Temporary Cardiac Pacing
Intermountain Heart Institute, Intermountain Medical Center, Murray, UT, USA
Introduction
Temporary cardiac pacing is a commonly used tool in the practice of cardiovascular and intensive care medicine. Temporary cardiac pacing is typically used to treat a bradyarrhythmia until it resolves or a permanent pacing solution can be applied. Temporary pacing can be lifesaving in maintaining cardiovascular and hemodynamic function. Although temporary pacing can be used to treat tachyarrhythmias, the most common use is for significant, life-threatening bradyarrhythmias. Temporary pacing is required in approximately 20% of patients presenting to the emergency department with symptomatic bradycardia.1 This chapter will focus on the use of temporary pacing in cardiopulmonary resuscitation and reversible causes of significant bradyarrhythmias, and then highlight current temporary pacing options and approaches.
Cardiopulmonary Resuscitation
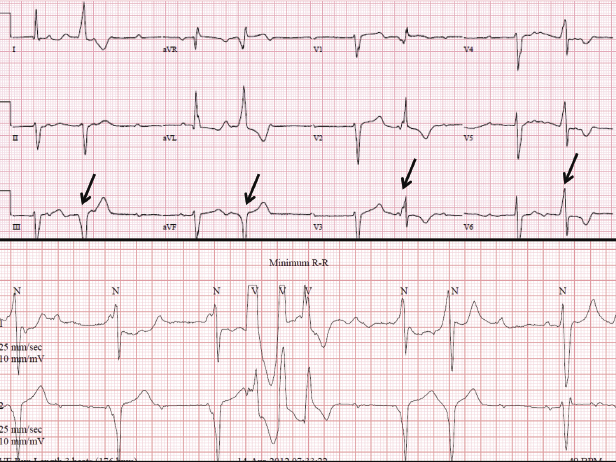
Symptomatic bradycardia can present with hypotension, signs of heart failure or cardiac ischemia, or electrical instability (Figure 4.1). There have been two randomized trials comparing temporary (transcutaneous) pacing versus drug therapy in patients who have symptomatic bradycardia with a pulse. Unfortunately, neither study demonstrated a clear survival benefit and as such, current guidelines suggest that pacing be considered only in those patients who do not respond to pharmacological approaches such as atropine.2–4 However, in patients who do not respond to pharmacological approaches, pacing is indicated.
In general, temporary pacing is not recommended for patients who present in asystole. Three randomized controlled trials have failed to show an improvement in survival to hospital admission or discharge with pacing in patients who had an asystolic cardiac arrest.5–8 In these patients, pharmacological approaches remain the mainstay of therapy, but if a patient is resuscitated to a bradyarrhythmia, temporary pacing may re-enter the resuscitation algorithm.
Reversible Causes of Severe Bradycardia
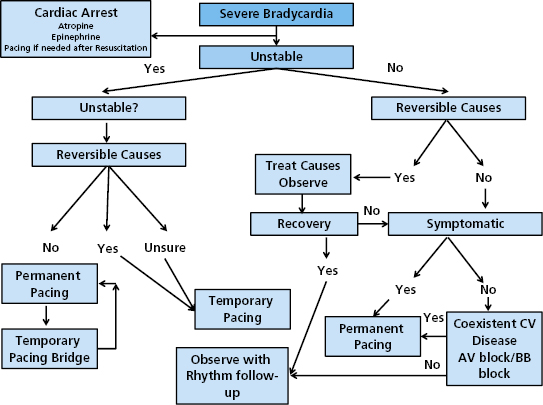
Temporary pacing is indicated for symptomatic bradycardia that stems from acute and reversible causes of cardiac instability. In these scenarios, temporary pacing may serve as a bridge to placement of a permanent pacemaker, or merely as a means to bypass this need while the reversible conditions are addressed. There are many potential reversible and/or acute causes of bradycardia that may require temporary pacing (Table 4.1). Unfortunately, although Table 4.1 details many potential reversible causes of injury, in some cases, despite removal or treatment of the offending source, long-term need for pacing may persist. Nonetheless, a careful patient history and laboratory investigation is required to exclude reversible causes of bradyarrhythmia, before committing the patient to long-term pacing. During the investigation of potential reversible causes of bradycardia there may be a need for temporary pacing. An algorithm is provided in Figure 4.2 to show our approach in a patient who presents with symptomatic bradycardia.
| Metabolic/electrolyte |
| Drug-induced/toxic: |
| Digoxin |
| Antiarrhythmic drugs |
| β-Adrenergic blockers |
| Calcium channel blockers |
| Clonidine |
| Cardiac ischemia |
| Injury to the sinus node and/or atrioventricular (AV) node during cardiac surgery |
| Post cardiac transplant |
| Central nervous system injury |
| Infectious: |
| Lyme carditis |
| Bacterial endocarditis |
| Influenza |
| Trauma to the AV node or His–Purkinje system during a cardiac procedure: |
| Electrophysiology study of catheter placement |
| Catheter ablation near the sinus node, AV node, or His bundle |
| Right heart catheterization |
| Cardiac pacing |
| Transcutaneous aortic valve placement/valvuloplasty |
| Ethanol ablation for hypertrophic cardiomyopathy |
| Paroxysmal atrial tachyarrhythmias |
| Autonomically-mediated syndromes |
Table 4.1 Examples of potentially reversible causes of symptomatic bradycardia
Temporary Pacing Options
Transcutaneous Pacing
The ability to pace transcutaneously was first described in the 1950s by Zoll.9 Dr Zoll reported the successful treatment in two patients of asystole with subcutaneous needle electrodes. Since the establishment of the utility of this concept, transcutaneous pacing has been an integral part of the treatment of bradyarrhythmias in the emergency setting.
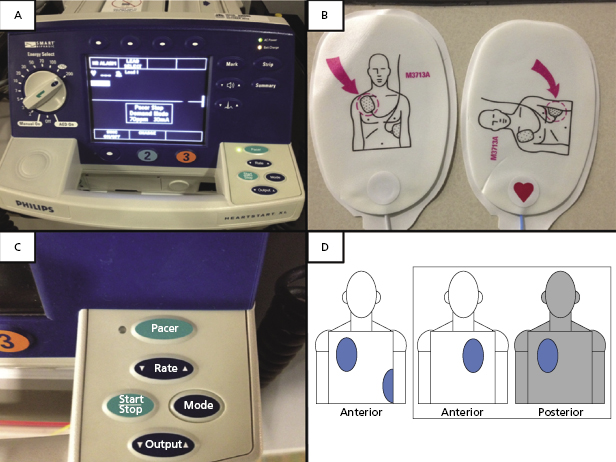
The successful application of transcutaneous pacing requires pacemaker pads and cables, a pulse generator unit, electrocardiogram (ECG) patches, monitoring equipment, and analgesia/sedation (Figure 4.3). Placement of the pads, as shown in Figure 4.3, is typically done by using one of two configurations. One option is an anterior and posterior placement. The anterior pad is placed on the left chest over the heart and the posterior patch immediately behind this pad on the left upper quadrant of the back. Another option is to place one pad on the right upper chest and the other pad lateral over the region of the anticipated apex of the heart.
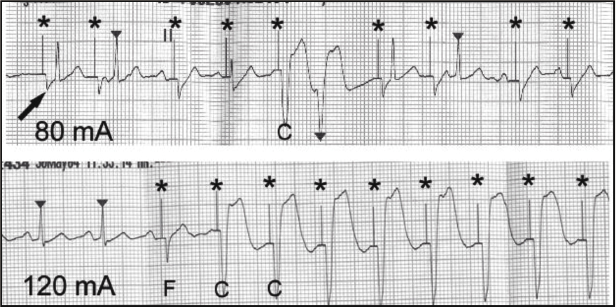
Initially the pacing rate is often set between 70 and 80 bpm. The generator current is increased until there is capture of the myocardium and then typically increased by an additional 10 mA above this capture threshold. The transcutaneous pacing threshold is variable amongst patients and their disease state, typically between 40 and 80 mA, and lowest in healthier individuals.10–12 Care must be taken to confirm that stable and complete capture of the myocardium has been accomplished as the transcutaneous pacing will result in pacemaker spikes on telemetry monitoring; a finding that may not necessarily confirm that capture has also been accomplished. Adequate capture may be verified with palpation of the femoral or carotid pulse, or by observing arterial pressure waveform (if an arterial line is present). Careful monitoring of the ECG with evidence of temporary transcutaneous electrical capture is shown in Figure 4.4;13 there is initiation of pacing, followed by fusion with the native sinus complexes, and ultimately complete ventricular capture. In patients with co-existent sepsis or hypotension, additional confirmation of pacing capture may be required with echocardiography.14 Table 4.2 outlines common causes of failure to capture during transcutaneous pacing and the respective solution to consider.
| Cause | Solution |
|---|---|
| Suboptimal lead position | Reposition leads, avoiding scapula, sternum, and spine |
| Negative electrode placed posteriorly | Place negative electrode anteriorly over apex or V3 |
| Poor skin–electrode contact | Clean skin of sweat and debris; shave body hair |
| Faulty electrical contacts | Check electrical connections |
| Generator battery depletion | Charge battery or plug-in generator |
| Increased intrathoracic air | Reduce positive pressure ventilation; relieve pneumothorax |
| Pericardial effusion | Drain pericardial effusion |
| Myocardial ischemia/metabolic | Cardiopulmonary resuscitation, ventilation, correct acidosis/hypoxia/derangements electrolyte abnormalities |
| High threshold | Shave hair beneath electrodes, apply pressure to patches, apply patches with fresh gel |
Table 4.2 Failure to capture during transcutaneous pacing13
Transcutaneous pacing is painful. Sedation and analgesia are often required, and at levels that may necessitate general anesthesia with intubation. Furthermore, the side effects of these medications can impact hemodynamic stability in an already compromised patient. In addition, there can be a mild reduction in cardiac function and stroke index due to atrioventricular (AV) dyssynchrony during transcutaneous pacing.15 As such, transcutaneous pacing largely is used as a temporary bridge to either permanent pacing or a more stable and tolerable endovascular temporary pacing modality.
Temporary Endocardial Pacing
Transvenous endocardial pacing is the most stable means to provide temporary pacing. There are various types of electrode catheters available for temporary pacing. Unlike transcutaneous pacing, once transvenous pacing is initiated, it is typically well tolerated. As such, transvenous pacing can be applied for extended periods of time, unlike transcutaneous pacing. Furthermore, depending on the type of electrode catheter used, patients can remain ambulatory.
The tools required for temporary endocardial pacing continue to evolve. Initially, transvenous electrode catheters are inserted through a large vein, typically the femoral vein, using a modified Seldinger technique (Figure 4.5). The catheters can be balloon tipped to allow easier and safer navigation into the right ventricle (RV).16 There are different catheter sizes and shapes that enhance their stability in the right atrium and ventricle. However, typically, an atrial catheter is not inserted as the procedure is largely viewed as temporary for a reversible condition and control of the ventricular rate provides the quickest avenue towards stability. At times dual chamber pacing may be helpful. These potential scenarios will be discussed later in this chapter.
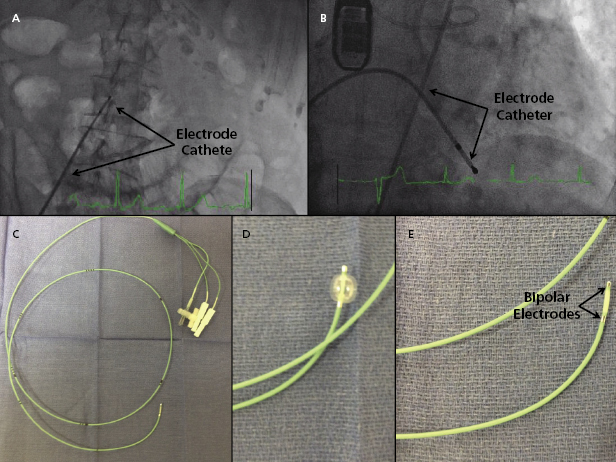
Figure 4.5 shows the insertion of a 5-Fr balloon-tipped, relatively stiff temporary electrode catheter via a transfemoral approach. In this case, the electrode catheter was placed as a precaution at the time of a transcutaneous aortic valve placement in case high-grade AV block developed during the procedure. A femoral venous approach offers a rapid, stable access for temporary pacing.17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


