CASE 39 PCI Versus Medical Therapy for Stable Angina
Case presentation
A 73-year-old woman with a past medical history of poorly controlled hypertension, hyperlipidemia, hypothyroidism, and gastroesophageal reflux disease and a family history of coronary artery disease presented with exertional chest and arm discomfort and shortness of breath. She underwent an exercise stress thallium test during which she exercised 6 minutes in a standard Bruce protocol, achieved 73% of her age-predicted heart rate, and reached a maximum blood pressure of 200/90 mmHg. The test was terminated secondary to fatigue. Nuclear imaging revealed no convincing evidence of ischemia. Due to continued symptoms, she underwent cardiac catheterization. The right coronary artery was dominant, with minimal disease (Figure 39-1). The left coronary showed minimal disease of the left anterior descending artery and a severe stenosis in the mid-circumflex artery (Figures 39-2, 39-3 and Video 39-1). After her physician discussed the risks and benefits of percutaneous intervention versus optimal medical therapy, she chose medical management. Her medical regimen was maximized and included an angiotensin-receptor blocker, a calcium-channel blocker, aspirin, a beta-blocker, long-acting nitrates, and a statin. However, despite this therapy, she continued to experience exertional chest pressure and shortness of breath that significantly limited her physical activity. Thus, 3 months later she decided to pursue percutaneous intervention of the circumflex artery.
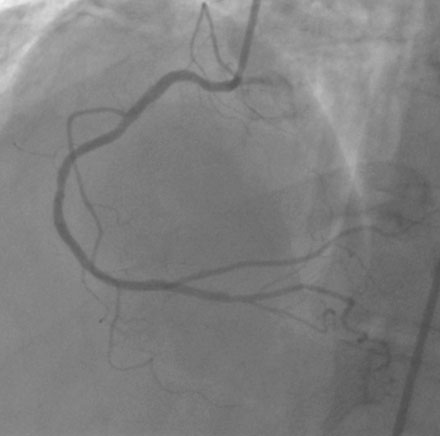
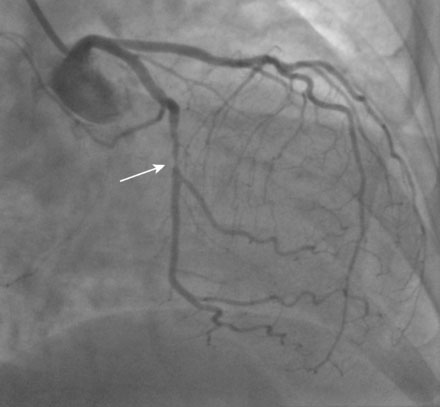
FIGURE 39-1 Right coronary angiogram, demonstrating a dominant right coronary artery with minimal disease.
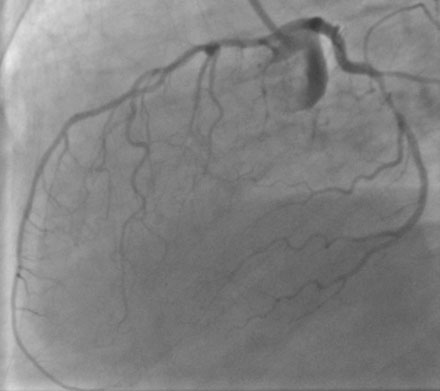
FIGURE 39-2 This lateral projection of the left coronary artery demonstrated minimal disease in the LAD.
Cardiac catheterization
The lesion appeared unchanged by angiography. Anticoagulation was achieved with a bolus and infusion of bivalirudin. A 0.014 inch floppy-tipped guidewire was advanced into the circumflex artery beyond the lesion. The lesion was successfully predilated with a 2.0 mm diameter by 20 mm long compliant balloon. A 2.5 mm diameter by 24 mm long drug-eluting stent was then deployed (Figure 39-4 and Video 39-2). Hemostasis was achieved with a vascular closure device and she was discharged the next morning after an uncomplicated overnight stay.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree