CASE 51 Percutaneous Aortic Valve Replacement
Case presentation
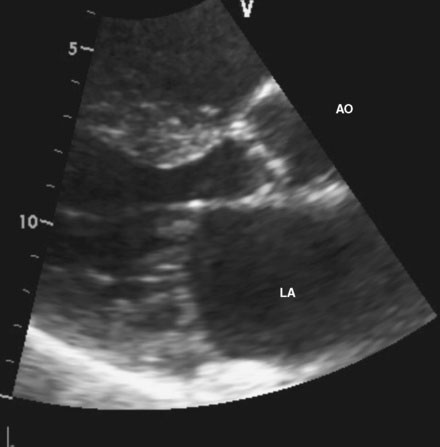
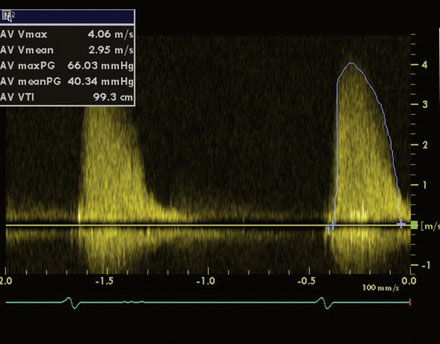
An 86-year-old man with previously known, asymptomatic aortic stenosis presented for an outpatient follow-up after a recent hospital admission for congestive heart failure and progressive angina. Before his admission with heart failure, he had noted several months of increasing shortness of breath with exertion and associated with chest tightness. During the office visit, his cardiologist obtained an echocardiogram that revealed severe, calcific aortic stenosis with a peak velocity of 4 m/sec, a peak instantaneous gradient of 66 mmHg, and a calculated valve area of 0.7 cm2, with preserved left ventricular function and an estimated pulmonary artery pressure of 70 mmHg (Figures 51-1, 51-2 and Video 51-1). In addition to the known aortic stenosis, his past medical history is extensive and includes chronic obstructive pulmonary disease, persistent atrial fibrillation, non–insulin-dependent diabetes mellitus, hypertension, dyslipidemia, obstructive sleep apnea, and coronary artery disease, with coronary bypass surgery performed 13 years earlier consisting of a left internal mammary artery to the left anterior descending artery, and saphenous vein grafts to the first and second obtuse marginals, to a large first diagonal, and to the right coronary arteries. He also has mild dementia, manifested primarily by short-term memory loss, but he remains functional and interactive with his family. Medications included metformin, ramipril, aspirin, furosemide, atorvastatin, and warfarin. He was referred for cardiac catheterization for further evaluation.
Cardiac catheterization
A hemodynamic evaluation found elevated right-sided heart pressures with a mean right atrial pressure of 19 mmHg and prominent V waves consistent with severe tricuspid regurgitation, pulmonary artery pressure of 63/18 mmHg (mean of 37 mmHg), and mean pulmonary capillary wedge pressure of 26 mmHg, with a cardiac output of 4.8 L/min and a valve area of 0.8 cm2. The native coronary arteries were all occluded but the left internal mammary and saphenous vein grafts remained patent and free of disease. Abdominal aortography found normal, large-caliber iliac arteries with moderate left-sided tortuosity (Figure 51-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree