CASE 36 Multivessel Coronary Artery Disease
PCI Versus CABG?
Cardiac catheterization
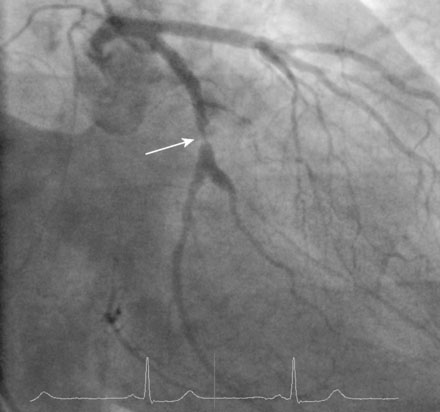
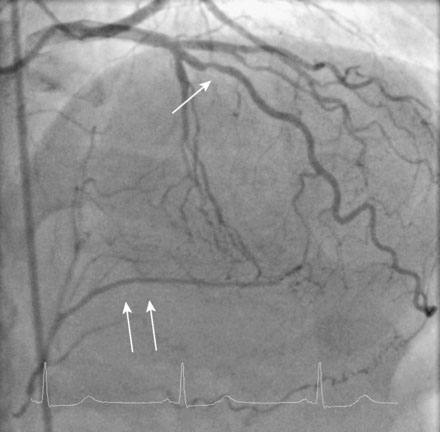
Ventriculography demonstrated moderate hypokinesis of the inferior wall, but global function was normal with an estimated ejection fraction of 60%. The right coronary artery was completely occluded and the duration of the occlusion could not be precisely determined (Figure 36-1 and Video 36-1). In the left coronary artery, a severe stenosis was identified in the midsegment of the left circumflex artery (Figure 36-2 and Video 36-2), and a stenosis of at least moderate severity was seen in the midsegment of the left anterior descending artery (Figure 36-3 and Video 36-3). The presence of well-developed left to right collaterals and the duration of symptoms suggested that the right coronary artery was chronically occluded and at least 3 months old.
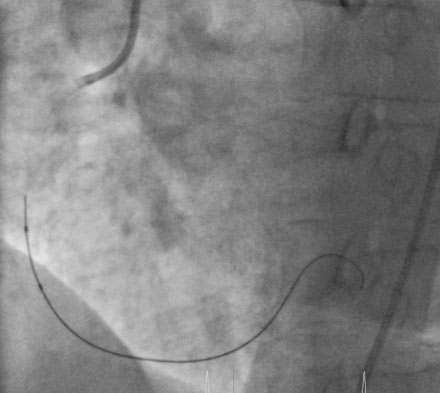
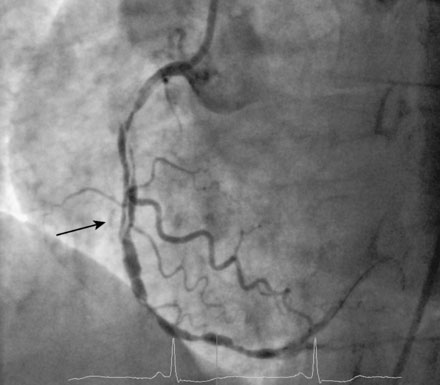
With this strategy in mind, the operator began with the right coronary artery. Procedural anticoagulation was accomplished with bivalirudin; the patient had already received pretreatment with 300 mg of clopidogrel the night before the procedure. After engaging a 6 French right Judkins guide catheter, the operator loaded a stiff-tipped 0.014 inch guidewire (Miracle Bros, 3, Asahi) into the lumen of a 2.5 mm diameter by 15 mm long, “over-the-wire,” compliant balloon catheter. The stiff-tipped guidewire easily crossed the occlusion and was advanced into the distal right coronary artery (Figure 36-4). The “over-the-wire” balloon was advanced distally and the stiff-tipped wire was removed and replaced by a floppy-tipped guidewire. Patency was restored after performing balloon angioplasty with the 2.5 mm balloon; however, the artery appeared diffusely diseased distally with an extensive dissection in the midsection (Figure 36-5 and Video 36-4). Multiple everolimus-eluting stents were placed, ranging in diameter from 2.5 mm distally to 3.5 mm proximally, covering 98 mm of length. The proximal and midsegments were postdilated with a 4.0 mm noncompliant balloon and an excellent final angiographic result was obtained (Figure 36-6 and Video 36-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree