CASE 56 Mitral Balloon Valvuloplasty
Case presentation
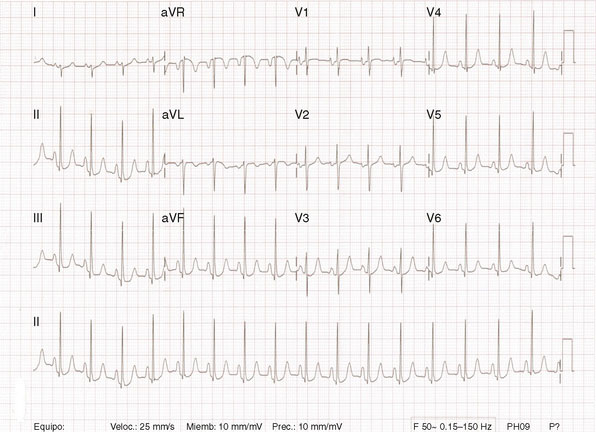
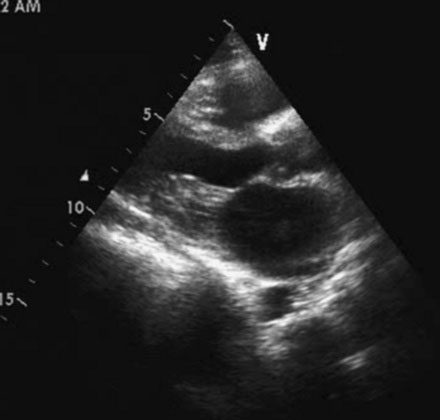
Several members of the Cardiovascular Division of the University of Virginia visit a medical clinic in Santo Domingo, Dominican Republic each year to provide tertiary care services for indigent patients with rheumatic heart disease. During one of these excursions, a 33-year-old Dominican woman presented with a 1-year history of worsening dyspnea on exertion. She reported fatigue and severe dyspnea with mild exertion but denied orthopnea or paroxysmal nocturnal dyspnea. She had been treated with a diuretic and aspirin with minimal improvement. On physical examination, she appeared healthy with a blood pressure of 110/80 mmHg and a regular pulse at 72 bpm. Her jugular veins were normal and lung fields clear. Cardiac exam revealed a loud first sound, an opening snap, and a diastolic rumble consistent with mitral stenosis without evidence of regurgitation. Her chest x-ray revealed left atrial enlargement, and a 12-lead electrocardiogram showed sinus rhythm with a right axis, evidence of right ventricular hypertrophy, and atrial enlargement (Figure 56-1). Her echocardiogram (Figure 56-2) confirmed the presence of rheumatic mitral stenosis with left atrial enlargement and a mean gradient by Doppler of 5 to 8 mmHg with only trace mitral regurgitation. The Wilkins score calculated to 8, based on the following characteristics: leaflets were severely restricted at the tips with the base showing normal mobility (score of 2); leaflet thickening appeared primarily at the margins (score of 2); there was only minimal leaflet calcification (score of 2); and there appeared to be modest thickening of the subvalvular apparatus (score of 2).
Cardiac catheterization
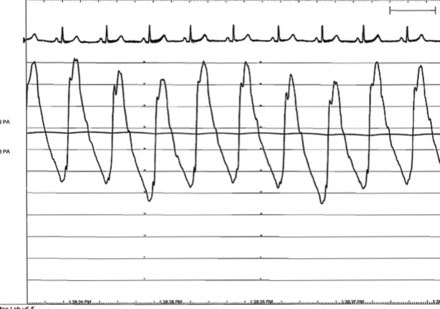
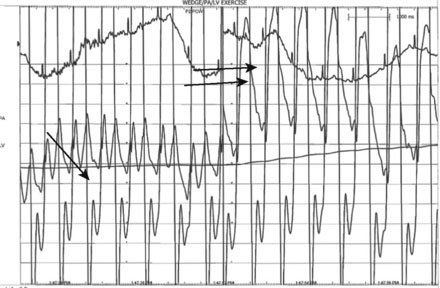
The pulmonary artery pressure measured 50/22 mmHg (Figure 56-3) and the baseline cardiac output measured 5.3 L/min. Simultaneous left ventricular and pulmonary capillary wedge pressures are shown in Figure 56-4. This confirmed a mean transmitral gradient of about 5 mmHg, and the valve area calculated to 1.4 cm2. Her symptoms appeared to be out of proportion to these findings and therefore, while on the cardiac catheterization laboratory table, exercise was performed by having the patient repetitively raise and lower a one liter bag of saline in each arm. The hemodynamic measurements were repeated after just a few minutes of exercise and showed a marked increase in pulmonary artery pressure (systolic pressure >65 mmHg) and an increase in the transmitral gradient to more than 10 mmHg (Figure 56-5). Based on the hemodynamic data, the patient’s symptoms, and the favorable echocardiographic findings, the operator proceeded with mitral balloon valvuloplasty.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree