TOPIC 8 Adult congenital heart disease
Congenitally corrected transposition of the great arteries (L-transposition of the great arteries) 79
Genetic and non-genetic associations with congenital heart disease
Genetic
Table 8.1 Genetic syndromes associated with congenital heart disease
| Syndrome | Typical genetic defect | Typical cardiac defects |
|---|---|---|
| Down syndrome | Trisomy 21 | Atrioventricular septal defect, VSD, ASD, PDA |
| Holt–Oram syndrome | 12q2 | ASD, VSD |
| Turner syndrome | XO | Aortic coarctation, bicuspid aortic valve |
| Noonan syndrome | 12q | Pulmonary stenosis, hypertrophic cardiomyopathy |
| Di George syndrome | 22q11 deletion | Truncus arteriosus, tetralogy of Fallot, interrupted aortic arch |
| Williams syndrome | 7q11 deletion | Supravalvular aortic stenosis, peripheral pulmonary artery stenosis |
Non-genetic
Table 8.2 Non-genetic associations with congenital heart disease (known or suspected maternal factors)
| Infective | Rubella, toxoplasmosis, Coxsackie B virus |
| Environmental | Trichloroethylene, dichloroethylene, chromium |
| Iatrogenic | Antiepileptics, lithium, thalidomide, warfarin, isotretinoin |
| Lifestyle | Alcohol and illicit drug use, low folate intake |
| Medical | Diabetes mellitus, phenylketonuria |
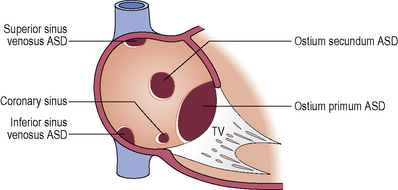
Atrial septal defect (ASD)
Communication between the atrial chambers allowing mixing of blood.
Clinical features
Pulmonary hypertension (ASD is associated with pulmonary hypertension though there is not thought to be a direct causal relationship)
Ventricular septal defect (VSD)
Clinical features
Clinical features depend upon the anatomy and haemodynamic severity of the VSD and presence of associated anomalies.
VSDs can be classified according to haemodynamic effect. The measured variables are the pulmonary artery: aortic systolic pressure ratio and pulmonary blood flow: systemic blood flow ratio.
Small: Pressure ratio < 0.3 and flow ratio < 1.4
Moderate: Pressure ratio > 0.3 and flow ratio 1.4 to 2.2
Large: Pressure ratio > 0.3 and flow ratio > 2.2
Eisenmenger: Pressure ratio > 0.9 and flow ratio < 1.5
Adults may have a small unrepaired VSD, a repaired VSD or Eisenmenger syndrome. Moderate or large VSDs are likely to have been repaired in childhood. Haemodynamically significant VSDs can lead to left heart pressure loading, right heart volume loading, pulmonary vascular disease and Eisenmenger syndrome.
Infective endocarditis.
Aortic regurgitation due to aortic cusp prolapse (outlet VSD and membranous VSD).
Arrhythmia: Atrial fibrillation may occur with left atrial dilatation secondary to left heart volume overload. Ventricular arrhythmia and late sudden death are reported.
Indications for adult intervention include:
Pulmonary artery systolic pressure > 50 mmHg. If the pulmonary artery pressure (or arteriolar resistance) is greater than 2/3 systemic arterial pressure (or arteriolar resistance), there must be evidence of a net left to right shunt of ≥ 1.5 or evidence of reactivity or potential reversibility (assessment with pulmonary vasodilator or lung biopsy).