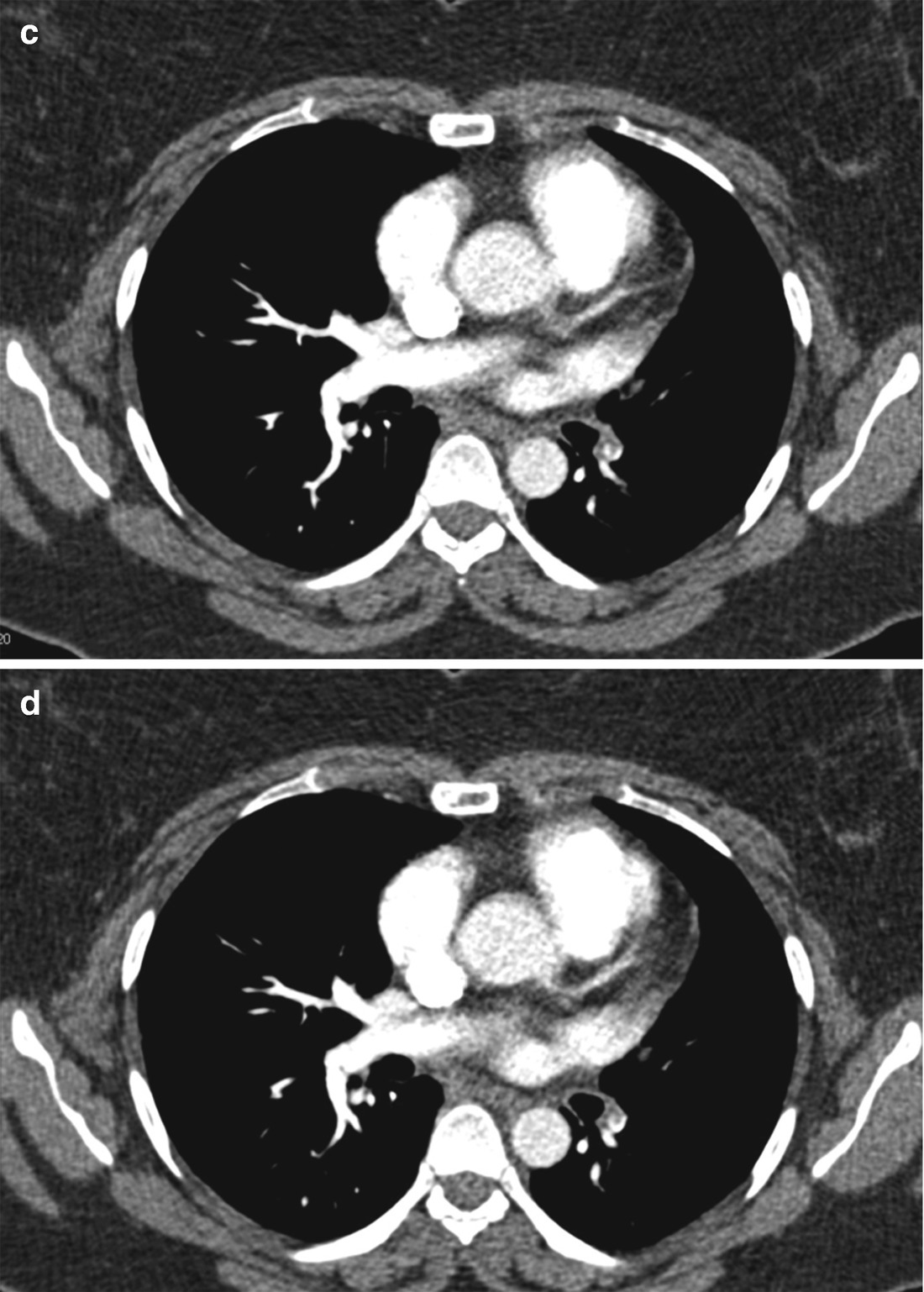
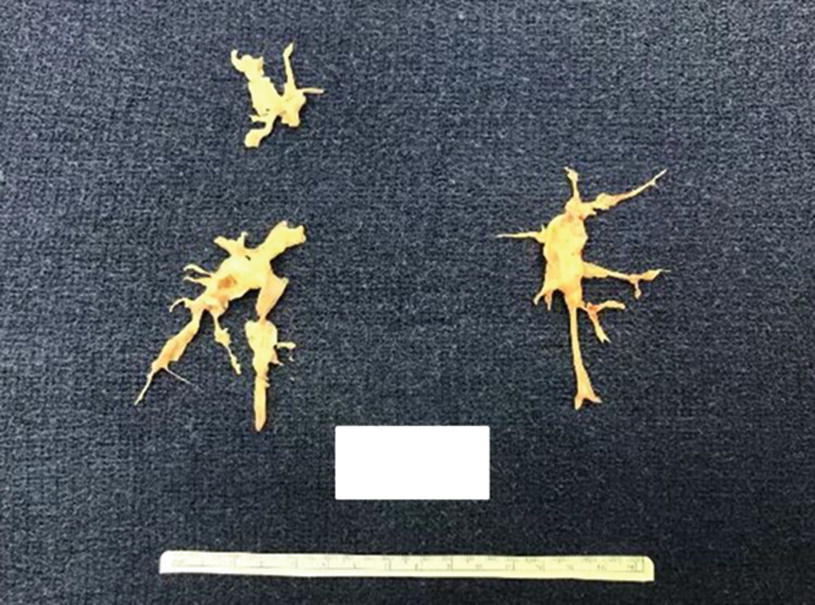
(a–d) Selected images from computed tomography pulmonary angiography 6 months post-acute pulmonary embolism
Due to her young age, persistence of symptoms 6 months post acute PE, with chronic changes consistent with chronic thromboembolic disease on CTA chest and V/Q scan, she was referred to CTEPH Center for evaluation and consideration of pulmonary thromboendarterectomy (PTE). A right heart catheterization was performed to evaluate for chronic thromboembolic pulmonary hypertension (CTEPH). Resting pulmonary hemodynamics: RA 10, PA 42/19 (mean 29), PCWP 14, thermodilution cardiac output 5.4 L/min, cardiac index 2.5 L/min/m2, PVR 2.8 Wood Unit, PA saturation 64%. Using weights, her upper extremities were exercised resulting in an increase in her thermodilution cardiac output to 8.1 L/min, PA pressure was 72/30 (mean 49), PCWP 17. She was diagnosed with chronic thromboembolic disease (CTED), characterized by persistent pulmonary thromboembolic occlusion with mild pulmonary hypertension at rest and significant rise in pulmonary artery pressures with a modest increase in cardiac output. As a result of her dissatisfaction with her functional status, and with her exercised induced pulmonary hypertension, she elected to proceed with surgery.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


