CASE 6 High-Risk, Hemodynamically Supported PCI
Case presentation
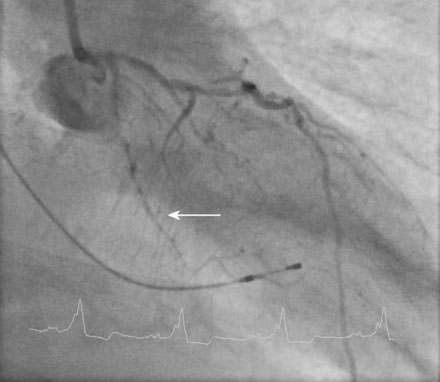
A fairly active 83-year-old man, with a past medical history notable for previous inferior infarction and ischemic cardiomyopathy, presented with a non-ST elevation myocardial infarction and congestive heart failure. His presenting electrocardiogram revealed an old left bundle branch block. Pertinent laboratory values revealed a brain natriuretic peptide (BNP) of 1473 pg/mL and a peak troponin of 2.28 ng/mL. Cardiac catheterization was performed during his initial hospitalization and revealed a severe mid-right coronary artery stenosis in a diffusely diseased, heavily calcified artery (Figure 6-1 and Video 6-1). The left coronary system was also heavily calcified and demonstrated a moderate-to-severe left main stenosis; a completely occluded circumflex with left to left collateralization (Figure 6-2 and Video 6-2); and a nearly occluded, severely diseased, ostial left anterior descending artery (LAD) (Figure 6-3 and Video 6-3). The LAD also provided collateral flow to the distal RCA territory. A cardiac MRI was subsequently performed to evaluate left ventricular function and myocardial viability. This demonstrated severely reduced left ventricular function (ejection fraction of 12.7%) and viability in the LAD territory. Transmural infarct was present in the inferolateral wall, representing the myocardium supplied by the right coronary and circumflex arteries. He was also noted to have a left ventricular thrombus and a 6 by 9 mm filling defect in the descending thoracic aorta that likely represented atheroma. Based on these findings, he was denied surgical revascularization. Thus, he was managed medically and was discharged on optimal medical therapy including a beta blocker, an ACE inhibitor, a nitrate, a diuretic, aspirin, clopidogrel, and a statin. However, within a 2-week period following discharge, he had two separate admissions for rest chest pain, heart failure, and recurrent non-ST elevation myocardial infarctions. Following the second admission, the decision was made to attempt high-risk percutaneous revascularization of the LAD.
Cardiac catheterization
Repeat angiography at the time of intervention was unchanged. Severe three-vessel disease with left main involvement, heavily calcified coronary arteries, significant collateralization of the RCA from the LAD, and a severely reduced ejection fraction, together placed the patient at significantly high risk for percutaneous intervention. Thus, the operator chose to employ a TandemHeart for hemodynamic support during the procedure. Prior to insertion, the left internal iliac was imaged to assure that the artery was of proper size and was without significant disease burden, to allow passage of the large arterial cannula required for the procedure (Figure 6-4 and Video 6-4). The artery measured 7.7 mm in minimum diameter and thus the operator inserted a 17 French cannula in the left external iliac percutaneously through the left common femoral artery. A transseptal puncture was performed; baseline hemodynamics showed a marked elevation of the left atrial pressure and preserved arterial pressure (Figure 6-5). The transseptal sheath was exchanged for a 21 French cannula placed via the right femoral vein into the left atrium (Figure 6-6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree