Preoperative chest radiograph showing a prominent right atrial shadow, with central PA enlargement
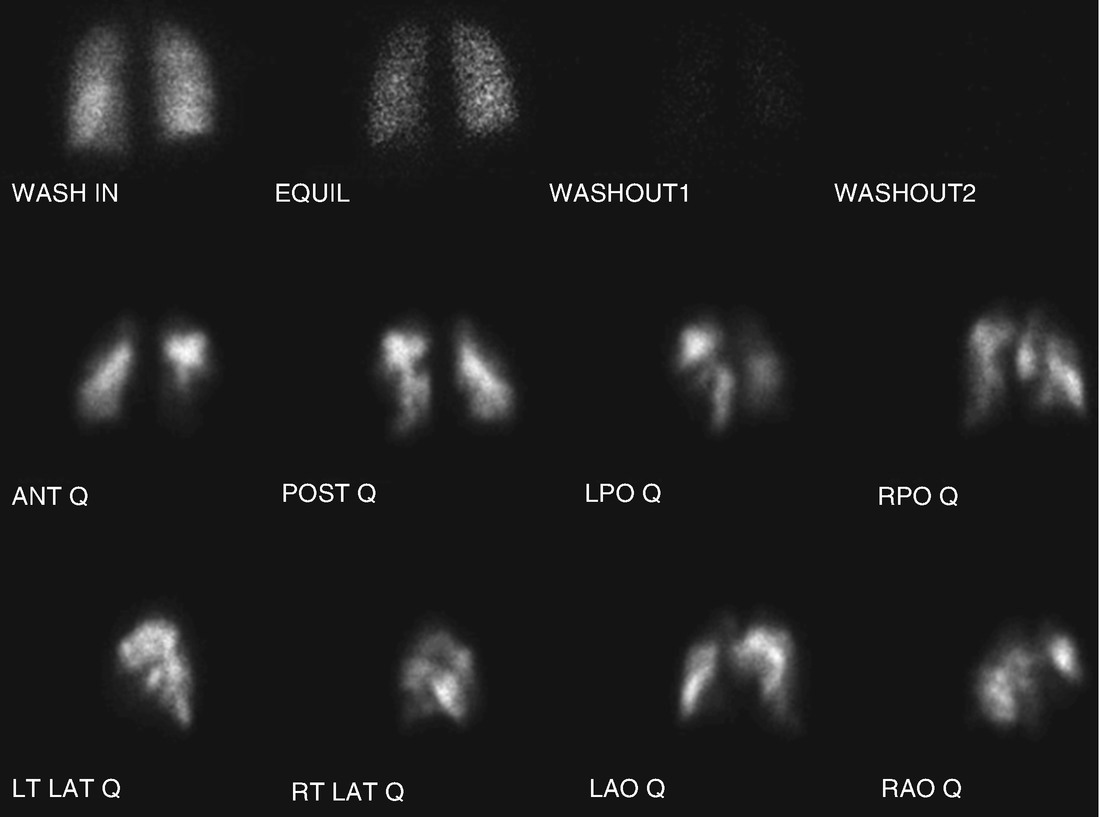
Preoperative lung scintigraphy demonstrating bilateral mismatched perfusion defects
An echocardiogram revealed RA and RV severely enlarged with depressed RV systolic function. LV size is small, with normal systolic function, TR velocity 4.5 m/s with PA systolic pressure 82 mmHg plus CVP, cardiac output 4.4 L/min, mild tricuspid regurgitation, absent pericardial effusion.
Laboratory data was as follows: Sodium 142, potassium 4.0, chloride 103, bicarbonate 24, BUN 15, creatinine 1.14, blood glucose 99. Liver function tests within normal limits except total bilirubin mildly up at 1.54. Urinalysis was negative for protein. White blood cell count 6.9, hemoglobin 13.6, hematocrit 41.5, platelets 259,000. INR 1.3, PTT 39.6.
Right heart catheterization showed right atrial mean pressure 10 mmHg, PA pressure 101/28 with a mean of 58 mmHg, Pulmonary capillary wedge pressure 13 mmHg, Cardiac output 3.30 L/min, cardiac index 1.95 L/min/m2, Pulmonary vascular resistance 1091 dynes/sec/cm-5.
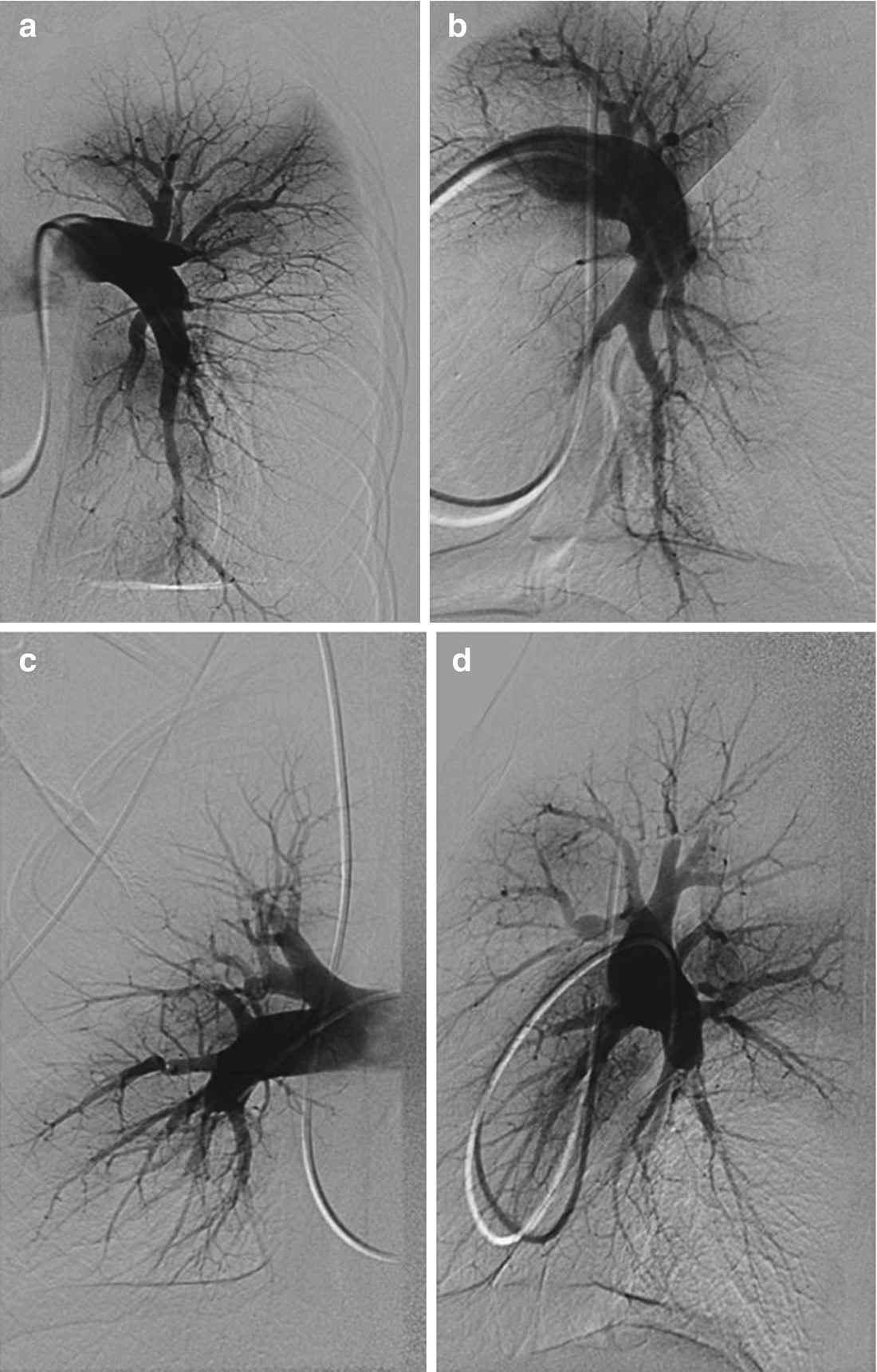
(a–d) Frontal (panel a) and lateral (panel b) views of the left pulmonary artery . Frontal (panel c) and lateral (panel d) views of the right pulmonary artery

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


