History
This 54-year-old man first sought treatment in 2005 with symptoms of progressive dyspnea on exertion, pedal edema accompanied by paroxysmal nocturnal dyspnea, and orthopnea. He had initially been treated in the community for upper respiratory tract infection with oral antibiotics but then developed symptoms of shortness of breath and fatigue. On further medical testing, he was diagnosed with dilated cardiomyopathy. His initial echocardiogram showed dilated cardiomyopathy with left ventricular internal diameter at end-diastole of 64 mm Hg, left ventricular ejection fraction (LVEF) of 18% with diffuse hypokinesis, moderate mitral regurgitation, left atrial enlargement, and moderate-to-severe tricuspid regurgitation.
The patient’s risk factors included active cigarette smoking, with a 25 pack-year history, and hyperlipidemia. He underwent cardiac catheterization, which showed mild obstructive coronary artery disease; however, this was unlikely to explain the severity of his cardiomyopathy and symptoms.
A single-lead implantable cardioverter-defibrillator (ICD) was originally placed in March 2010 for New York Heart Association (NYHA) class II symptoms with a QRS duration of 110 ms. Progressive worsening and widening of his QRS duration resulted in an upgrade to a cardiac resynchronization therapy defibrillator (CRT-D) with the addition of atrial and left ventricular leads. His NYHA classification had worsened to NYHA class III with hospitalizations for heart failure. Because of his relatively narrow QRS duration (126 ms), he also underwent a dyssynchrony echocardiographic study to ascertain the potential value of an upgrade of his ICD.
After the upgrade he came to our clinic for an unscheduled visit after being “bothered” by an audible tone from his device occurring every morning over several consecutive days. He described it as “an annoying occurrence” during his morning business meetings. His device interrogation was notable for inappropriate ICD therapy having occurred while he was asleep 7 days previously. The intracardiac electrograms documented atrial fibrillation with rapid ventricular response, which converted to sinus rhythm after he received one 34-J shock. After this initial shock he connected and established himself on our remote monitoring system.
He proceeded over the next several months to have several episodes of paroxysmal atrial fibrillation, which were detected accurately by his remote monitoring intracardiac electrograms, as exemplified in Table 48-1. Amiodarone therapy was started, but poorly tolerated secondary to neurologic effects of increased somnolence and fatigue, which led to the patient discontinuing the medication. On the amiodarone, his activity level decreased significantly, as seen on remote monitoring, although his biventricular pacing quantities went up significantly, as highlighted and circled in Figure 48-1.
The choices for alert alarms are audible and/or system monitor alerts that can range from 3 to 24 hours, including settings for the accompanying ventricular rates. For patients with heart failure, it is beneficial to set these parameters conservatively because the onset of atrial fibrillation could exacerbate their heart failure.
As a result of increasing heart failure symptoms, a month-long trial of turning off the left ventricular lead was done, but his heart failure symptoms worsened over the following weeks. As indicated earlier, his baseline QRS duration was fairly narrow, at 126 ms, which can be a substrate for nonresponse to CRT.
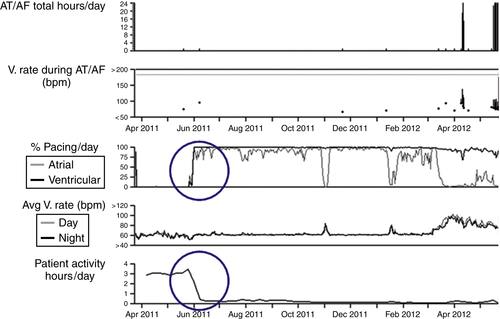
TABLE 48-1
Remote Arrhythmia Episode List
| Type | ATP Seq | Shocks | Success | ID no. | Date | Time hh:mm | Duration hh:mm:ss | Average BPM A/V |
| AT/AF | 102 | 17-Sep-2012 | 04:32 | (Episode in progress) | ||||
| AT/AF | 101 | 17-Sep-2012 | 03:48 | :44:22 | 178/98 | |||
| AT/AF | 100 | 17-Sep-2012 | 00:16 | 03:31:53 | 180/90 | |||
| AT/AF | 99 | 16-Sep-2012 | 02:17 | 21:58:27 | 180/91 | |||
| AT/AF | 98 | 15-Sep-2012 | 23:20 | 02:57:42 | 178/89 | |||
| AT/AF | 97 | 15-Sep-2012 | 01:10 | 22:09:17 | 180/90 | |||
| AT/AF | 96 | 15-Sep-2012 | 00:06 | 01:04:13 | 175/87 | |||
| AT/AF | 95 | 14-Sep-2012 | 14:10 | 09:56:19 | 178/88 | |||
| AT/AF | 94 | 14-Sep-2012 | 13:59 | :10:43 | 176/88 | |||
| AT/AF | 93 | 14-Sep-2012 | 08:20 | 05:38:34 | 176/88 | |||
| AT/AF | 92 | 14-Sep-2012 | 05:22 | 02:57:52 | 176/86 | |||
| AT/AF | 91 | 13-Sep-2012 | 19:38 | 09:44:24 | 169/83 | |||
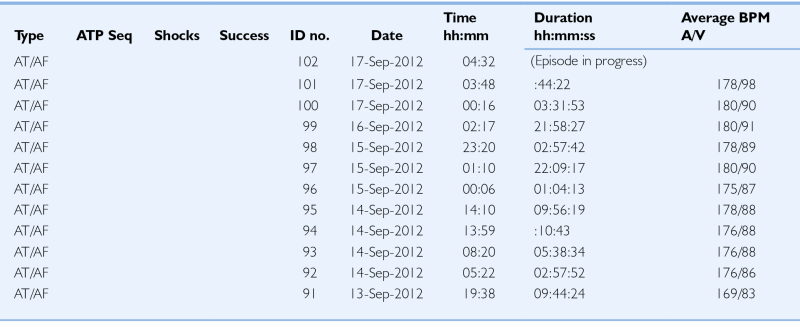
AF, Atrial fibrillation; AT, atrial tachycardia; ATP Seq, anti-tachycardial pacing sequence; A/V, atrioventricular; BPM, beats per minute; hh, hours; ID, identification; mm, minutes; ss; seconds.
As his heart failure progressed, he developed multiple episodes of nonsustained ventricular tachycardia, some of which occurred at ventricular rates as low as 131 bpm. These ventricular arrhythmias were preceded by elevations in his intrathoracic lead impedance fluid index trends measured in Ohms and identified as OptiVol in Medtronic (Medtronic, Minneapolis, Minn.) devices. His impedance measurements became important to monitor on a regular basis, because they were an accurate predictor of his heart failure exacerbations. Remote monitoring trends of these episodes are viewed in Figure 48-2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


