Admission chest radiograph demonstrating cardiomegaly and massively enlarged central pulmonary arteries
Prior to presentation, he was unable to walk through large grocery stores without stopping. However, he drives, cares for himself, and does his other activities of daily living. He is using 3 L oxygen by nasal cannula at all times but his oxygen saturations drop to the 70s when walking short distances. Recently in clinic his 6-min walk test showed a distance of 134 m with oxygen saturations 80–86% on 25 L per nasal cannula.
His pulmonary function testing reveals an FEV1 of 1.89 L (54% of predicted), FVC of 3.66 L (78% predicted), and an FEV1/FVC ratio of 51%. The patient was unable to perform the lung volume or DLCO maneuver due to dyspnea and hypoxemia.
By provided history, at age 19 he was diagnosed with a pulmonary embolism after presenting with hemoptysis and was anticoagulated for several months but then enlisted in the United States Army and stopped his warfarin. He stayed off of the warfarin until 1990 when he presented with dyspnea and was found to have an “acute PE in the main pulmonary artery.” He again was treated with warfarin but only took it for 1–2 years and then was lost to follow-up. He presented to a health care provider for routine care and was restarted on anticoagulation in 2000 and has been on it ever since. He has been a heavy smoker for the past 30 years and was diagnosed with chronic obstructive pulmonary disease (COPD) a decade ago by pulmonary function testing. He started using oxygen about 8 years ago. The patient has had frequent admissions for COPD exacerbation characterized by productive cough, dyspnea, wheezing and an increased oxygen requirement. At the time of each episode he is treated with antibiotics and steroids and improves. His pulmonologist noted he had pulmonary hypertension, and recognized that it might be related to chronic thromboembolic disease after a ventilation/perfusion scan and computed tomography of the chest were obtained. He was started him on an oral prostacyclin approximately 8 months prior to presentation. The patient felt much worse on this and his oxygen requirement had been increasing.
Other past medical history included a gastric ulcer, chronic atrial fibrillation, gout, a chainsaw accident with a hand injury and squamous cell skin cancer. He has been evaluated for a thrombophilia but none was found.
Social History is notable for smoking 3/4 pack per day for 30 years. Upon presentation he was smoking e-cigarettes. He has a significant alcohol history and consumed at least 20 cans of beer per week for 30 years. He now drinks 1–2 beers per week. He worked in oil field, drilling. In the Army, he was a transportation security gunner.
Family history was significant for coronary artery disease but no clotting disorders, pulmonary emboli or deep vein thrombosis.
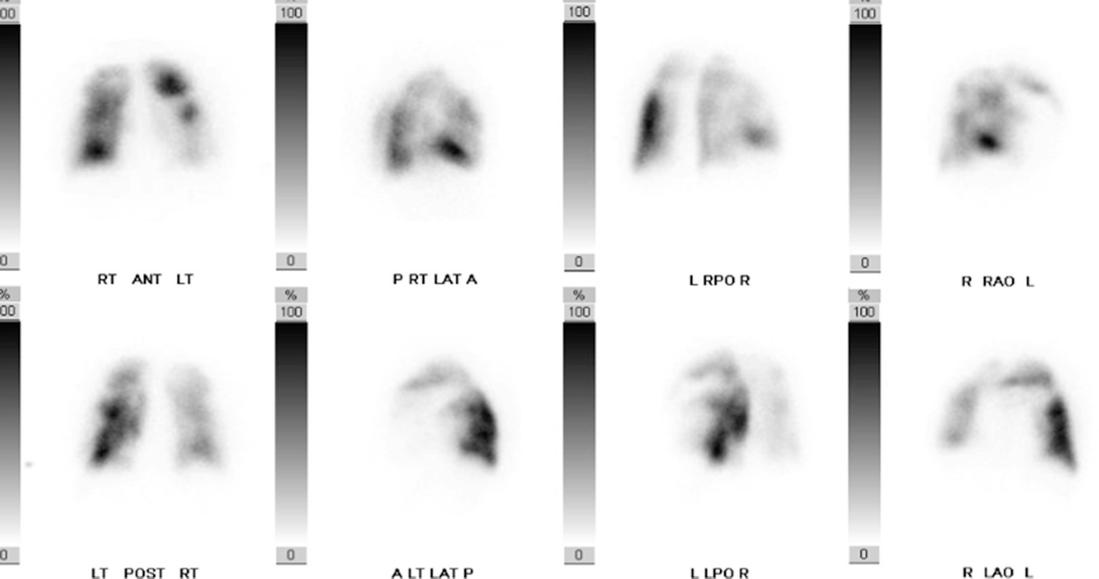
Abnormal perfusion scintigraphy with distinct segmental defects involving primarily the left lung
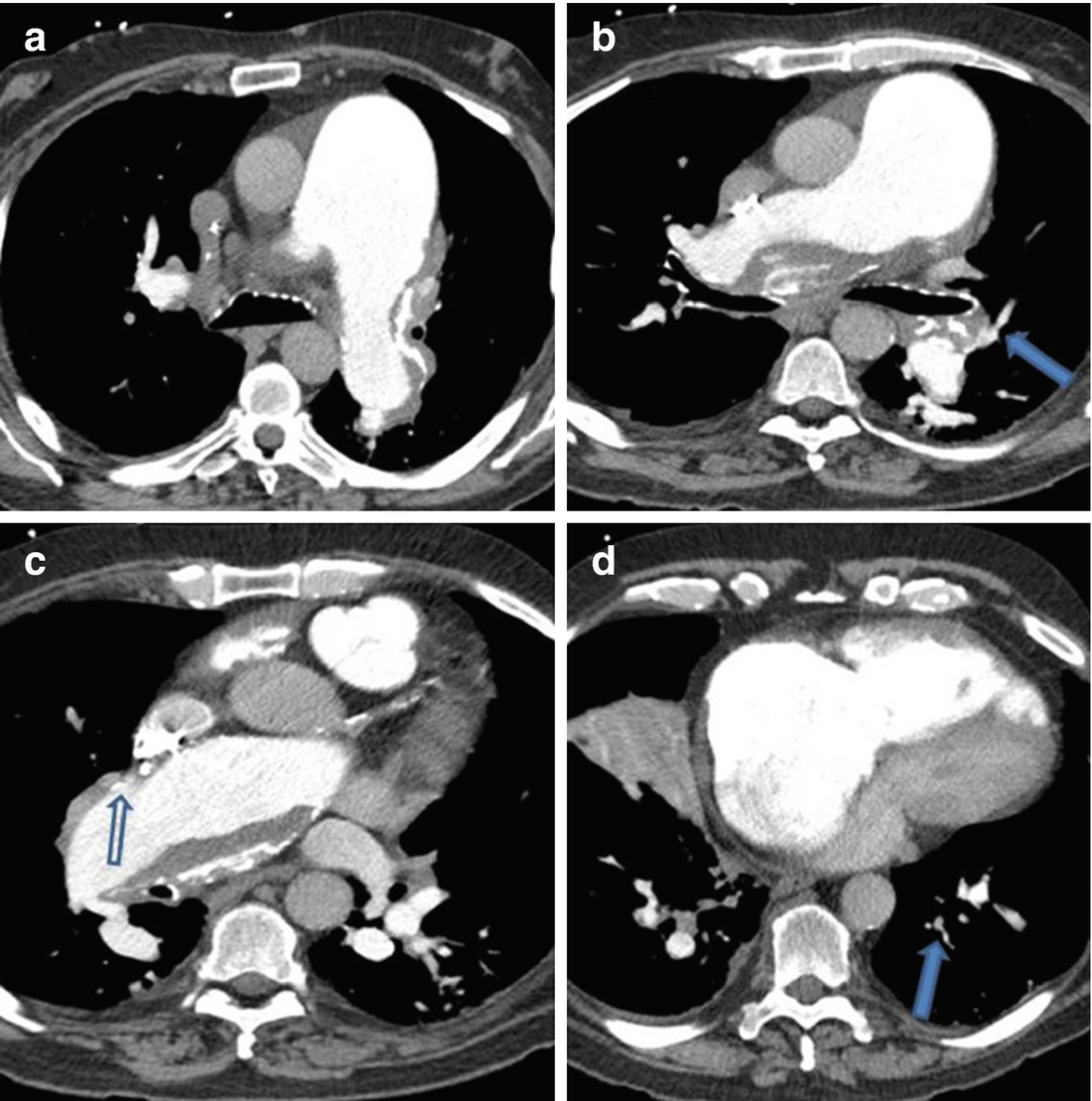
Calcified thrombus lining the central pulmonary vessels. (Panels a–c) Proximal vessel narrowing of the lingula (Panel b, arrow) from chronic thromboembolic disease, along with reduction in vascularity of the RML (Panel c, open arrow) and vessel attenuation (Panel d, arrow) due to involvement of the central vessels with calcified thrombus. Panel d also showing right atrial enlargement and hypertrophy of the RV free wall

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


